Introduction to tissue engineering
Regeneration of the lost periodontal tissues is the ultimate goal of a successful periodontal therapy. A lot of techniques have been used to achieve this goal so far. More recent introduction in this context is the concept of tissue engineering. Tissue engineering is defined as the science of fabrication of new tissues for replacement and regeneration of lost tissues or defined tissues 1. This approach for regeneration of the lost tissues was proposed by Langer and Vacanti in 1993 2. The primary aim of this therapy is to deliver biologically active elements which get integrated into the host tissues and result in three-dimensional regeneration of the lost tissue which is structurally and functionally similar to the tissue which was lost. Generally, tissue engineering involves combining of living cells with a natural/synthetic support or scaffold that is also biodegradable to build a three-dimensional living construct that is functionally, structurally and mechanically equal to or better than the tissue that is to be replaced 3. In the following sections, we shall discuss in detail various aspects of tissue engineering.
Key elements in tissue engineering
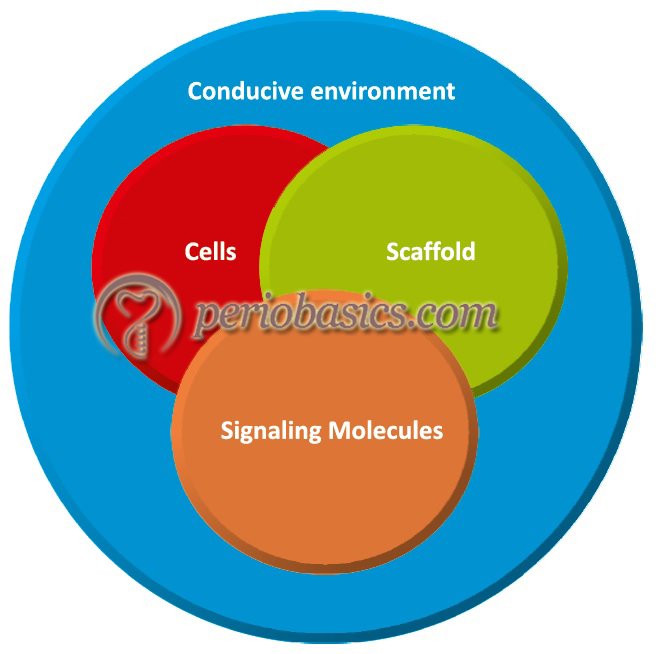
To achieve complete regeneration of the lost tissue, we need to have progenitor cells which can differentiate into desired cell types and give rise to desired structural components of extracellular matrix (ECM) and signaling molecules which initiate desired cellular activities, a scaffold which is able to carry these components in the active form and a conducive environment. Presently, there are two approaches used to regenerate tissues,
Ex vivo approach:
In this approach, the tissue is created in a laboratory by culturing the cells on a biodegradable scaffold in the presence of molecular factors required for growth and then it is transferred into the body. Various body organs have been developed by this technique.
In vivo approach:
In this technique, all the components which are required for regeneration are placed in the tissue defect and an environment which is conducive to maximum regeneration is created to achieve favorable regeneration.
To achieve any kind of tissue regeneration, some basic components are required, which participate at different levels in the formation of the desired tissue. These can be called as key elements of tissue engineering. These include,
- Progenitor cells.
- Scaffold or supporting matrix.
- Signaling molecules.
Following is the brief description of these components of in vivo regeneration,
Progenitor cells
There has been a lot of research on the regenerative capacity of post-natal progenitor cells. These cells can differentiate into different types of end cells and can form the desired structural components of the lost tissue. However, these cells should satisfy the following criteria to achieve effective, long-lasting repair of the damaged tissues 4,
1. An adequate number of cells must be produced to fill the defect.
2. Cells must be able to differentiate into desired pheno-types.
3. Cells must adopt appropriate three-dimensional structural support/scaffold and produce ECM.
4. Produced cells must be structurally and mechanically compliant with the native cells.
5. Cells must successfully be able to integrate with native cells and overcome the risk of immunological rejection.
6. There should be minimal associated biological risks
The source of these progenitor cells may be autologous, allogeneic or xenogeneic. Autologous or autogenic source (derived from the patient) is an ideal source of these cells because of low association with immune complications and almost complete acceptability. Allogeneic source (derived from another member of the same species) of these cells is also ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Progenitor cell population in periodontal tissues:
The first evidence for the presence of undifferentiated mesenchymal cells within periodontal tissues was provided by McCulloch and co-workers (1987) 5. Most of the present literature on periodontal regeneration has discussed periodontal ligament-derived cells for their potential to differentiate into various different types of cells required for the regeneration of lost tissues. However, other sources including periodontal ligament-derived mesenchymal stromal cells, periosteal cells, bone marrow-derived mesenchymal stem cells (BM-MSCs), adipose-derived stem cells (ADSCs), ES/iPS cells and gingival fibroblasts have also been investigated recently.
Periodontal ligament (PDL) derived progenitor cells:
The ability of PDL-derived progenitor cells in periodontal regeneration was discovered way back when research in this field had just started. The PDL stem cells have the capability to produce cementum and periodontal ligament-like structure and contribute to periodontal tissue repair. It has been shown that PDL stem cells can differentiate into ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Periodontal ligament (PDL) derived mesenchymal stromal cells:
The mesenchymal stem cells were initially identified in aspirates of adult bone marrow. Later on, Friedenstein et al. (1970, 1976, 1987) 7-9 in their experiments developed clonogenic clusters of adherent fibroblastic-like cells or fibroblastic colony-forming units with the potential to undergo extensive proliferation. These cells had the capacity to differentiate into different stromal cell lineages. The periodontal ligament-derived mesenchymal stromal cells were isolated by Seo et al. (2004) 10 in an experiment where they showed that ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Periosteal cells:
Along with differentiation into an osteoblastic lineage, periosteal cells also have the capability to express PDL related genes. In an experiment, it was observed that these cells were clonogenic, displayed long telomeres and expressed markers of mesenchymal stem cells (MSCs), regardless of donor age 11. In another experiment Mizuno et al. (2006) 12 repaired Class III furcation defects in Beagle dogs by grafting autologous periosteal cells, which were cultured from membrane derived from the periosteum. In another experiment, Yamamiya et al. (2008) 13 showed that ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Bone marrow-derived mesenchymal stem cells (BM-MSCs):
These cells have a potential to differentiate into various target cells, which are capable of producing bone, cartilage, adipose tissue, muscle, and periodontal tissues etc. 14-17. Recently, it has been demonstrated by in vitro studies that these cells are capable of inducing periodontal regeneration 16, 18. In another experiment, BM-MSCs were used in combination with platelet-rich plasma (PRP). The results of the study demonstrated that this combination was capable of inducing periodontal regeneration 19.
Adipose-derived stem cells (ADSCs):
Recent research has reported the potential of ADSCs to be used in periodontal tissue regeneration. One major advantage of ADSCs is that adipose tissue from where these cells are obtained is abundant and easy to obtain as compared to other sources. These cells have been shown to differentiate into different tissue types 20-23. In vitro experimental studies have shown that the combination of PRP and ADSCs was capable of inducing periodontal regeneration in bony defects 24, 25. Hence, these cells need to be further investigated for their potential for periodontal regeneration.
Gingival fibroblasts:
Cell transplantation therapy using gingival fibroblasts has been developed for root coverage in areas with recession. The gingival fibroblasts were seeded onto sponges of human Type I or III recombinant collagen. After culturing, vascular endothelial growth factor (VEGF) and hepatocyte growth factor (HGF) were released in the culture media. It was observed that there was a significant increase in fibroblast proliferation, indicating that the technique may provide a new tool for the treatment of ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Scaffold or supporting matrix
Scaffolds are natural or synthetic materials used to carry biologically active molecules to the site of regeneration. Tissue engineering scaffolds have been fabricated using several natural and synthetic polymers. The primary requirements for a scaffold are,
- It must be inherently biocompatible.
- It should be biodegradable, and highly cell-adhesive.
- It should have a porous, mechanically stable, and three-dimensional structure.
- It should have a simple and predictable manufacturing process.
Naturally derived scaffold materials:
The natural polymers used for tissue engineering applications include fibrin, collagen, gelatin, chitosan, alginate, and hyaluronic acid 31-36.
Fibrin:
It is an important component of the blood clot and is used in mixtures with thrombin to produce an in-situ forming gel which is used as a scaffold to carry various biologically active molecules.
Collagen:
It is one of the most widely used scaffold material. Type I collagen is usually derived from animal tissues and gelatin.
Chitosan:
It is a cationic polymer derived from chitin. Its scaffold produces a hydrophilic surface which is osteoconductive which indicates its potential use for bone tissue engineering.
Alginate:
It is an anionic polysaccharide derived from brown algae. It forms a gel when complexed with divalent cations such as Ca2+.
Hyaluronic acid:
It is a non-sulfated glycosaminoglycan of repeating disaccharide units. It is a major component of connective tissue, forming cross-linkable hydrogels with various modifications.
Synthetically derived scaffold materials:
These are biodegradable synthetic polymers which have matrices in their structure to carry bioactive molecules. The commonly used chemical compounds to fabricate synthetic scaffolds include poly(α-hydroxyester)s, polyanhydrides, and polyorthoesters 37. Among these polymers, poly(α-hydroxy-ester)s such as polylactide (PLA), polyglycolide (PGA), and its copolymers are most extensively used. These polymers have been approved by the Food and Drug Administration (FDA). They are biocompatible, biodegradable, bioresorbable and can be easily processed to form various 3-D structural matrices. A major advantage of poly (lactide-co-glycolide) (PLGA) copolymers is that they ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
These polymers can also be fabricated in the form of microspheres and can be injected at the site of the defect. Furthermore, these can also be used to make scaffolds with nanofibrous structure. The disadvantage of these polymers is that when they degrade, they produce acidic by-products which may hamper the process of regeneration. The solution to this problem is the use of biodegradable hydrogel scaffolds fabricated with hydrophilic polymers such as poly (ethylene glycol), which do not produce acidic by-products on degradation.
Scaffold fabrication
There are various methods to make scaffolds which are then used to carry bioactive molecules. These include,
- Fiber bonding.
- Emulsion freeze-drying.
- Solvent casting/particulate leaching.
- High-pressure processing.
- Gas foaming/particulate leaching.
- Thermally-induced phase separation.
- Electrospinning.
- Rapid prototyping.
Fiber bonding:
In this technique, interconnected fiber networks within the matrix are achieved. The PGA fibers are aligned in the shape of the desired scaffold and then embedded in a Poly (L -lactide) /methylene chloride solution. Once the solvent evaporates, Poly (L-lactide)/PGA composite is heated above the melting temperatures of both the polymers. Poly (L-lactide) is then removed by selective dissolution after ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Emulsion freeze-drying:
In this technique, an emulsion solution containing a dispersed water phase and an organic continuous phase is freeze-dried. It results in the formation of a porous scaffold with various pore sizes and inter-connectivities. Using this technique, up to 95% porous scaffold with a pore size, up to 200 μm has been prepared 38.
Solvent casting/particulate leaching:
Another method to create pores involves the use of a water-soluble porogen, such as salt (NaCl). In this technique, the polymer (PLLA or PLGA) is first dissolved in chloroform or methylene chloride and then is casted onto a petri dish filled with the porogen. Once the solvent evaporates, the ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
High-pressure processing:
In this technique, a gas such as CO2 is applied at high pressure to the dry polymer. It results in the formation of a single-phase polymer/gas solution. After the formation of this single-phase polymer/gas solution, pressure is reduced, which creates thermodynamic instability in the dissolved CO2 and results in nucleation and growth of gas cells to generate pores within the polymer matrix. This technique has been used to make highly porous sponges of PLGA 39.
Gas foaming/particulate leaching:
This technique was developed by Park et al., where they made a binary solution of PLA-solvent gel containing dispersed ammonium bicarbonate salt particles. The mixture was casted in a mold and subsequently immersed in hot water. Due to increased temperature, ammonia and carbon dioxide gas are formed along with the leaching out of ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Thermally-induced phase separation:
This procedure involves phase separation by thermodynamic demixing of a homogeneous polymer-solvent solution into a polymer-rich phase and a polymer-poor phase. Liquid-liquid phase separation or emulsification/freeze-drying method is used to separate the two phases. The polymer solution is quenched below the freezing point of the solvent and subsequently freeze-dried. It results in the formation of a highly porous structure. The porosity of the structure can be modified by changing the thermodynamic and kinetic parameters.
Electrospinning:
This is the most widely used method for preparation of nanofiber non-woven matrices. In this technique, a polymer solution is pumped at a constant rate through a syringe with a small-diameter needle that is connected to a high-voltage source. When this voltage source is turned on, an electric field is created between the needle and a metallic collecting plate. Under the strong electrical field, electric charge overcomes the surface tension of the polymer ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Rapid prototyping:
In this method, a computer-aided design (CAD) with pre-decided three-dimensional architecture is formed in a layer-by-layer manner with precise control over its morphological characteristics. This is the most recent introduction in the field of tissue engineering and is being extensively investigated for fabrication of scaffolds for carrying bioactive molecules. The main advantage of this technique is that a scaffold with a predetermined size, shape, porosity, chemical composition and desired mechanical properties can be fabricated.
Signaling molecules
The signaling molecules play a vital role during various biological processes. They are secreted from various cells in response to a stimulus and they act on the same, neighboring or distant cells to cause specific effects. The knowledge of signaling molecules involved in regeneration is primarily derived from wound healing. A detailed description of biological events that happen during wound healing has been discussed in “Biology of periodontal regeneration”.
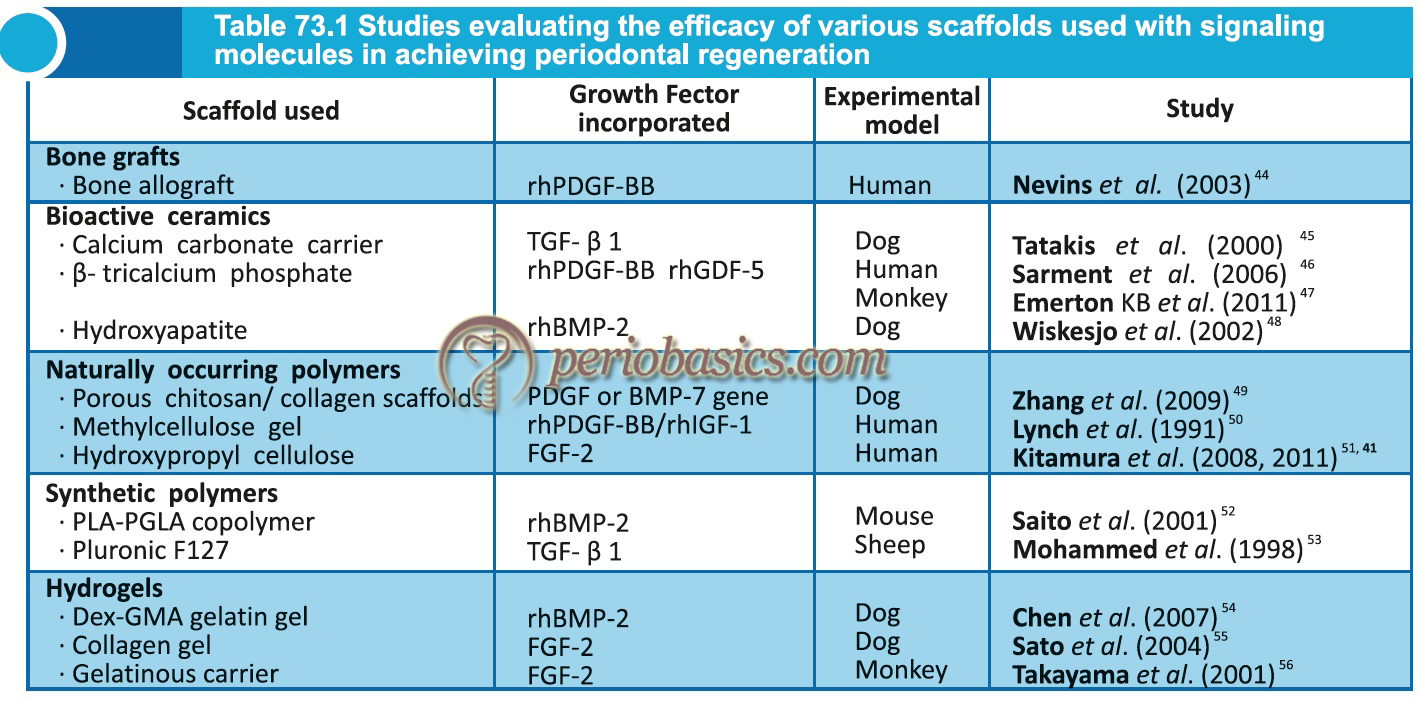
The application of growth factors and bone morphogenetic proteins (BMP’s) has been shown to enhance periodontal regeneration 24, 41, 42. Growth factors play a vital role during growth and development. They enhance regeneration via stimulating synthesis of ECM by cells such as fibroblasts, osteoblasts etc. A detailed description of the role of growth factors in periodontal regeneration has been given in “Application of growth factors in periodontal regeneration”. Presently, some recombinant growth factors have been made available for commercial use, including platelet-derived growth factor (PDGF; GEM21®) and bone morphogenic protein-2 (BMP-2; Infuse®) 43. The potential of fibroblast growth factor (FGF)-2 has recently been investigated for its efficacy in periodontal regeneration in large clinical trials 24, 41. These studies warrant further research on this growth factor and its clinical use on a large scale. Following table describes various animal and human studies that have been done to evaluate the efficacy of various scaffolds used with signaling molecules in achieving periodontal regeneration,
Desired properties of scaffolds used for periodontal regeneration
To achieve regeneration in the periodontal defects, the biomaterial placed in the defect should have some desirable properties. The scaffold material should allow cell-cell and cell-matrix interaction of bioactive molecules (such as growth factors) with the surrounding environment. The scaffold should hold the growth factor in its matrix for a desirable duration of time so that the growth factor can exert its effect on the surrounding cells and matrix for long enough. The scaffold should be ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
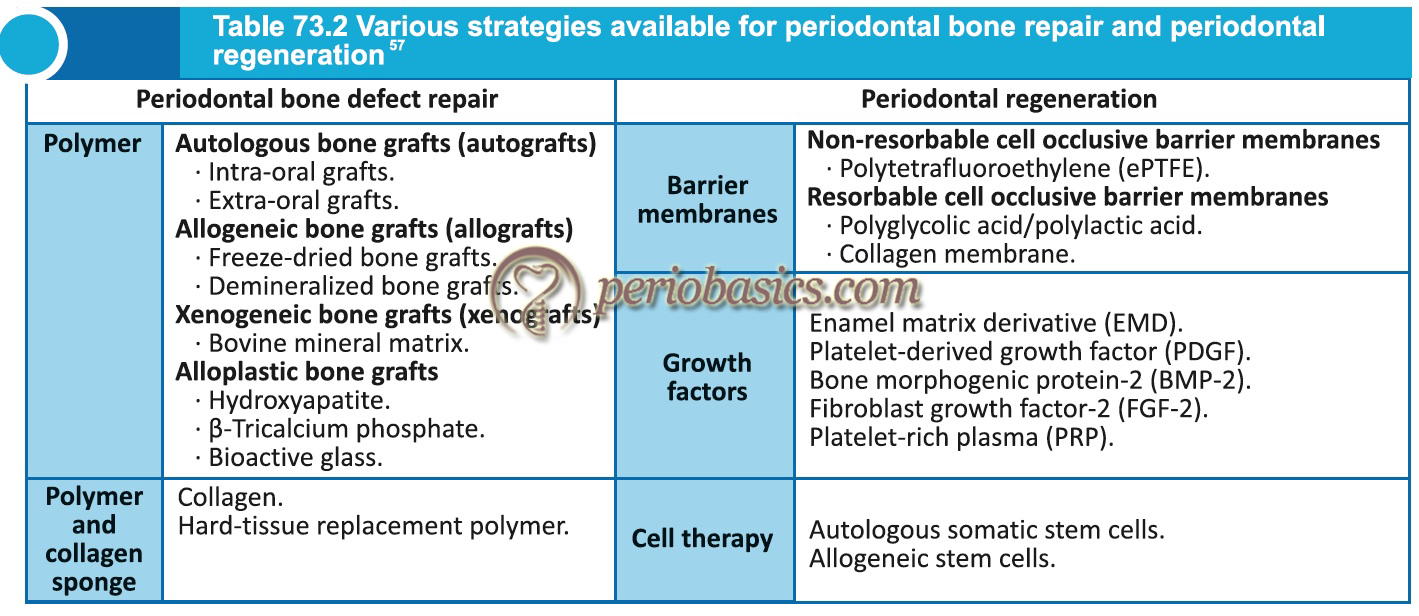
Current strategies for periodontal regeneration
The current methods to achieve periodontal regeneration are based on using a scaffold which may or may not carry biologically active molecules in periodontal defect (bone grafts or hard tissue replacement polymer) or creating a three-dimensional area secured by a membrane to allow the proliferation of cells from PDL to facilitate regeneration (guided tissue regeneration). Presently, research is being done to incorporate various biologically active molecules (BMP’s and growth factors) in scaffolds which are placed in the periodontal defect to achieve maximum regeneration. The scaffolds used so far in periodontal research include bone grafts, synthetic polyesters such as polyglycolic acid, polylactic acid and ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Bone grafts:
Bone grafts can be autogenic, allogeneic or xenogeneic depending on their source from where they are derived from. The biological properties of bone grafts can be described by three interrelated but not identical terminologies: osteogenic (formation of new bone by stem cell lineage derived from graft material); osteoinductive (bone growth by the surrounding immature cells recruited by graft material); and osteoconductive (bone growth on the surface of a material with fabrication) 58. Autogenous bone grafts are considered as gold standard because of their osteogenic and osteoinductive properties and complete acceptance. A detailed description of bone grafts has been given in “Bone grafts in periodontics”. The tissue engineering approach in ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Barrier membranes:
Barrier membranes are used to achieve regeneration by selectively allowing the growth of cells derived from PDL. Both biodegradable and non-degradable membranes have been used extensively to achieve periodontal regeneration. A detailed description of these membranes has been given in “Guided tissue regeneration”.
Gene therapy in periodontal tissue engineering
The problem associated with the delivery of proteins (growth factors and other bioactive molecules) is that they get easily degraded in the biological environment due to proteolytic breakdown by host enzymes. Secondly, to exert their effect, these factors should attach to their respective ligands on the target cells. The binding of the growth factors on target cells is not predictable. Their inability to bind to their receptors on the cell surface results in no biological activity by the target cell. Finally, lack of stability of scaffold carrying these molecules further jeopardizes the potential for regeneration.
To overcome these problems, gene therapy has been introduced which may circumvent many of the limitations of protein delivery systems 59, 60. The principle of gene therapy is to transfer desirable genes to the target cell which then synthesizes a protein of interest. The transfer of gene to target cells is achieved by viral (retroviruses, adenoviruses and adeno-associated viruses) and non-viral vectors (plasmids and DNA-polymer complexes) 61. The gene can be ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Ribonucleic acid-mediated silencing:
Fire and Mello were awarded the Nobel Prize in Physiology and Medicine in 2006 for their discovery of RNA interference (RNAi) gene silencing by double-stranded DNA 63. It is a biological process in which RNA molecules inhibit the expression of certain genes which are detrimental to the tissue regeneration by causing the destruction of specific mRNA molecules. RNA interference is executed by two types of small RNA molecules – microRNA (miRNA) and small interfering RNA (siRNA). RNAs are the direct products of genes, and these small RNAs can bind to other specific messenger RNA (mRNA) molecules. Most of the RNA-based research done presently uses siRNAs because they are safe and cost-effective. This technique is presently a focus of intensive research to make it useful in clinical practice and making it widely available.
Implantation of live cells to achieve regeneration:
Implantation of living cells in the periodontal defect and achieving regeneration is a challenging task. However, attempts have been made in this direction with varying degree of success. In a study, McGuire and Scheyer (2007) 64 implanted autologous fibroblast following a minimally invasive papilla priming procedure to augment open interproximal spaces. The interdental papillary height was assessed using subject visual analog scale. The results were found to be significantly better in test sites as compared to placebo sites. In another experiment, Bowsma and D’souza (2005) 65 expanded autologous fibroblasts and ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Implantation of tissue-engineered human fibroblast-derived dermal substitute:
Human fibroblast-derived dermal substitute (HF-DDS) is tissue-engineered living tissue derived from dermal fibroblasts. Various studies have compared the safety and effectiveness of this tissue in root coverage as compared to autogenous graft. One study compared the safety and effectiveness of a living HF-DDS to a connective tissue graft (CTG) for root coverage on Miller Class I or II bilateral facial recession. The results of the study showed that HF-DDS may offer a potential substitute to the connective tissue graft for root coverage 66. In another study, it was found that HF-DDS graft was capable of generating keratinized tissue around the teeth that did not require root coverage. Thus, morbidity and potential clinical difficulties associated with donor site surgery could be avoided with the use of this tissue 67.
Application of bi-layered cell therapy as a substitute to tissue from palate:
Tissue-engineered bi-layered skin substitutes have been used for immediate replacement of both, the lost dermis and epidermis in cases of skin burn or other injuries. This tissue is composed of Type I bovine collagen and viable allogeneic human fibroblasts and keratinocytes isolated from human foreskin. The tissue behaves in a similar manner as normal human skin. The proliferation of keratinocytes takes place in the basal layer of the epidermis and fibroblast proliferation takes place in the matrix. The keratinocytes produce various growth factors which facilitate wound healing. In an experiment, Momose et al. (2002) 68 estimated the levels of growth factors, including vascular endothelial growth factor (VEGF), transforming growth factor-α and β1 (TGF-α and β1), and epidermal growth factor (EGF) in tissue culture of human cultured gingival epithelial sheets (HCGES). The gingival tissues were obtained from the patient with generalized chronic periodontitis while performing flap surgery. It was observed that levels of these growth factors were significantly high in test cell culture media as compared to culture media without cells. Hence, these growth factors influence the ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Recent developments in the construction of “Smart scaffolds”
As already stated in the chapter, scaffolds, cells, and signaling molecules are the three basic elements of bone tissue engineering. Scaffolds not only act as a substitute for the extracellular matrix (ECM) but can also serve as the delivery vehicle for cells and the carrier for growth factors 71. “Smart scaffolds” have been designed recently that have physical and chemical properties similar to the tissue to be replaced. Further, they have bioactive molecules and nanoparticles that enhance regenerative potential.
Biomimetic and bionic smart scaffolds:
The term “biomimetic” is derived from Greek, where bios means “life” and mimetikos means “imitative”. Biomimetic materials are materials developed using inspiration from nature (such as natural structures, including the honeycomb structure of the beehive, bird flight mechanics, and shark skin water repellency, etc.). These scaffolds have been designed such that they elicit specified cellular responses mediated by interactions with scaffold-tethered peptides from the extracellular matrix (ECM) proteins; essentially, the incorporation of cell-binding peptides into biomaterials via chemical or physical ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Immune-sensitive smart scaffolds:
It is of prime importance that the scaffold, when placed in the body, should not generate a foreign-body reaction. In other words, the scaffold should have immunomodulatory properties, directing the host response towards tolerance of the foreign scaffolds or regulating immunological microenvironments to promote cell survival. IL-4 has been incorporated in the scaffolds to enable their immunomodulatory capability 73. Incorporation of nanofibrous heparin-modified gelatin microspheres in the scaffold can spatiotemporally deliver the anti-inflammatory cytokine IL-4 to polarize the proinflammatory M1 macrophages into an anti-inflammatory M2 phenotype. It improves the osteogenic potential of the scaffold 73.
Shape-memory smart scaffolds:
Recently, shape-memory smart scaffolds have been described. These scaffold materials have shape memory and they can return from a deformed shape to their original shape by an external stimulus, such as temperature change 74, an electric or magnetic field 75 and light 76. These scaffolds are fabricated by utilizing three-dimensional (3D) and four-dimensional (4D) printing technologies. These scaffolds have gained attention, especially because of extensive research in the field of minimally invasive surgical therapy (MIST). The scaffold with small size is placed in the bone defect using minimally invasive means with the least damage to host tissues. With time the scaffold regains its actual size and precisely fills the bone defect. In a study, BMP2-loaded shape-memory porous nanocomposite scaffold was placed in bone defects in the rabbit model. It was demonstrated that the porous scaffold displayed shape-memory recovery from the compressed pores of 33 μm in diameter to ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Electromechanical-stimulus smart scaffolds:
It has been discovered that biological tissues possess electrical fields. This discovery has led to the development of electrical stimulation therapies 78. The piezoelectric property of certain materials can be utilized to enhance the regenerative potential of the scaffolds. The piezoelectric effect is the ability of a material to generate an electric charge in response to applied mechanical stress. Recently, piezoelectric poly (vinylidene fluoride-trifluoroethylene) (PVDF-TrFE) has been used to ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……..
Critical analysis of present status of tissue engineering in periodontics
Tissue engineering is one of the most extensively researched fields presently. So far we have succeeded in fabricating scaffolds suitable to deliver various bioactive molecules at the sites where tissue regeneration is required. We can isolate the growth factors or synthesize them in vivo. We can expand cell line in tissue cultures and implant them at the site of interest. However, there are many challenges which need to be addressed. These are,
- Various growth factors act through intracellular signaling mechanism once they attach to their corresponding surface receptors. Our knowledge of these intracellular mechanisms is still incomplete.
- The exact mechanism by which the growth factors enhance periodontal regeneration yet remains to be proven in vivo. Although tritiated thymidine and proline labeling studies would yield valuable information regarding in vitro effects of PDGF/IGF-1 80, more research is required in this field.
- Ideally, once delivered at the site of interest, the growth factors should act on their target cells to produce desired effects. However, there are many mechanisms which neutralize or deactivate these growth factors when placed in the biological environment. This issue needs to be addressed.
- Presently, we have insufficient data for the authentication of clinical safety and effectiveness of various newer regenerative techniques provided by tissue engineering.
- Although, growth factors have been found to be useful for periodontal regeneration, their cost-effective application, and easy availability still need to be sorted out.
- Gene therapy has provided us a new technique for regulating cellular activity. However, its safety in the clinical application has still not been well investigated.
- Cell culture media of xenogeneic products (such as fetal bovine serum or mouse feeder layers) always carry a risk of disease transmission.
- Newer identification techniques are required to authenticate the safety of xenogeneic products.
- There are always possibilities of immune rejection of the implanted cell line when allogenic and xenogenic sources of the cell line are used.
- Cell lines need to be well investigated for any immunological reaction. Preferably, autologous stem cells should be used to overcome this problem 81.
- The culturing techniques still need to be improvised to mimic the cell microenvironment in vivo. The culture media should facilitate cell attachment, allow controlled release of bioactive factors, be conducive to tissue ingrowth and facilitate laboratory handling 82.
- One serious problem associated with cell culturing is that with extended duration in culture the cells may undergo genetic or epigenetic changes 83. In recent studies, it has been hypothesized that bone marrow-derived mesenchymal stem cells may result in the development of carcinoma-associated fibroblasts (CAF) which may cause the formation of epithelial solid tumors 84.
Conclusion
There are a lot of questions in the field of tissue engineering, which still need to be answered. Delivery systems which are suitable for their placement in periodontal defects need to be evaluated. More research is required to find out the exact molecular mechanisms involved in the action of various growth factors and other bioactive molecules. Particular attention is required to authenticate the clinical usage of gene therapy. Because gene therapy involves changes in the genetic material, i.e., DNA, both pros and cons need to be analyzed thoroughly before this therapy is implemented clinically for periodontal regeneration.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

