Introduction to classification systems used in periodontics
Our basic understanding regarding periodontal diseases and the concepts in the etiopathogenesis of periodontal diseases have evolved and substantially changed during the past centuries. The initial classification systems were based on the clinical features of the diseases (1870-1920), then came the concepts of classical pathology (1920-1970), and presently we are following the concepts of infectious etiology of periodontal diseases and host response (1970-present) 1. The most important landmark in our current understanding of periodontal diseases was the work done by Lӧe et al. (1986) 2 on the natural history of periodontal disease, where they observed the progression of periodontal diseases naturally without interfering. Their observations showed that the natural history of periodontal disease, in some but not all patients, results in tooth loss. In the following sections, we shall study why many classification systems were proposed, their drawbacks and finally the classification system that we are following presently.
Why do we need a classification system?
Diseases are classified to simplify our understanding regarding different diseases in a particular medical or dental field. Generally, diseases are classified according to their etiology into different classes like, inflammatory, congenital, genetic, neoplastic, acquired, etc. Disease names which last with “itis” have an inflammatory etiology, for example, periodontitis. Classification of diseases also helps us to communicate, for example, if I say a patient is suffering from generalized periodontitis Stage III, Grade C, you shall have an idea about all the clinical signs and symptoms of the disease and present periodontal status of the patient. So, half the job is done. Now we can elaborate the disease by going into detailed clinical and radiographic examination of the patient. Classification also helps us to formulate the treatment plan, predict the outcome of treatment as well as to educate the patient about the disease.
Historical background
The initial workers on periodontal diseases did not specify any particular terminology for these conditions, until Fauchard (1723) 3, who used the term “scurvy of the gums”, for the first time. Since then, researchers have introduced names for diseases of the periodontium on the basis of etiologic factors, pathologic changes or clinical manifestations. For the ease of understanding, let us divide the classification systems proposed on the basis of dominant paradigms,
Classification of periodontal diseases based on the clinical features paradigm (1870 to 1920)
These were initial classification systems proposed solely on the basis of clinical features of the disease. At that time, there was a little knowledge about the etiopathogenesis of the diseases. Many researchers at that time proposed that these diseases are caused by local factors 4-8 while others believed that systemic factors were responsible for the diseases 9-12. Some researchers suggested that local factors are responsible for the diseases, but in some cases systemic factors also play an important role 13-15. During this time period, due to relatively fewer publications and lack of appropriate interactions between different schools of thoughts, researchers individually put forward their point of view regarding the classification of periodontal diseases. G V Black (1886) 16, based on his understanding of clinical features of different periodontal diseases, published the following classification,
| G V Black classification of periodontal diseases |
|---|
| Constitutional gingivitis |
| Painful form of gingivitis |
| Simple gingivitis |
| Calcic inflammation of the peridental membrane |
| Phagedenic pericementitis |
Constitutional gingivitis:
These included scurvy, mercurial gingivitis, and potassium iodide gingivitis. Painful form of gingivitis: This condition is presently known as necrotizing ulcerative gingivitis (NUG) which is a painful condition with necrosis of gingiva and tooth-supporting structures.
Simple gingivitis:
This term was used to describe the condition where local deposits caused inflammation of the periodontal membrane.
Calcic inflammation of the peridental membrane:
In this condition the calculus deposition was associated with an even or generalized pattern of destruction of alveolar bone which progressed through a long duration of time.
Phagedenic pericementitis:
This condition shared many features with the Calcic inflammation of the peridental membrane (presently called as periodontal ligament) except that the calculus deposition was less and there was an irregular pattern of alveolar bone destruction.
Classification of periodontal diseases based on the classical pathology paradigm (1920-1970)
This paradigm was dominated by the pathology of the disease process. Almost all the classification systems given during this period used terms like atrophic, degenerative, dystrophic etc. These classification systems were based on the ‘principles of general pathology’ as presented by Orban et al. (1958) 17. The first widely accepted classification system was given by Gottlieb, who classified periodontal diseases into four types 18-20.
| Gottlieb's classification of periodontal diseases |
|---|
| Schmutz-Pyorrhӧea |
| Alveolar atrophy or diffuse atrophy |
| Paradental-Pyorrhӧea |
| Occlusal trauma |
Schmutz-Pyorrhӧea:
The term Schmutz-Pyorrhӧea was used to describe a periodontal condition that was caused due to the accumulation of deposits on the teeth, leading to inflammation, shallow pockets, and resorption of the alveolar crest.
Alveolar atrophy or diffuse atrophy:
Alveolar atrophy or diffuse atrophy was described as a noninflammatory disease in which minimal local factors, i.e. deposits were present on the teeth, deep pockets were seen in later stages with the loosening of teeth and eventually leading to tooth loss.
Paradental-Pyorrhӧea:
Paradental-Pyorrhӧea was characterized by irregularly distributed pockets varying from shallow to extremely deep. The disease process, in this case, may have started as Schmutz-Pyorrhӧea or as diffuse atrophy.
Occlusal trauma:
The fourth condition described was occlusal trauma in which there were alveolar bone resorption and tooth mobility due to increased occlusal physical overload.
Orban in 1942 proposed a classification based on classical pathology paradigm 21. This classification was accepted by the American Academy of Periodontology (AAP) and gained wide acceptance. In this classification periodontitis was classified into two categories simplex and complex. Periodontitis simplex was secondary to gingivitis and characterized by bone loss, pockets, abscess formation and calculus deposits. Periodontitis complex was caused secondary to periodontosis, having similar etiological factors to periodontitis and little or no calculus and was considered as a degenerative disease. Based on the classical pathology paradigm, many classifications were given during this time period. These include classification by Fish 1944 22, Goldman et al. 1956 23, Goldman and Cohen 1968 24, and Grant et al. 1968 25.
| Orban's classification of periodontal diseases |
|---|
| Inflammation |
| I. Gingivitis (little or no pocket formation: can include ulcerative form - Vincent's) A. Local (calculus, food impaction, irritating restorations, drug action, etc. B. Systemic Pregnancy Diabetes and other endocrine dysfunctions Tuberculosis Syphilis Nutritional disturbances Drug action Allergy Hereditary Idiopathic II. Periodontitis Simplex (secondary to gingivitis). Complex (secondary to periodontosis). |
| Degeneration |
| Periodontosis (as a rule attacks young girls and older men; often caries immunity) A. Systemic disturbances a) Diabetes b) Endocrine dysfunctions c) Blood dyscrasias d) Nutritional disturbances e) Nervous disorders f) Infectious diseases (acute and chronic) B. Hereditary C. Idiopathic |
| Atrophy |
| Periodontal Atrophy (Recession, no inflammation, no pockets; osteoporosis.) A. Local trauma (e.g., from toothbrush) B. Presenile C. Senile D. Disuse E. Following inflammation F. Idiopathic |
| Hypertrophy |
| Gingival Hypertrophy A. Chronic irritation (see inflammation) B. Drug action (e.g. Dilantin sodium) C. Idiopathic (e.g. gingivoma, elephantiasis, fibromatosis) |
| Traumatism |
| Periodontal Traumatism A. Occlusal trauma |
Classification systems based on infection/host response paradigm (1970-present)
This paradigm started with the classical ‘experimental gingivitis’ studies published by Harald Löe and his colleagues from 1965 to 1968 26-29. Their research work showed that host response is an important factor in determining the disease progression and its outcome. Along with this, research done on neutrophils from juvenile periodontitis (periodontosis) cases showed their defective chemotactic and phagocytic functions which supported this concept 30-31.
Page and Schroeder in 1982 32 proposed a new classification system which was based on infection/host response paradigm. In this classification five distinctly different forms of periodontitis were described. It is important to discuss this classification as the American Academy of Periodontology (AAP) in 1986 adopted a new classification that incorporated these groups.
| Page and Schroeder classification of periodontal diseases |
|---|
| Prepubertal periodontitis Generalized Localized |
| Juvenile periodontitis |
| Rapidly progressing periodontitis |
| Adult type periodontitis |
| Acute necrotizing ulcerative gingivo-periodontitis |
Prepubertal periodontitis:
This type of periodontitis was described as a condition that occurs during or immediately after the eruption of primary teeth. Two forms were described in this condition: localized and generalized. In the generalized form acute inflammation is present with the proliferation and clefting of the gingival margin. Genetic predisposition is ……………..Contents available in the book……….Contents available in the book……….Contents available in the book……….Contents available in the book…..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Juvenile periodontitis:
This condition was described as of circumpubertal origin where the diagnosis was usually made at an age beyond puberty. Lesions are primarily around permanent first molars and/or incisors with the usually symmetrical distribution. The disease is 4 times more prevalent in females as compared to males. Clinically gingiva appears completely normal with minimal local factors. X-linked dominant or recessive genetic trait is present. The majority of patients with this condition have neutrophil and monocyte function defects.
Rapidly progressing periodontitis:
This condition was described as generalized, affecting most of the teeth with the age of onset between puberty and 35 years. The periodontal destruction is rapid which gradually slows down spontaneously. In active disease, the gingiva is acutely inflamed with marginal proliferation, whereas in inactive disease gingiva may appear completely normal. Most of the patients have neutrophil and monocyte function defects. Most of the patients respond appropriately to the treatment, but a small number of patients are refractory to treatment.
Adult periodontitis:
Here, the age of onset of the disease was described as usually 30 to 35 years and older. Incisors and molars are more severely affected as compared to rest of the dentition. The accumulation of plaque is consistent with periodontal destruction. Neutrophil and monocyte function defects are not usually present. The pattern of bone destruction is highly variable. Acute inflammation of gingiva is not usually present with gingiva being more fibrotic and thickened. The disease is usually treatable by routine non-surgical and surgical periodontal therapy.
Acute necrotizing ulcerative gingivo-periodontitis:
This was described as an acute infective condition characterized by deep craters in the interdental bone, either in localized regions or throughout the mouth. The mouth of the patient is foul-smelling. This condition is usually seen in malnourished or immunocompromised patients. A pseudomembrane is seen on the lesion made up of necrotic tissue and bacteria.
Based on the classification given by Page and Schroeder (1982), American Academy of Periodontology (AAP) in 1986 adopted a new classification system. Further, AAP at the World Workshop in Clinical Periodontics at Princeton in 1989 33 amended the classification system with a few refinements. 1989 AAP classification of periodontal diseases was based on the following factors,
- Presence ⁄ absence of clinically detectable inflammation.
- Extent and pattern of attachment loss.
- Patient’s age at onset.
- Rate of progression.
- Presence ⁄ absence of miscellaneous signs and symptoms, including pain, ulceration and amount of observable plaque and calculus.
| AAP periodontal disease classification systems 1986 |
|---|
| I. Juvenile Periodontitis A. Prepubertal B. Localized juvenile periodontitis C. Generalized juvenile periodontitis |
| Adult Periodontitis |
| Necrotizing Ulcerative Gingivo-Periodontitis |
| Refractory Periodontitis |
| AAP periodontal disease classification systems 1989 |
|---|
| I. Early-Onset Periodontitis A. Prepubertal periodontitis 1. Localized 2. Generalized B. Juvenile periodontitis 1. Localized 2. Generalized C. Rapidly progressive periodontitis |
| Adult Periodontitis |
| Necrotizing Ulcerative Periodontitis |
| Refractory Periodontitis |
| Periodontitis Associated with Systemic Disease |
Drawbacks of AAP 1989 classification system:
- One major drawback of this classification was that it was heavily depended upon the age of the patient 34-36.
- Classification did not include gingivitis or gingival disease category.
- There was considerable overlap between different categories within the classification system. Some cases were difficult to place in one category as they possessed some features of other category also. Especially, ‘rapidly progressive periodontitis’ was a heterogeneous category.
- Different forms of periodontitis proposed in the classification shared many microbiological and host response features, which suggested extensive overlap and heterogeneity among the categories 37.
- The refractory periodontitis was also a heterogeneous category as the criteria for this condition were difficult to relate clinically while placing the patient in this category.
As a result of these drawbacks, Ranney in ………..Contents available in the book……….Contents available in the book……….Contents available in the book……….Contents available in the book…..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
American Academy of Periodontology (AAP) world workshop 1999 classification of periodontal diseases and conditions
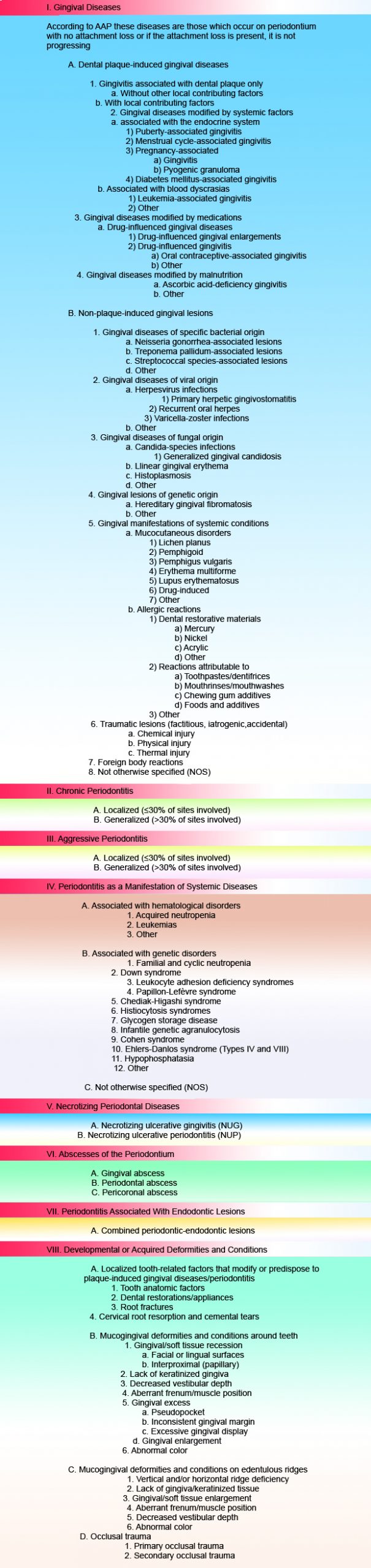
In 1999 an international workshop for classification of periodontal diseases and conditions was held at Oak Brook (Illinois, USA), in which a group of internationally acknowledged experts produced a generally accepted and scientifically founded classification of periodontal diseases 40. This classification was quite different from earlier classifications as it addressed a wide variety of periodontal diseases and conditions. This classification was very complete, detailed and complex. The simplified classification is as follows,
I. Gingival diseases,
- Plaque-induced.
- Non-plaque induced.
II. Chronic periodontitis,
- Localized.
- Generalized.
III. Aggressive periodontitis,
- Localized.
- Generalized.
IV. Periodontitis as a manifestation of systemic disease.
V. Necrotizing periodontal diseases.
VI. Abscesses of the periodontium.
VII. Periodontitis associated with endodontic lesions.
VIII. Developmental or acquired deformities and conditions.
AAP world workshop 1999 Classification of Periodontal Diseases and Conditions
Highlights of AAP world workshop 1999 classification system
Addition of a gingival disease component:
This is an important change in the 1999 classification of periodontal diseases and conditions. Gingivitis is commonly attributed to plaque accumulation, but many other conditions also have gingivitis as one of the clinical features. So, in the 1999 classification, we have two categories,
- Dental plaque-induced gingival diseases: These include plaque-induced gingivitis and systemic conditions as well as endocrinal conditions which exacerbate plaque-associated gingivitis. Systemic diseases such as diabetes and leukemia can exacerbate plaque-associated gingivitis. Endocrine changes (puberty, pregnancy), medications (nifedipine, cyclosporine, and phenytoin) and malnutrition (vitamin C deficiency) add a component to plaque-induced gingivitis.
- Non-plaque-induced gingival lesions: In this category we have mucocutaneous disorders (e.g., lichen planus, pemphigoid), allergic reactions (e.g., restorative materials, toothpaste, gum), trauma (chemical, physical or thermal) as well as disorders of genetic origin such as, hereditary gingival fibromatosis. The gingivitis in these conditions cannot be attributed to plaque accumulation so these are categorized as Non-plaque-induced gingival lesions.
Replacement of “Early-Onset Periodontitis” with “Aggressive Periodontitis”:
In 1989 classification, early-onset periodontitis category consisted of patients having significant attachment loss in the presence of little local factors (plaque and calculus) and age less than 35 years. Although it is a fact that this condition is commonly found in people under 35 years of age, but it may also affect older patients. So, a new term “aggressive periodontitis” was introduced for this condition because the earlier term was too restrictive. The diagnosis of aggressive periodontitis is made on the basis of ………..Contents available in the book……….Contents available in the book……….Contents available in the book……….Contents available in the book…..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Replacement of “Adult Periodontitis” with “Chronic Periodontitis”:
Adult periodontitis category in 1989 classification was designated for patients more than 35 years of age, having a slow rate of disease progression and periodontal destruction consistent with the presence of local factors. Although these cases are common at the age 35 years or more, but this condition can be seen in adolescents and even in the primary dentition of children. Another drawback was, the age at which a patient presents for the treatment does not necessarily reflect the age at which the disease began. So, to overcome these difficulties, a new term “Chronic periodontitis” was given to categorize these patients. The disease was categorized as localized if <30% teeth were involved and generalized if >30% teeth were involved and severity was classified on the basis of clinical attachment loss (CAL) as slight (1-2 mm CAL), moderate (3-4 mm CAL) or severe (≥ 5 mm CAL). Periods of disease progression and regression may occur in a random manner in this condition.
Elimination of the ‘Prepubertal Periodontitis’ category:
It was difficult to categorize prepubertal periodontitis as a single entity as some of the severe cases of periodontitis in children were attributed to systemic diseases and some may occur without any modifying factors 41, 42. In fact the beginning of chronic periodontitis has been suggested to start during childhood. So, this category was discontinued in the new classification.
Discontinuation of term “Refractory Periodontitis”:
As our present knowledge about the pathogenesis of periodontal diseases suggests that there are many factors that affect the disease progression and its response to the treatment, category “Refractory Periodontitis” was eliminated as a separate entity in the new classification. Factors like extent of disease prior to the therapy, type of therapy provided (nonsurgical or surgical, with or without antibiotics, etc.), tooth type and furcation involvement, species and strains of microflora, degree of host response (particularly immune response), and whether the patient smokes make it difficult to classify a patient as a refractory periodontitis patient. So, based on these factors this category was discontinued.
Replacement of “Necrotizing ulcerative periodontitis” with “Necrotizing periodontal diseases”:
Another important change was replacement of “Necrotizing Ulcerative Periodontitis” with “Necrotizing Periodontal Diseases”. Necrotizing ulcerative gingivitis (NUG) and necrotizing ulcerative periodontitis (NUP) were clinically distinguishable disease entities but it was unclear that whether they were a part of the same disease process or were two distinct diseases. So, a new term “Necrotizing Periodontal Diseases” was used for these conditions.
Addition of “Periodontal Abscesses” and “Periodontitis associated with endodontic lesions” as new entities:
These conditions were added to the classification system as such without any change in their definitions. Periodontitis associated with endodontic lesions indicate periodontic-endodontic lesions in which there are both periodontic and endodontic components.
Addition of new category “developmental and acquired deformities and conditions”:
These are conditions which influence the course of the disease and may dramatically affect the results of treatment. So, it was felt that these acquired deformities and conditions should be added in the classification as a separate category.
Critical analysis of AAP 1999 classification system
An important observation that we make in the 1999 classification system is that it appears complicated and too comprehensive, particularly from the clinical aspect. It may be difficult to remember details of the classification. But on the other hand, earlier, simpler classification systems were not able to clearly classify some patients, which was their major drawback. Furthermore, it should be noted that although, criteria have been framed to differentiate between aggressive and chronic periodontitis, there are still clinical situations where it may be difficult to classify a case as aggressive or chronic periodontitis. A chronic periodontitis case may have periods of rapid periodontal breakdown and during this period the case may mimic an aggressive periodontitis case. One more point to be mentioned here is regarding the recession. The attachment loss in the absence of periodontitis (such as toothbrush trauma) cannot be considered as periodontitis.
After completion of periodontal treatment, periodontal health is re-established with reduced periodontium. There is no clear categorization of such cases in this classification. Finally, dental implants have become an inseparable part of periodontics but implant-associated diseases have not been classified in the 1999 classification system. Keeping all these points in mind, the scientific community came together recently in 2017 and proposed a new classification for periodontal and peri-implant diseases and conditions.
Conclusion
The primary purpose of a classification system is to systematically classify the diseases into various categories. It not only simplifies our understanding regarding the diseases but also facilitates communication. The understanding of the historical aspect of the classification systems is essential to understand the presently used classification. In the next article we shall read the recent 2017 classification system for classifying periodontal and peri-implant diseases and conditions.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

