Introduction to the recent 2017 classification system
Since the introduction of the World Workshop 1999 classification, tremendous research has been done in both basic and clinical fields in periodontics. With the evolution of new evidence, there was a need to re-define various periodontal and peri-implant diseases and conditions. With this intention, the American Academy of Periodontology (AAP) and European Federation of Periodontology (EFP) in early 2015 planned for a world workshop which was finally held on November 9 to 11, 2017 in Chicago. The main purpose of this workshop was not only to classify various diseases and conditions but also to provide a structure for treatment planning and for monitoring the patient response to therapy. Because dental implant therapy has become an integral part of Periodontics, the new classification specifically included classification for peri-implant diseases and conditions. In the following discussion, we shall discuss in detail this classification.
Basic outline of classification
Significant changes have been made in the new classification when we compare it with the World Workshop 1999 classification. Let us first try to understand the basic outline of the classification. The new classification classifies periodontal and peri-implant diseases and condition as follows,
Periodontal diseases and conditions:
Periodontal health, gingival diseases, and conditions,
- Periodontal health and gingival health.
- Gingivitis: Dental biofilm-induced.
- Gingival diseases: Non-dental biofilm-induced.
Periodontitis,
- Necrotizing periodontal diseases.
- Periodontitis.
- Periodontitis as a manifestation of systemic diseases.
Other conditions affecting the periodontium,
- Systemic diseases or conditions affecting the periodontal supporting tissues.
- Periodontal abscess and endodontic-periodontal lesions.
- Mucogingival deformities and conditions.
- Traumatic occlusal forces.
- Tooth and prosthesis-related factors.
Peri-implant diseases and conditions:
- Peri-implant health.
- Peri-implant mucositis.
- Peri-implantitis.
- Peri-implant soft and hard tissue deficiencies.
Let us now discuss each point of the above classification in detail,
Periodontal health, gingival diseases & conditions
Periodontal health and gingival health:
Periodontal and gingival health refers to the absence of inflammation associated with gingivitis or periodontitis. It can be assessed both histologically and clinically. In this classification, gingival and periodontal health has been further classified as 44,
- Clinical gingival health on intact periodontium.
- Clinical gingival health on reduced periodontium.
- Stable periodontitis patient.
- Non-periodontitis patient.
The most predictable sign of inflammation is bleeding on probing. A standard probing pressure of 0.25 N should be used during probing and an absence of bleeding on probing at this pressure indicates periodontal health, with a negative predictive value of 98% to 99% 45. Periodontal health can be achieved before the commencement of the disease in intact periodontium and following the treatment of the disease in reduced periodontium. Four levels of periodontal health have been proposed under this classification which depend upon whether the periodontium has normal attachment and bonenlevel or reduced support, as well as the ability to control modifying factors and relative treatment outcomes 44. These are,
- Pristine periodontal health: It has been defined as the total absence of clinical inflammation and physiological immune surveillance on a periodontium with normal support. In pristine periodontal health, there is no attachment or bone loss. However, this situation is unlikely to be observed clinically.
- Clinical periodontal health: This type of periodontal health most likely describes periodontal health in the normal periodontium. It is characterized by an absence or minimal levels of clinical inflammation in a periodontium with normal support. As compared to pristine periodontal health, clinical periodontal health is characterized by physiological immune surveillance involving levels of biological and inflammatory markers compatible with homeostasis.
- Periodontal disease stability: It describes the periodontal status in reduced (periodontitis-affected) periodontium and is characterized by minimal inflammation and optimal therapeutic response, with control of modifiable risk factors. It is the most desirable outcome of periodontal therapy.
- Periodontal disease remission/ control: It is defined as a period in the course of disease during which treatment has resulted in a reduction (although not total resolution) of inflammation and some improvement in periodontal pocket depth and attachment levels, but not optimal control of local or systemic contributing factors. It should be noted here that it is differentiated from periodontal disease stability by the fact that, it is not possible to fully control the modifying and predisposing factors such as smoking or diabetes.
Case definition for periodontal health:
As already stated, checking bleeding on probing with a controlled (0.25 N) force is a very predictable method of assessing gingival inflammation. The probing should be done at six sites (mesiobuccal, buccal, distobuccal, mesiolingual, lingual, distolingual) on all teeth present.
Definition of gingival health for a case of gingival health on an intact and a reduced periodontium for epidemiological purposes:
For an intact periodontium and a reduced and stable periodontium, gingival health is defined as <10% bleeding sites with probing depths ≤3 mm.
Definition of gingival health for a case of gingival health on an intact and a reduced periodontium for clinical practice:
Gingival health on an intact periodontium and a reduced and stable periodontium, gingival health is defined as <10% bleeding sites 46, 47 with probing depths ≤3 mm. This definition is the same as that given for epidemiological purposes. Gingival health on a reduced periodontium in stable periodontitis patient is characterized by successful treatment through control of local and systemic risk factors, resulting in minimal (< 10% of sites) bleeding on probing, no probing depths of ……… Contents available in the book……….. Contents available in the book……….. Contents available in the book…………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Gingival diseases:
The World workshop, 2017 has classified the gingival diseases into two broad categories,
- Dental plaque biofilm-induced gingivitis.
- Non-dental plaque-induced gingival diseases.
Dental plaque biofilm-induced gingivitis
The World Workshop, 2017 48 defines gingivitis at the site level as “an inflammatory lesion resulting from interactions between the dental plaque biofilm and the host’s immune-inflammatory response, which remains contained within the gingiva and does not extend to the periodontal attachment (cementum, periodontal ligament and alveolar bone). Such inflammation remains confined to the gingiva and does not extend beyond the mucogingival junction and is reversible by reducing levels of dental plaque at and apical to the gingival margin”.
The symptoms observed by the patients during gingivitis include bleeding from gums while tooth brushing, blood in saliva, swollen gums and bad breath. The clinical signs of gingivitis include erythema, edema, bleeding, tenderness, and enlargement. It should be noted here that dental biofilm is the basic etiology for plaque-induced gingivitis; however, many other systemic factors may act as modifying factors for plaque-induced gingivitis. Following classification of plaque induced gingivitis and modifying factors has been given in the present classification,
A) Associated with bacterial dental biofilm only
B) Potential modifying factors of plaque-induced gingivitis
1) Systemic conditions
a) Sex steroid hormones
1) Puberty
2) Menstrual cycle
3) Pregnancy
4) Oral contraceptives
b) Hyperglycemia
c) Leukemia
d) Smoking
e) Malnutrition
2) Oral factors enhancing plaque accumulation
a) Prominent subgingival restoration margins
b) Hyposalivation
C) Drug-influenced gingival enlargements.
It is important to note here that terms like “menstrual cycle-associated gingivitis,” “oral contraceptive-associated gingivitis,” and “ascorbic acid-associated gingivitis” were removed from the classification system. The reason suggested for the elimination of these terminologies was, although, scientific evidence suggests that in all the abovestated conditions gingival inflammation increases; however, the clinical signs of gingival inflammation that do occur in these conditions may be statistically significant but are not clinically significant. Therefore, these inflammatory changes are not clinically evident to the dentist. In other words, we can say that it is not possible clinically to distinguish between the plaque-induced gingivitis and gingival inflammation caused by the above conditions. Hence, these terms were eliminated.
Gingivitis may occur both in the intact or reduced periodontium. So, in the present classification, dental plaque biofilm-induced gingivitis has been further classified as 48:
- Gingivitis on an intact periodontium.
- Gingivitis on a reduced periodontium in a non-periodontitis patient (e.g., recession, crown lengthening).
- Gingival inflammation on a reduced periodontium in a successfully treated periodontitis patient (Note that recurrent periodontitis cannot be ruled out in this case).
Case definition for dental plaque biofilm-induced gingivitis on intact and reduced periodontium for epidemiological purposes
The consensus report defines the gingivitis on an intact and reduced periodontium for epidemiological purposes as ≥10% bleeding sites in a patient without a history of periodontitis with probing depths ≤3 mm. Localized gingivitis is defined as 10%-30% bleeding sites; generalized gingivitis is defined as > 30% bleeding sites. It has been clarified that for epidemiological purposes, a periodontitis case cannot simultaneously be defined as a gingivitis case, that is, a patient with a history of periodontitis, with gingival inflammation is still a periodontitis case.
Case definition of gingivitis in an intact periodontium
| Localized gingivitis | Generalized gingivitis | |
|---|---|---|
| Probing attachment loss | No | No |
| Radiographic bone loss | No | No |
| BOP score | ≥10%, ≤30% | >30% |
Case definition of gingivitis in a reduced periodontium without history of periodontitis
| Localized gingivitis | Generalized gingivitis | |
|---|---|---|
| Probing attachment loss | Yes | Yes |
| Radiographic bone loss | Possible | Possible |
| Probing depth (all sites) | ≤3 mm | ≤3 mm |
| BOP score | ≥10%, ≤30% | >30% |
Case definition for a patient with dental plaque-induced gingivitis on an intact and a reduced periodontium for clinical practice
In clinical practice, the case definition for a patient with dental plaque-induced gingivitis on an intact and a reduced periodontium without any history of periodontitis is similar to as stated above.
The consensus report defines gingivitis in a stable periodontitis patient as gingival inflammation at specific sites with probing depths ……. Contents available in the book……….. Contents available in the book……….. Contents available in the book…………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
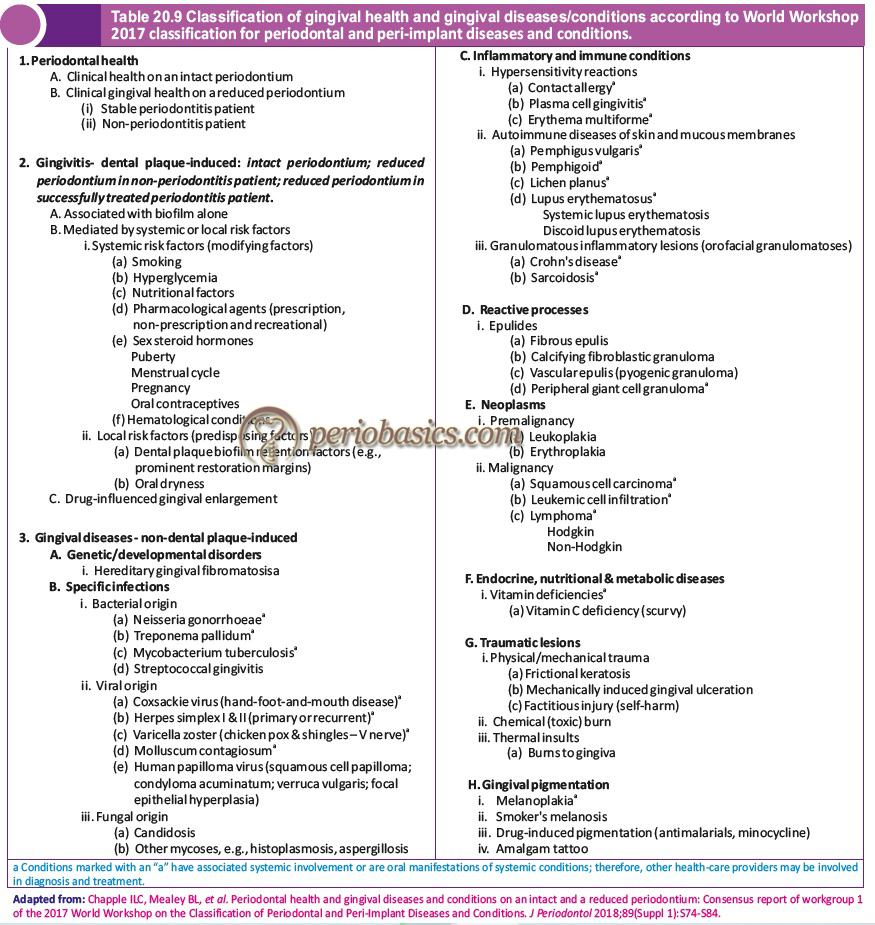
Non-dental plaque-induced gingival diseases
Presently, there is strong evidence suggesting the interrelationship between oral and systemic diseases. Various systemic diseases may have their oral manifestations and various oral diseases may have an impact on systemic health. So, it is essential for health care providers to understand this interrelationship and incorporate appropriate referrals for the overall treatment of the patient. The category of non-dental plaque-induced gingival diseases includes that are not caused by plaque and usually do not resolve following plaque removal. These gingival lesions may be the oral manifestations of certain systemic diseases. The non-dental-biofilm gingival diseases have been classified into eight categories in this classification,
- Genetic/developmental disorders.
- Specific infections.
- Inflammatory and immune conditions.
- Reactive processes.
- Neoplasms.
- Endocrine, nutritional and metabolic diseases.
- Traumatic lesions.
- Gingival pigmentation.
The following table enumerates the details of the non-dental plaque-induced gingival diseases. Because the aim of the present classification system is to provide the right care at the right time, conditions marked with ‘a’ have associated systemic involvement or are oral manifestations of systemic conditions. So, other health care providers may be involved in diagnosis and treatment. This kind of patient-centered care has been referred to as “precision dental medicine (PDM)”.
Forms of Periodontitis
Periodontitis is the inflammation of periodontium characterized by clinical attachment loss (CAL). In the present classification system, on the basis of pathophysiology, three clearly different forms of periodontitis have been identified,
- Necrotizing periodontal diseases.
- Periodontitis.
- Periodontitis as a manifestation of systemic diseases.
The Workshop proposed the identification of the above three forms of periodontitis by following three steps,
- Identification of a patient as a periodontitis case,
- Identification of the specific type of periodontitis, &
- Description of the clinical presentation and other elements that affect clinical management, prognosis, and potentially broader influences on both oral and systemic health.
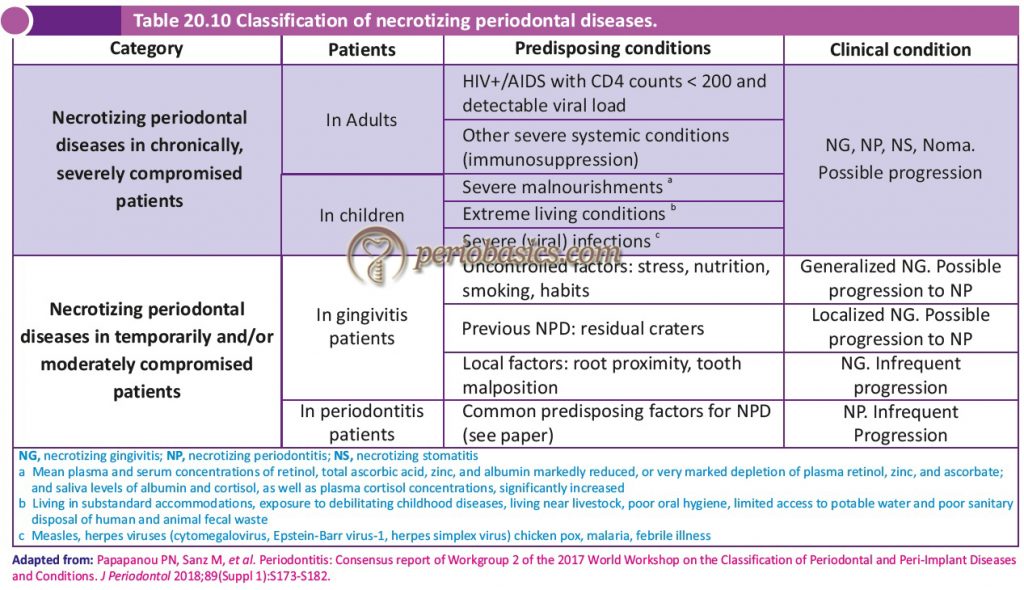
Necrotizing periodontal diseases (NPD)
These are infectious conditions characterized by necrosis of tissues of the periodontium. The predisposing factors, including a compromised immune system, are critical in its pathogenesis. In the 1999 classification system, the necrotizing periodontal disease category included two conditions, necrotizing ulcerative gingivitis (NUG) and necrotizing ulcerative periodontitis (NUP) which represent different stages of the same disease, because they have similar etiology, clinical characteristics, and treatment. However, it was realized that this classification did not consider a wide variation among prevalence, risk of progression, and the extent and severity of NPD among patients with different predisposing conditions. For example, in underdeveloped countries where malnutrition is prevalent in children, and also in HIV/AIDS patients, the NPD are severe and even life-threatening conditions. On the other hand, in developed countries, NPD in smokers and stressed adult patients represents a relevant but normally non-threatening condition.
Thus, in 2017 World Worksop classification the NPD were classified considering these factors 52 (Table 20.10). Three types of necrotizing periodontal diseases have been described in this classification,
- Necrotizing gingivitis.
- Necrotizing periodontitis.
- Necrotizing stomatitis.
Periodontitis
2017, World workshop defines periodontitis as a chronic multifactorial inflammatory disease associated with dysbiotic plaque biofilms and characterized by progressive destruction of the tooth-supporting apparatus 52. It is characterized by loss of periodontal tissue support, manifested through clinical attachment loss (CAL) and radiographically assessed alveolar bone loss, presence of periodontal pocketing and gingival bleeding.
Before we go ahead with the discussion on 2017 classification of periodontitis, it is essential to discuss the 1999 classification of periodontitis. The 1999 classification described four different forms of periodontitis,
- Necrotizing periodontitis.
- Chronic periodontitis.
- Aggressive periodontitis.
- Periodontitis as a manifestation of systemic diseases.
The necrotizing periodontitis is characterized by unique pathophysiology and presentation and was classified differently from more common forms of periodontitis, chronic and aggressive periodontitis. Further, in the 1999 classification, specific features were identified to classify a case as an aggressive periodontitis case which consisted of major and minor criteria to define the case. The distribution features were used to differentiate the localized and generalized forms of periodontitis. The periodontitis cases that did not satisfy the criteria laid down for aggressive form were referred to as chronic periodontitis cases. The main idea behind differentiating the aggressive and chronic forms of periodontitis was to identify more problematic cases which required special efforts to control the disease progression. The fourth category of periodontitis in the 1999 classification was, ‘Periodontitis as a manifestation of systemic diseases’. It included the systemic diseases which had periodontitis as one of their clinical features.
With immense basic and clinical research in the field of periodontics from 1999 till 2017, many aspects of the etiopathogenesis of periodontal diseases became more clear. In the light of present evidence, the following interpretations were made during the 2017 World Workshop,
- There is no clear evidence that differentiates the chronic and aggressive forms of periodontitis on the basis of specific pathophysiology. Further, there is no clear evidence that provides guidelines for different interventions in chronic and aggressive cases.
- There is little evidence in support of aggressive and chronic periodontitis being two different diseases. However, there is evidence in favor of multiple factors, interaction among which influences the clinically observable disease outcomes (phenotypes) at the individual level.
- On a population basis, the mean rates of periodontitis progression are consistent across all observed populations throughout the world.
- There is evidence in favor of the existence of the specific segments of the population that exhibits different levels of disease progression, as indicated by greater severity of clinical attachment loss (CAL) in subsets of each age cohort relative to the majority of individuals in the age cohort.
- A classification system that is entirely based on the severity of the disease fails to identify the importance of other dimensions of an individual’s disease consisting of the complexities of the case that may influence the approach towards delivering periodontal therapy, risk factors influencing the treatment outcome and level of knowledge and training required to manage the individual cases.
Case definition for Periodontitis
The World Workshop 2017, adopted the following criteria for defining a case of periodontitis,
- Interdental CAL is ‘detectable’ at ≥2 non-adjacent teeth, or
- Buccal or oral CAL ≥3 mm with pocketing >3 mm is detectable at ≥2 teeth.
Further, it was clarified that the observed CAL cannot be ascribed to non-periodontal causes such as,
- Gingival recession of traumatic origin;
- Dental caries extending in the cervical area of the tooth;
- The presence of CAL on the distal aspect of a second molar and associated with malposition or extraction of a third molar,
- An endodontic lesion draining through the marginal periodontium; and
- The occurrence of a vertical root fracture.
Staging and grading system of periodontitis
Staging of periodontitis
The first goal of staging a periodontitis patient is to classify the patient on the basis of severity and extent of disease by measuring the extent of destroyed and damaged tissue attributable to periodontitis. The second goal of staging the periodontitis patient is to assess specific factors that may determine the complexity of controlling current disease and managing long-term function and esthetics of the patient’s dentition. Thus, the stage of periodontitis is decided by estimating the severity and complexity of the disease. In the present classification system, following four stages of periodontitis have been suggested,
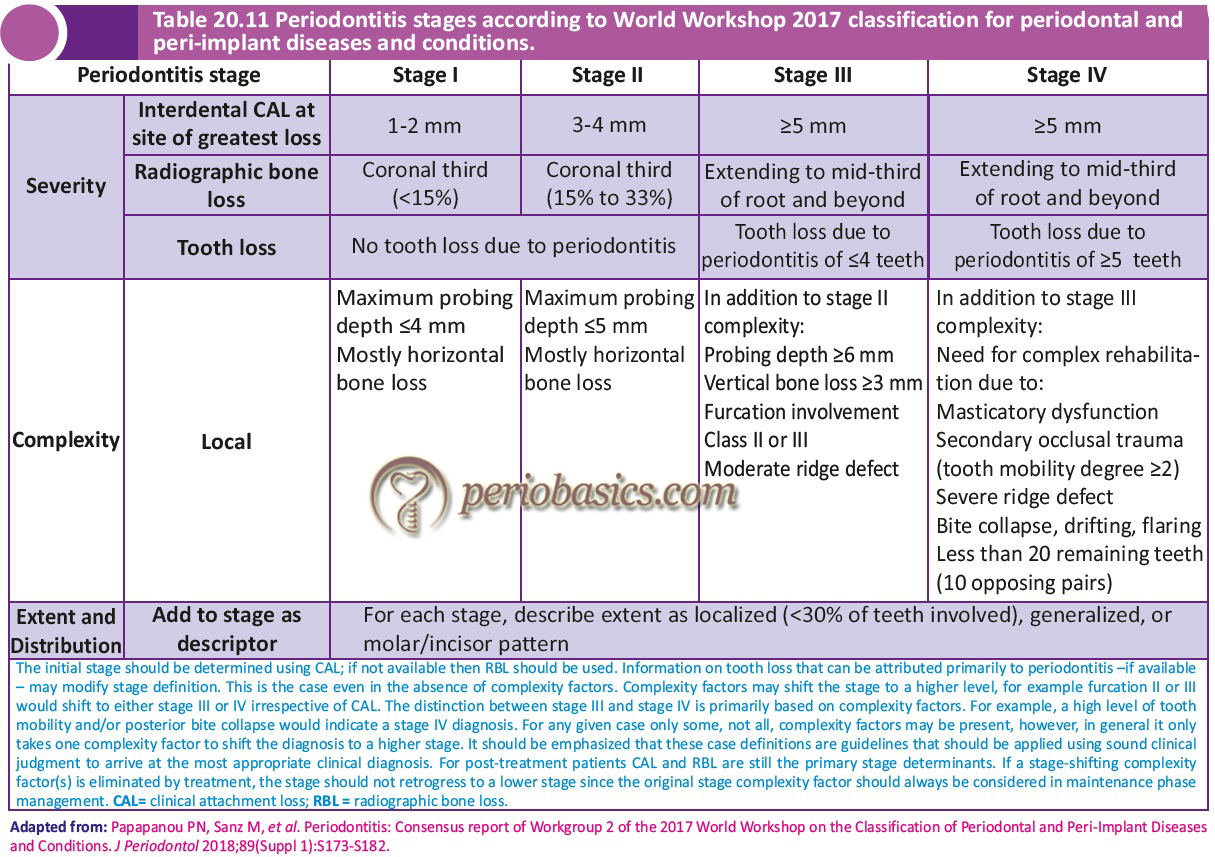
Stage I Periodontitis:
This stage is characterized by initial periodontitis, that is, the transition of gingivitis to periodontitis. This stage represents the early attachment loss. In this stage, the interdental clinical attachment loss (CAL) at the site of greatest attachment loss is 1-2 mm. The radiographic bone loss is <15% and there is no tooth loss due to periodontitis. All these factors come under the severity of the disease. To estimate the complexity, the probing depths and pattern of bone loss are calculated. Stage I periodontitis is characterized by probing depths ≤4 mm with mostly horizontal bone loss.
Stage II Periodontitis:
It represents established periodontitis, where carefully done periodontal examination identifies damage to the supporting periodontal tissues. The CAL in Stage II periodontitis is 3-4 mm and radiographic bone loss is between 15% to 33%. There should be no tooth loss due to periodontitis. In the determination of the complexity, the probing depths are ≤5 mm with mostly horizontal bone loss.
Stage III Periodontitis:
In this stage, there is significant damage to the supporting periodontal tissues. The CAL is ≥5 mm and the bone loss extends to the middle third of the root and beyond. Along with this, tooth loss due to periodontitis is ≤4 teeth. As in this stage, there is considerable damage to the periodontium, there are multiple complexing factors which should be carefully examined. These include (in addition to stage II complexity), probing depth ≥6 mm, vertical bone loss ≥3 mm, furcation involvement Class II or III and moderate ridge defect. In this stage, in spite of the possibility of tooth loss, the masticatory function is preserved and the treatment of periodontitis does not require complex rehabilitation of function.
Stage IV Periodontitis:
This stage is characterized by ………. Contents available in the book……….. Contents available in the book……….. Contents available in the book…………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
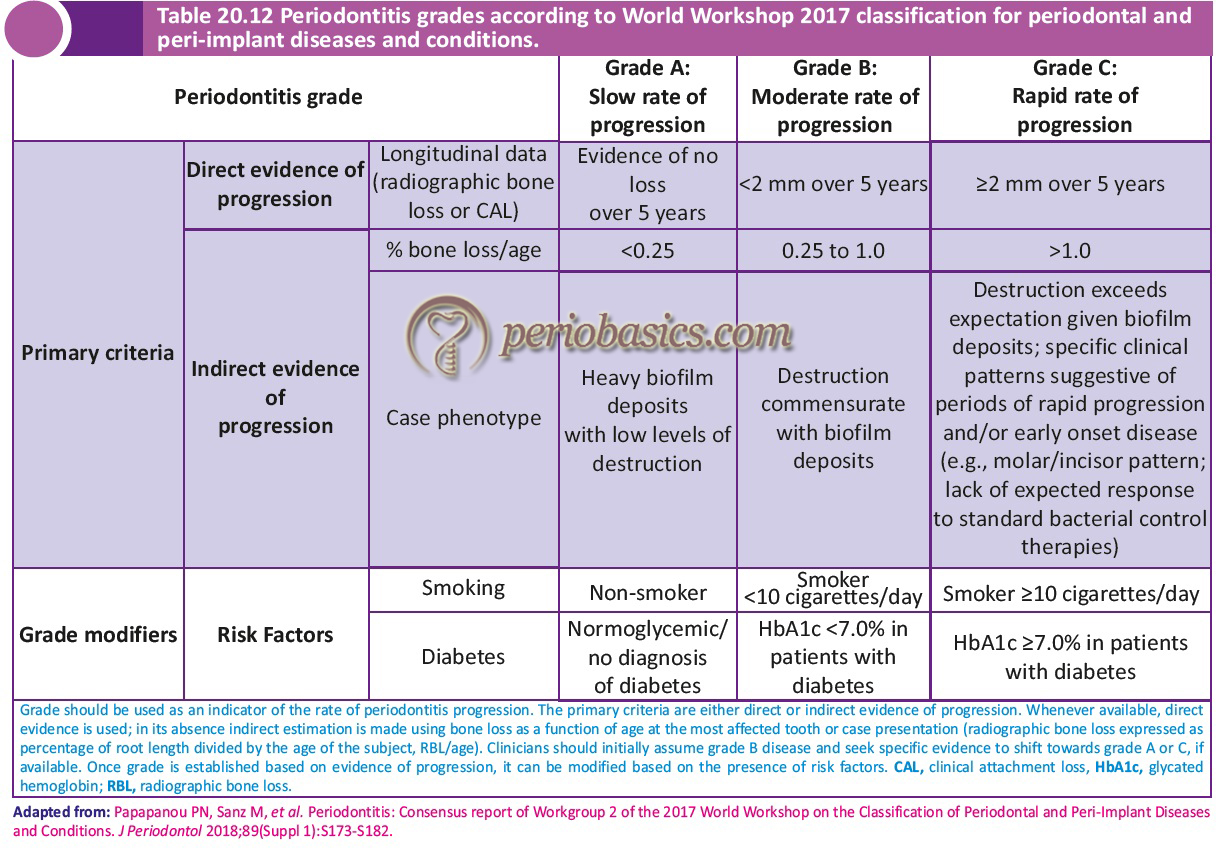
Grading of periodontitis
The first goal of grading a periodontitis patient is to estimate future risk of periodontitis progression and responsiveness to standard therapeutic principles, to guide the intensity of therapy and monitoring. The second goal is to estimate the potential health impact of periodontitis on systemic disease and the reverse, to guide systemic monitoring and co-therapy with medical colleagues. The rate of disease progression can be assessed by direct evidence or indirect evidence. The direct evidence can be obtained from … Contents available in the book……….. Contents available in the book……….. Contents available in the book…………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book…………..
To begin with, the clinician should assume Grade B or moderate rate of disease progression in every case. Then, by going into the details of the case history, the presence of risk factors that have participated in the disease progression are identified. If one or more risk factors are present, they shift the grade score to a higher value, independently of the primary criterion represented by the rate of progression. For example, if a patient has moderate attachment loss (Stage II) and a moderate rate of disease progression (Grade B); however, he/she has poorly controlled Type II diabetes mellitus, then the grade of disease progression will shift to Grade C (rapid progression).
Periodontitis as a manifestation of systemic diseases
The 2017 classification system for periodontal diseases and conditions also includes systemic diseases and conditions that affect the periodontal supporting structures. Certain rare disorders like Papillon Lefever syndrome have severe periodontitis as one of their early clinical features. Such conditions are grouped as “Periodontitis as a Manifestation of Systemic Disease”, and their classification should be based on the primary systemic disease 53. With regard to periodontitis as a direct manifestation of systemic disease, the recommendation is to follow the classification of the primary disease, according to the respective International Statistical Classification of Diseases and Related Health Problems (ICD) codes.
It should be noted here that there are other systemic diseases such as neoplasms which may affect the periodontal apparatus independent of the dental plaque-induced periodontitis. According to the present classification, such clinical findings should also be classified based on the primary systemic disease and be grouped as “Systemic Diseases or Conditions Affecting the Periodontal Supporting Tissues”.
Other conditions affecting periodontium
Systemic diseases or conditions affecting the periodontal supporting tissues
As stated above, this category includes the systemic diseases which may affect the periodontal apparatus independent of the dental plaque-induced periodontitis. Uncommon or rare conditions such as neoplastic lesions may affect the periodontal apparatus independent of dental plaque biofilm induced periodontitis. As per the new classification system, the classification of these conditions should be based on the primary systemic disease, according to the international statistical classification of diseases and related health problems (ICD codes).

Common systemic diseases such as diabetes mellitus are important modifiers of the course of periodontitis. However, diabetes-associated periodontitis should not be regarded as a distinct diagnosis because diabetes is now included in the new clinical classification of periodontitis as a descriptor in the grading process. Similarly, smoking, which adversely affects the periodontium has also been included as a descriptor in the grading process.
Periodontal abscess and endodontic-periodontal lesions
Periodontal abscess
As per the 2017 World workshop 52, the periodontal abscess has been defined as a localized accumulation of pus located within the gingival wall of the periodontal pocket/sulcus, resulting in a significant tissue breakdown. In the 1999 classification system, the abscesses of the periodontium were classified as,
- Gingival abscess,
- Periodontal abscess,
- Pericoronal abscess, and
- Periapical abscess.
The drawbacks in this classification were: a) The distinction between gingival and periodontal abscess was not clear, b) The periodontal abscess was classified as acute and chronic; however, an abscess, by definition, is an acute lesion; and c) the inclusion of pericoronitis and periapical abscesses in the classification together with periodontal abscess might not be appropriate. Hence, in the 2017 classification system, the periodontal abscesses were classified on the basis of etiological factors involved.

Endodontic-periodontal lesions
According to World Workshop 2017, endo-periodontal lesions are defined as a pathologic communication between the pulpal and periodontal tissues at a given tooth that may occur in an acute or a chronic form. Clinically, endo-periodontal lesions are characterized by deep periodontal pockets extending to the root apex and/or negative/altered response to pulp vitality tests. Other signs and symptoms may include tenderness of percussion, purulent suppuration, presence of sinus tract/fistula, tooth mobility and radiographic evidence of bone loss in the apical or furcation area. The iatrogenic causes for endo-periodontal lesions include perforation during root canal treatment, fracture/cracking, or external root resorption.
In the 1999 classification system, the endo-periodontal lesions were classified for the first time under section VII Periodontitis Associated with Endodontic Lesion, as a single category entitled “Combined Periodontal-Endodontic Lesions.” The advantage of classifying endo-periodontal lesions under a single category was that it reflected the current clinical condition of the lesion. However, the problems associated with this classification were,
- All kinds of endo-periodontal lesions were classified under a single category which is not ideal because these lesions may occur in subjects with or without periodontitis, and
- A single category for endo-periodontal lesions was too generic and is not able to help the clinicians to make the most effective treatment choice for a particular endo-periodontal lesion.
So, there was a need to classify the endo-periodontal lesions according to the signs and symptoms detected at the time of diagnosis because they had a direct impact on the treatment plan. Table 20.15 describes the World Workshop 2017 classification for the endo-periodontal lesions.
Mucogingival deformities and conditions
The most common mucogingival deformities observed are recession and lack of keratinized tissue. In the World Workshop 2017 classification, a treatment-oriented classification of mucogingival deformities has been proposed. Periodontal biotype plays a very important role in the occurrence and the treatment of mucogingival deformities. The periodontal biotype has been referred to as “gingival” or “periodontal” “biotype”, “morphotype” or “phenotype” by various authors. In the consensus report the term “periodontal biotype” was replaced by “periodontal phenotype”. Term ‘Biotype’ refers to a group of organs having the same specific genotype; whereas, term ‘Phenotype’ refers to the appearance of an organ-based on a multifactorial combination of genetic traits and environmental factors (its expression includes the biotype).
Three types of periodontal phenotypes have been described,
Thin scalloped: This type of periodontal phenotype is commonly associated with slender triangular crown, subtle cervical convexity, interproximal contacts close to the incisal edge and a narrow zone of keratinized tissue. The gingiva is thin and delicate. The alveolar bone is relatively thin.
Thick scalloped: This type of periodontal phenotype demonstrates thick fibrotic gingiva, slender teeth, narrow zone of keratinized tissue, and pronounced gingival scalloping.
Thick flat: This type of periodontal phenotype is usually associated with more square-shaped tooth crowns, pronounced cervical convexity, large interproximal contact located more apically, a broad zone of keratinized tissue, thick, fibrotic gingiva, and a comparatively thick alveolar bone.
A thin periodontal phenotype (< 1 mm) is associated with less probability for complete root coverage when applying advanced flaps. Thus, the periodontal biotype plays an important role during the recession coverage.
Considering the drawbacks of Miller’s classification (1985) 54 of gingival recession, the classification given by Cairo et al. (2011) 55 was used in the present classification.
Classification of gingival recession by Cairo et al. (2011)55:
Recession Type 1 (RT1): Gingival recession with no loss of interproximal attachment. Interproximal CEJ is clinically not detectable at both mesial and distal aspects of the tooth.
Recession Type 2 (RT2): Gingival recession associated with loss of interproximal attachment. The amount of interproximal attachment loss (measured from the interproximal CEJ to the depth of the interproximal sulcus/pocket) is less than or equal to the buccal attachment loss (measured from the buccal CEJ to the apical end of the buccal sulcus/pocket).
Recession Type 3 (RT3): Gingival recession associated with loss of interproximal attachment. The amount of interproximal attachment loss (measured from the interproximal CEJ to the apical end of the sulcus/pocket) is greater than the buccal attachment loss (measured from the buccal CEJ to the apical end of the buccal sulcus/pocket).
It is a treatment-oriented classification. In Cairo RT1 (equivalent to Miller’s Class I and Class II) 100% root coverage can be anticipated. In Cairo RT2 (equivalent to Miller’s Class III), as indicated by some recent randomized controlled trials, 100% root coverage is predictable within a limit of interdental CAL loss. In Cairo RT3 (equivalent to Miller class IV) full root coverage is not achievable 55, 56.
To facilitate the treatment-oriented classification of these deformities, the 2017 World Workshop suggested a diagnostic approach to classify gingival phenotype, gingival recession, and associated cervical lesions. The workshop explained four situations (case a-d) based on the assessment of gingival biotype, gingival thickness, recession depth, and keratinized tissue width either in full oral cavity or in single sites.
Absence of gingival recession:
Case a: Thick gingival biotype without gingival recession:
In this case, the gingival recession can be prevented through oral hygiene instructions and monitoring of the case.
Case b: Thin gingival biotype without gingival recession:
These cases are at an increased risk of future development of gingival recession. Careful professional monitoring is required in such cases. In cases where severe thin gingival biotype is present mucogingival surgery in high-risk sites could be considered to prevent future mucogingival damage.
Presence of gingival recession:
The recession should be classified based on the interdental clinical attachment level (Cairo RT1-RT3). Along with this, other factors, including recession depth, gingival thickness, keratinized tissue width, and root surface condition should also be considered. Factors such as tooth position, cervical tooth wear and the number of adjacent recessions should also be considered.
Case c: In the recession cases a conservative approach should be employed by charting the periodontal and root surface lesions and monitoring them overtime for deterioration. The parameters to be recorded include distance between the cementoenamel junction and free gingival margin, and distance between the mucogingival junction and the free gingival margin. It is done to determine the amount of keratinized tissue present. If the severity of the periodontal or dental lesions increases appropriate treatment should be done (Case d).
Case d: These recession cases (especially thin biotype cases) are treated with appropriate mucogingival surgical procedure based on the patient concern or complaint in terms of esthetics and/or dentinal hypersensitivity and due to the presence of cervical caries or non-carious cervical lesions (NCCL). The treatment is especially indicated in cases in which other treatments such as orthodontic treatment, restorative treatment (restorations with intrasulcular margins) or implant therapy are planned.
Traumatic occlusal forces
The World Workshop 2017 has defined traumatic occlusal force as any occlusal force resulting in injury of the teeth and/or the periodontal attachment apparatus. These forces are clinically indicated by one or more of the following,
- Tooth mobility,
- Tooth migration,
- Fremitus,
- Thermal sensitivity,
- Excessive occlusal wear,
- Discomfort/pain on chewing,
- Fractured teeth,
- Radiographically, widened periodontal ligament space,
- Hypercementosis,
- Root resorption.
Occlusal trauma is a lesion in the periodontal ligament, cementum and adjacent bone caused by traumatic occlusal forces. It is a histological finding and can be clinically identified by one or more above stated clinical findings.
The World Workshop 2017 classified the traumatic occlusal forces on the periodontium into following classes,
- Primary trauma from occlusion.
- Secondary trauma from occlusion.
- Orthodontic forces.
Tooth and prosthesis-related factors
There are many conditions related to teeth and prosthesis that may predispose to the diseases of the periodontium. Tooth related factors such as cervical enamel projections (CEPs), enamel pearls and developmental grooves are developmental variations that act as predisposing factors for the development of periodontitis. Tooth position, root proximity, and open contacts are additional factors that may facilitate the development of periodontitis. For example, crossbite, malalignment, and crowding of teeth are associated with increased accumulation of plaque thereby facilitating the progression of periodontal diseases. Tooth and root fractures do not initiate gingivitis or periodontitis, unless the surface characteristics of the fracture area predispose to greater plaque retention.
The most important factor that has to be considered during the placement of a dental prosthesis (crowns and bridges) is ... Contents available in the book……….. Contents available in the book……….. Contents available in the book…………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Peri-implant diseases and conditions
Peri-implant health
Peri-implant health is characterized by absence of erythema, bleeding on probing, swelling and suppuration. For day to day clinical practice and teaching situations, the world workshop proposed the following characteristics features of peri-implant health 58,
- Absence of clinical signs of inflammation.
- Absence of bleeding and/or suppuration on gentle probing.
- No increase in probing depth compared to previous examinations.
- Absence of bone loss beyond crestal bone level changes resulting from initial bone remodeling.
Peri-implant mucositis
This condition is characterized by bleeding on gentle probing. Erythema, swelling and/or suppuration may also be present. For day to day clinical practice and teaching situations, the world workshop proposed following characteristic features of peri-implant mucositis 58,
- Presence of bleeding and/or suppuration on gentle probing with or without increased probing depth compared to previous examinations.
- Absence of bone loss beyond crestal bone level changes resulting from initial bone remodeling.
It should be noted here that the in peri-implant mucositis, the clinical signs of inflammation may vary and this condition can exist around the implants with varying levels of bone support.
Peri-implantitis
It is a dental biofilm-associated inflammatory condition characterized by inflammation in the peri-implant mucosa and subsequent progressive loss of supporting bone. For day to day clinical practice and teaching situations, the world workshop proposed following characteristic features of peri-implant mucositis 58,
- Presence of bleeding and/or suppuration on gentle probing.
- Increased probing depth compared to previous examinations.
- Presence of bone loss beyond crestal bone level changes resulting from initial bone remodeling.
The above-stated observations require data from the baseline and subsequent examinations in the past. In the absence of previous examination data, the following criteria are used to diagnose peri-implantitis,
- Presence of bleeding and/or suppuration on gentle probing.
- Probing depths of ≥6 mm.
- Bone levels ≥3 mm apical of the most coronal portion of the intraosseous part of the implant.
Peri-implant soft and hard tissue deficiencies
Various factors may result in soft and hard tissue deficiencies around implants. Soft issue deficiency (recession) around implants may result from malpositioning of implants, lack of buccal bone, thin soft tissue, lack of keratinized tissue, the status of attachment of the adjacent teeth and surgical trauma. The soft tissue deficiency in the interdental area is dependent on the level of the periodontal tissues on the teeth adjacent to the implants. The height of the papilla between implants is determined by the bone crest between the implants. It is debatable whether the presence/absence of keratinized mucosa plays a role in the long-term maintenance of periimplant health. However, the 2017 World Workshop proposes that keratinized mucosa may have advantages regarding patient comfort and ease of plaque removal 58.
After tooth extraction, due to healing and remodeling of the bone, the alveolar ridge shows hard and soft tissue deficiencies. More than the usual bone loss occurs in cases with loss of periodontal support, endodontic infections, traumatic extractions, injury, pneumatization of the maxillary sinus, etc. Various surgical procedures are required to achieve the appropriate bone volume required to place the implant.
Procedural steps in diagnosing a patient
Step 1:
When seeing a patient for the first time, the first step in making a diagnosis is to decide whether the patient has healthy periodontium or has generalized/ localized gingivitis or he/she is a suspected periodontitis patient. Firstly, we should ask for a full-mouth radiograph of adequate quality. If the radiograph is available, we should check for bone loss. If bone loss is present, the patient is suspected to have periodontitis. If the radiograph is not available, we should clinically explore the patient and check for interdental clinical attachment loss (CAL). If CAL is not present, we check for buccal recessions with probing pocket depths (PPD) greater than 3 mm. If recessions are present, the patient is suspected to have periodontitis. If there are no buccal PPD greater than 3 mm, we check for bleeding on probing. If the bleeding on probing is present at > 10% sites, the patient is diagnosed with gingivitis. If the bleeding on probing is present at < 10% sites, the patient is diagnosed with periodontal health (Figure 20.1). If interdental CAL or buccal PPD greater than 3 mm is present, the patient is suspected to have periodontitis and we move to the second step.
Step 2:
In this step, we analyze a suspected periodontitis patient. First of all, we need to decide whether the CAL is present due to local factors such as endo-perio lesions, vertical root fractures, caries, restorations, or impacted third molars. If not, then we should find out whether interdental CAL is present in more than one, non-adjacent teeth (deciding criteria for periodontitis). If it is present, we have a patient with periodontitis for which we need to make a comprehensive diagnosis by doing periodontal charting and analyzing full mouth radiographs. If the periodontal charting does not show a PPD of 4 mm or more, we need to evaluate full-mouth bleeding on probing. If bleeding on probing is present in >10 % sites, the patient is diagnosed with gingival inflammation in a periodontitis patient. If bleeding on probing is present in <10 % sites, the patient is diagnosed with reduced but healthy periodontium. If periodontal charting shows PPD 4 mm or more, we need to move forward with the staging and grading process.
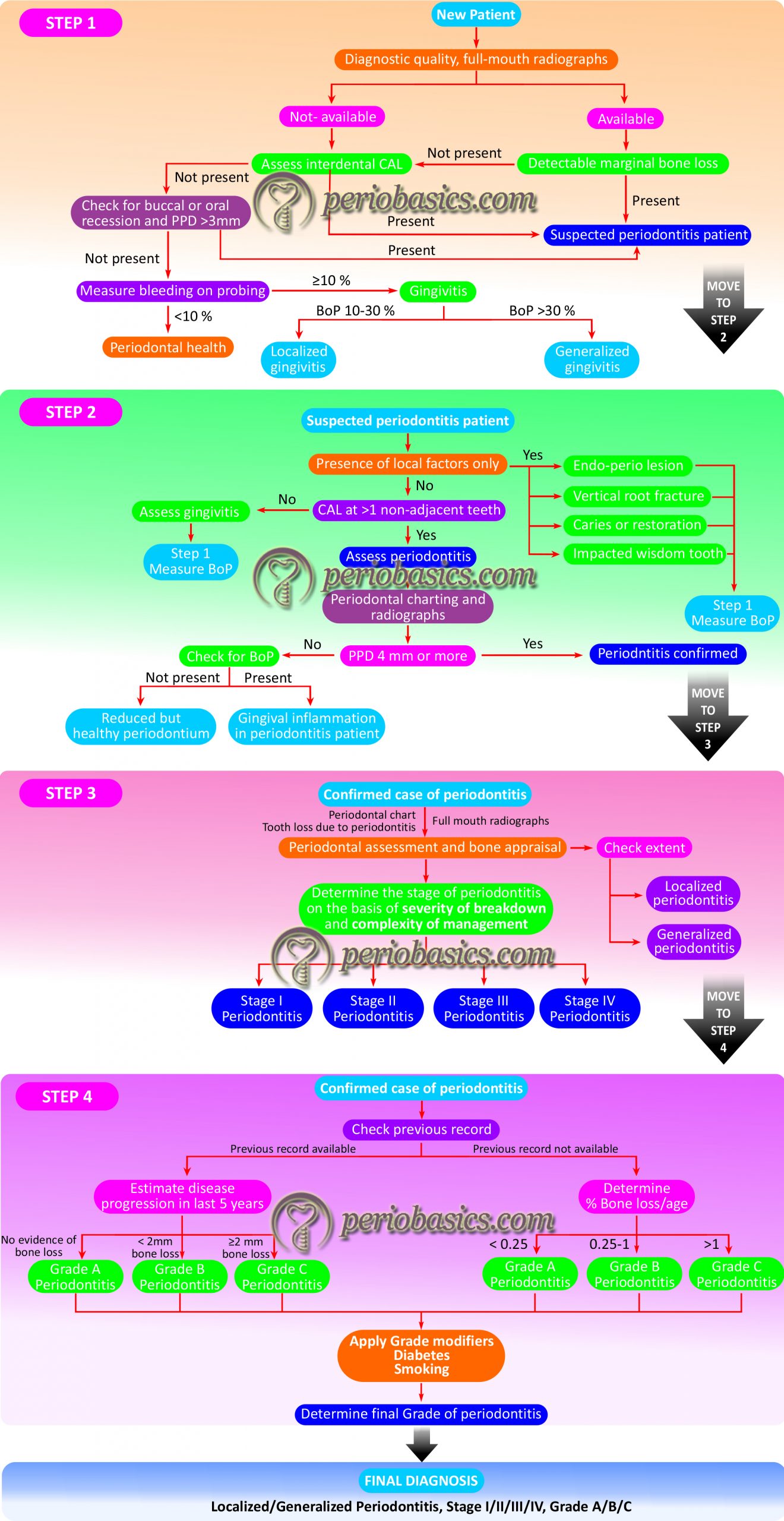
Step 3:
In this step, we establish the stage of periodontitis. To establish the stage of periodontitis, we need to have full mouth radiographs, a periodontal chart, and a periodontal history of tooth loss. We first need to establish whether it is a case of generalized or localized periodontitis. To do so, we analyze the radiograph for bone loss and check CAL in the periodontal chart. If CAL or bone loss affects less than 30% of the teeth, it is a case of localized periodontitis and if it affects 30% or more teeth, it is a case of generalized periodontitis. Finally, the stage is decided on the basis of severity (CAL, bone loss and tooth loss due to periodontitis) and complexity factors (by assessing PPD, furcation and intrabony lesions, tooth hypermobility, secondary occlusal trauma, bite collapse, drifting, flaring, or having fewer than 10 occluding pairs of teeth) (See Table 20.11). After establishing the stage, we need to establish the grade of periodontitis.
Step 4:
The grade of periodontitis is decided based on direct or indirect evidence of disease progression. For grading a patient, initially … Contents available in the book……….. Contents available in the book……….. Contents available in the book…………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Critical analysis of 2017 classification system
With immense research in the field of periodontics since 1999 World Workshop, it was necessary to re-define various periodontal and peri-implant diseases and conditions. The AAP and EFP jointly proposed the classification for periodontal and peri-implant diseases and conditions in 2017. The most attractive point of this classification is that it is clinically oriented and facilitates decision making in clinical practice. Grading and Staging of periodontitis was the need of the hour because it not only describes the extent and severity of the disease but also the rate of disease progression which directly affect the treatment planning. Another positive point regarding this classification is that a room has been left for future research and evidence. However, at the same time, the classification is comprehensive and is difficult to remember in its elaborated form. Further, students of periodontology need to be well versed with all aspects of the etiopathogenesis of periodontal diseases to clearly understand this classification. As we are doing extensive research on various aspects of the pathophysiology of periodontal diseases, we may incorporate various biomarkers in the decision making process. These evidences may be incorporated in the present classification system.
Conclusion
In this chapter, we discussed in detail the evolution of classification systems for periodontal and peri-implant diseases. Because periodontal diseases are multi-factorial diseases, it is not easy to simply classify these diseases into different categories. The risk factors have a significant effect on the progression of these diseases. Our scientific knowledge has tremendously improved since the introduction of initial classifications proposed by Gottlieb, Orban and Page & Schroeder. The World Workshop 2017 classification is based on sound scientific ground and is the most clinically oriented classification. However, tremendous research is still going on in the field of periodontics to understand the pathophysiology of periodontal and peri-implant diseases and in the future, we can expect more improvisations in this classification system.
References
References are available in the hard-copy of the website.
Suggested reading

