Introduction to endo-perio lesions
The term “endo-perio” lesion has been proposed to describe the destructive lesions resulting from inflammatory products found in varying degrees in both the periodontial and pulpal tissues. The periodontium and dental pulp are inter-linked from embryonic stage. The dental pulp originates from dental papilla and the periodontal ligament originates from dental sac, both of which have a common mesodermal origin. In the late bell stage of tooth formation, the dental sac and dental papilla are separated from each other by epithelial root sheath except at the future apical foramen. At apical foramen, the dental pulp and periodontal ligament communicate with each other. The relationship between the periodontium and the pulp was first discovered by Simring and Goldberg in 1964 1. The interrelation …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Communication between dental pulp and periodontium
As already stated, during tooth development the dental pulp and periodontium communicate with each other at apical foramen. It is the primary route of communication between the pulp and the periodontium. Along with apical foramen, periodontium communicates with pulp tissues through many channels or pathways known as the lateral or accessory canals. Studies of human teeth have shown that the lateral and accessory canals and foramina are present in great numbers, especially in the bifurcation and trifurcation regions of molars 2, 3. It is estimated that 30-40% of all teeth have lateral or accessory canals and the majority of them are found in the apical third of the root 4. One study investigated 1,140 extracted teeth and it was found that 27.4% exhibited accessory canals 5. Another study examined 102 teeth and found that 25.5% of the teeth had accessory canals in the furcation area alone 6. Patent accessory canals can act as a potential pathway for the spread of bacterial and toxic byproducts, resulting in a direct inflammatory process in the periodontal ligament 7, 8.
Other routes of communication between pulp and periodontal tissue include,
Dentinal tubules:
At the cervical area of the root surface, approximately 15,000 dentinal tubules per square millimeter are present 9. These tubules may get exposed due to various reasons such as periodontal disease, scaling, root planning, surgical …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Anatomical communication routes:
Most common anatomical communication route between pulp and periodontium is palatogingival groove. This developmen-tal groove is commonly found in maxillary lateral incisors. It begins in the central fossa or across the cingulum, extending upto varying distances apically 11. It is a developmental anomaly that occurs as developmental infolding of the inner enamel epithelium and Hertwig’s epithelial root sheath (HERS). Embryologically, it is related to a mild form of dens invaginatus, where, the invagination results in a circular opening 12. On radiographs they appear as a “tear drop” shaped area 13 and dark lines parallel or imposed on the root canal can be noticed which are termed as “parapulpal lines” 14. Kogon’s investigations show that the groove can be found in cingulum, followed by lateral fossa, cementoenamel junction, and root in decreasing order. He also found that most common location is in the midpalatal area of lingual surface followed by distal and then mesial 15. Its prevalence ranges from 1.01% to 8.5% independent of the sex 16. The chances of communication between the pulp chamber and periodontium vary according to the depth of the groove. Deeper the groove more are the chances of endo-perio communication. Other anatomical factors which can contribute to endo-perio communication are,
Cemental agenesis/hypoplasia,
Root anomalies,
Intermediate bifurcation ridges, and
Fibrinous communications.
Vertical root fractures:
A tooth fracture in which the fracture line is oriented along the long axis of the tooth is called as a vertical fracture. Any accidental trauma may result in tooth fracture which may involve cementum, dentine, and pulp. The clinical features of vertical root fracture are mobility of the involved teeth, pain on biting, pain on selective loading of the cusps, discomfort, periodontal defect, radiographic bone destruction, and abscess formation.
Classification of pathways of communication between pulp and periodontium
For the ease of understanding, the pathways of communication between pulp and periodontium can be broadly classified into three categories as follows,
Developmental origin
a. Apical foramen.
b. Accessory canals and lateral canals.
c. Congenital absence of cementum exposing the dentinal tubules at the cervical region of teeth.
d. Permeability of cementum.
e. Developmental grooves.
f. Enamel projection and enamel pearls at the cervical area.
Pathological origin
a. Empty spaces on the root created by the destruction of Sharpey’s fibers.
b. Vertical fractures.
c. Idiopathic resorption – internal and external.
d. Loss of cementum due to external irritants.
Iatrogenic origin
a. Exposure of dentinal tubules following root planing.
b. Accidental lateral perforation during endodontic procedure.
c. Root fracture due to endodontic procedure.
Etiology of endo-perio lesions
The most common reason for endo-perio lesions is dental plaque associated inflammation, which may be initiated either in the dental pulp or in the periodontium. The etiological factors for endo-perio lesions may be,
Microorganisms:
Bacteria, fungi, and viruses.
Contributing factors:
Poor endodontic treatment and root canal perforations.
Poor restorations.
Root resorption.
Role of microorganisms in endo-perio lesions:
The primary etiology of endo-perio lesions is micro-organisms. Various studies have investigated the bacterial species associated with periodontal and endodontic infections. One study showed that the bacterial profile of both endodontic lesions as well as in teeth with chronic apical periodontitis and chronic adult periodontitis consisted of Actinobacillus actinomycetemcomitans, Bacteroides forsythus, Eikenella corrodens, Fusobacterium nucleatum, Porphyromonas gingivalis, Prevotella intermedia and Treponema denticola 17. Recent studies …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
A study was done for qualitative and semi-quantitative evaluation of bacteria in endo-periodontal lesions using polymerase chain reaction (PCR) and DNA-DNA hybridization. Possible associations of six bacteria (Parvimonas micra, Fusobacterium nucleatum, Campylobacter rectus, Eubacterium nodatum, Eikenella corrodens and Capnocytophaga sputigena), belonging to ‘orange’ and ‘green’ complexes were evaluated in endo-periodontal lesions. Results showed that extremely high bacterial loads in endodontic samples were recorded for P. micra, F. nucleatum and C. sputigena, while periodontal …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
On the contrary, Kurihara et al. (1995) 20 examined the samples of root canal content and the deepest portion of the periodontal pocket by analyzing their microbiological and immunologic aspects. They observed a significant difference in the microflora of the root canal and periodontal pocket. While the periodontal pocket exhibited a great variety of species, the root canal was limited to Gram-positive coccus, including Peptostreptococcus and Streptococcus, or Gram-positive rods, such as Actinomyces and Rothia.
Fungi also have been isolated from both endodontic and periodontal lesions. The majority of the recovered fungi from endo-perio lesions are Candida albicans. Other fungi species which have been isolated include Candida glabrata, Candida guillermondii, Candida incospicia and Rodotorula mucilaginosa.
Recent studies have shown an association of viruses with periodontitis 21-25. The herpes virus is the most studied viruses isolated from periodontal lesions. It has been proposed that Herpes virus infection may initiate or accelerate periodontal tissue destruction due to virally mediated release of cytokines and chemokines from inflammatory and non-inflammatory host cells, or virally induced impairment of the periodontal defense, resulting in the …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Poor endodontic treatment and root canal perforations:
Poor endodontic treatments are often found associated with peri-radicular inflammation. Re-infection of the root canal results in inflammation in the peri-radicular area causing periodontal damage. Injudicious use of rotary instruments while gaining access to the root canal can result in perforation of the floor or the …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Poor restorations:
Faulty restorations may lead to coronal leakage resulting in endodontic involvement. This may lead to the spread of inflammation in dental pulp and then may involve the periodontal tissue. In root canal treated teeth with faulty restorations, there are more chances of root canal failure. In a study Ray and Trope (1995) 28, reported that defective restorations and adequate root fillings had a higher incidence of failures than teeth with inadequate root fillings and adequate restorations.
Root resorption:
The resorption of the root surface due to the pathological process may result in the endodontic-periodontal lesion. The resorption may be initiated in the periodontium and affect initially …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Spread of inflammation from dental pulp to periodontium
It is well established that the main cause of the periodontal lesions and dental caries is the presence of the bacterial plaque, formed by aerobic and anaerobic microorganisms 29-32. Other reasons of pulpal inflammation include restorative procedures, trauma, chemical irritation and severe thermal stimulation. These inflammatory lesions cause localized edema and a resulting increase in intra- pulpal pressure and cell death. Increased damage associated with an inflammatory exudate cause the local collapse of the venous part of the local microvasculature 33. This causes local tissue hypoxia and anoxia resulting in localized necrosis, the chemical mediators of which cause further localized edema, completing the cycle.
The inflammatory response then progresses to the periodontal ligament at apical foramen and at the opening of the accessory canals 34. This results in “retrograde periodontitis”. Because of the spread of inflammation, the endodontic lesion now becomes an endo-perio lesion. There is widespread destruction of the periodontium and with the due course of time radiolucency at the apex of the tooth or in the furcation or at various points along the root surface can be seen. With the continuous spread of inflammation, there is localized periodontal destruction associated with various signs and symptoms including, periodontal pocket formation, purulent inflammatory exudates, angular bone loss, swelling and bleeding of the gingival …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Spread of inflammation from periodontium to dental pulp
Periodontal pocket formation along the root surface causes attachment loss. There are multiple species of micro-organisms present in a periodontal pocket. The inflammatory response in the periodontium can involve dental pulp. However, the effect of periodontal disease on the pulp is not as clear-cut as the effect of pulpal disease on the periodontium. Reason being, normal pulps have also been observed in teeth with advanced periodontal disease. There are various responses of dental pulp to periodontal inflammation. The initial effect of periodontal inflammation on the pulp may be degenerative. Fibrosis, calcifications, and collagen resorption have been reported in the pulps of teeth with the long-standing periodontal disease.
The progression of periodontal pocket results in the involvement of the root surface. With due course of time, deepened periodontal pocket may result in the involvement of the apical foramen causing pulpal damage. The spread of inflammation into …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
The root surface is covered by cementum and an intact cementum layer is important for the protection of the pulp from pathogenic agents produced by the plaque bacteria 39. Rigorous scaling and root planing for the treatment of periodontal disease may result in removal of the cementum, exposing dentinal tubules. The exposed tubules may allow bacterial invasion and hence, as a consequence, pulp damage may result 40.
| Differences between endodontic and periodontal lesions | |
|---|---|
| Endodontic lesion | Periodontal lesion |
| Pulp is non-vital. | Pulp is vital except in advanced lesion. |
| Associated tooth has sharp throbbing pain. | Associated tooth has dull and chronic pain. |
| Swelling generally extends beyond attached gingiva. | Swelling is generally confined to attached mucosa. |
| Tracing the fistulous tract leads to apical region or in the region or in the region of a lateral canal. | Tracing the fistulous tract leads to middle root. |
| The fistulous tract is narrow and tortuous. | The fistulous tract is wide in the cervical area due to extensive loss of periodontal tissue. |
| Mobility associated with involved tooth in acute stage. | Generalized tooth mobility involving multiple teeth. |
| Bone loss limited to the involved tooth, which may be crestal and furcal. The angular bone loss is usually seen. | Generalized crestal bone either horizontal or vertical. |
Classification of endodontic-periodontal lesions
One of the earliest classifications to classify endo-perio lesions was proposed by Oliet and Pullock (1968) 41. This classification is based on treatment needs and has been used by Grossman 42. According to this classification, endo-perio lesions can be classified into three types,
Type I: Requiring endodontic treatment only.
Type II: Requiring periodontal treatment only.
Type III: requiring combined endo-perio treatment procedures.
Weine 43 classified endo-perio lesions into 4 types based on clinical presentation of cases and offered treatment strategies for each type.
Type I: Primary endodontic lesions mimicking periodontal disease.
Type II: Endodontic lesion in a periodontally involved tooth.
Type III: Primary periodontal lesion requiring endodontic treatment for healing.
Type IV: Primary periodontal lesion secondarily involving the pulp.
The most common classification used to classify endo-perio lesions is Simon’s classification. Simon et al. (1972) 44 classified the lesions based on the primary source of infection and its spread through anatomical pathways. They categorized these lesions into five types,
Type I: Primary endodontic lesions.
Type II: Primary endodontic lesions with secondary periodontal involvement.
Type III: Primary periodontal lesions.
Type IV: Primary periodontal lesions with secondary endodontic involvement.
Type V: True combined lesions.
The major difference between Weine’s and Simon’s classification is their description of Type II lesions. According to Weine’s classification Type II lesions are those having an endodontic lesion in …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book ……
Many other classifications of endo-perio lesions also have also been proposed such as “independent periodontal and endodontic lesions” 9 or “concomitant pulpal and periodontal lesions” 45, 46 to describe endodontic-periodontic lesions.
Let us now discuss Simon’s classification of endo-perio lesions,
Primary endodontic lesion (Type I):
The primary endodontic lesion results from the necrotic degeneration of the pulp, extending apically resulting in apical periodontitis. It may drain coronally through the periodontal ligament into the gingival sulcus. The clinical appearance of the condition mimics a periodontal abscess. However, it is actually a sinus tract originating from the pulp that opens into the periodontal ligament. The root canal treatment results in complete healing with the disappearance of drainage sinus in the early stage of the treatment.
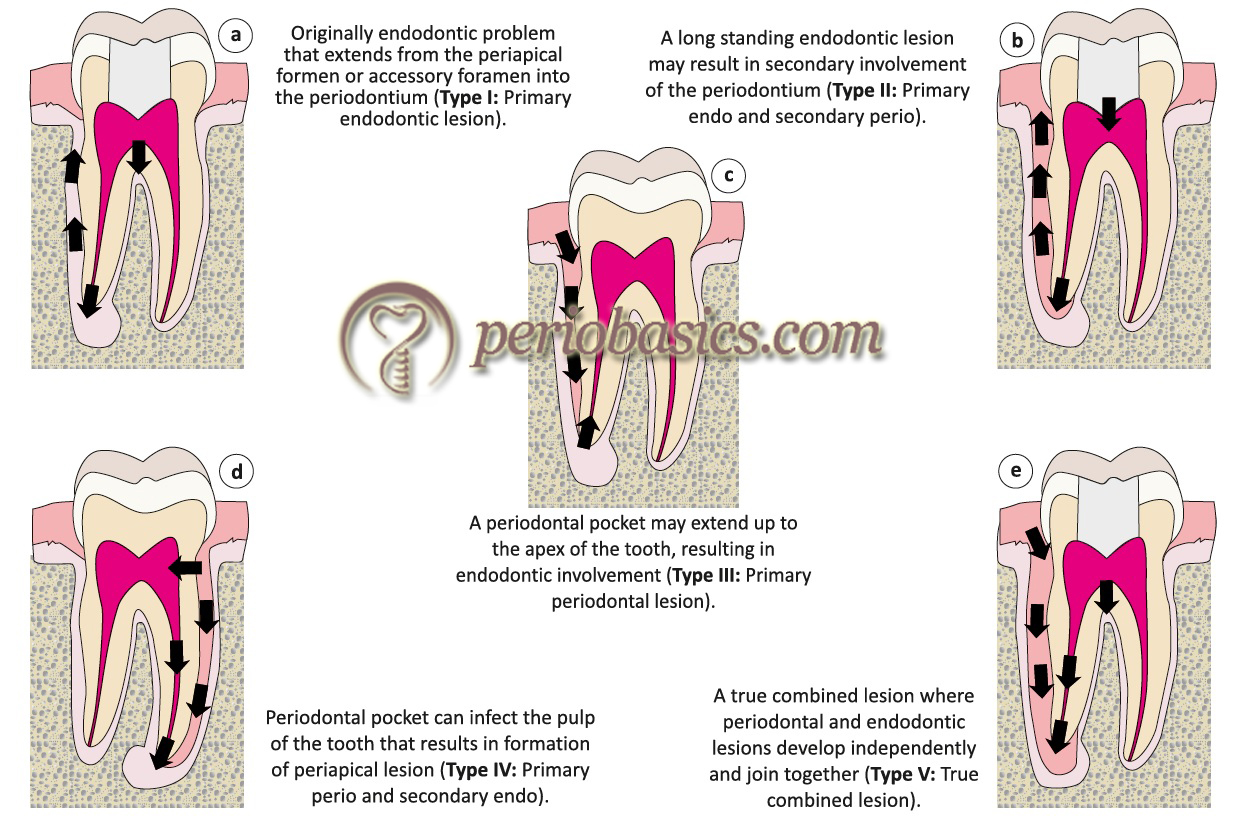
Primary endodontic lesion with secondary periodontal involvement (Type II):
In this case, the endodontic lesion is long-standing, which results in a chronic periapical lesion with drainage through gingival sulcus. The draining track from the sulcus becomes superimposed by plaque and calculus resulting in the pocket formation and apical migration of epithelial attachment. An angular bone loss can be seen in radiographs …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Primary periodontal lesion (Type III):
The primary periodontal lesion results from the periodontal pocket formation which progresses apically to involve dental pulp. In most cases, pulpal tests indicate a clinically normal pulpal reaction. The involved tooth is associated with a true periodontal pocket. Periodontal treatment resolves the condition and endodontic treatment is not required as the pulp is vital.
Primary periodontal lesion with secondary endodontic involvement (Type IV):
This type of lesion is associated with extensive periodontal destruction which may have been treated. The tooth is associated with deep periodontal pocket with the patient giving a history of chronic periodontal problem in that area. The deepened periodontal pocket results in the involvement of pulp through accessory canals, open dentinal tubules or apical foramen. When the pulp becomes involved the patient reports accentuated pain and clinical signs of pulpal disease. The damage to the pulp is irreversible, which can be confirmed by pulp vitality tests. Radiographically these lesions are similar to primary …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
True combined endodontic and periodontic lesions (Type V):
These lesions are relatively infrequent, but when present, may have significant periodontal involvement with considerable attachment loss. In this case, there are two independent endodontic and periodontal lesions which merge to form a combined lesion 51-55. The pulp vitality tests indicate pulp necrosis and periodontally deep pockets are present. Radiographically, these lesions …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Diagnosis of endo-perio lesions
The diagnosis of an endo-perio lesion is made with the help of visual examination, palpation, percussion, radiographic examination, and fistula tracking.
Visual examination:
The involved tooth and its associated gingiva are thoroughly examined for the presence of inflammation, ulcerations or sinus tracts. Usually, a draining sinus track is associated with the involved tooth, which should be diagnosed by visual examination.
Palpation:
The mucosa covering the roots and apices of the involved teeth is palpated by applying firm digital pressure with a finger. Any peri-radicular abnormality can be detected by palpation such as swelling and fluctuant abscess collection in the tissue.
Percussion:
The vertical and lateral percussion should be done to evaluate the periodontal and periapical tissue condition. Tenderness on lateral percussion is positive in periodontal inflammation on the lateral surface of the tooth whereas tenderness on vertical percussion is positive in apical periodontitis.
Tooth mobility:
Tooth mobility is an indicator of the integrity of periodontal attachment apparatus. In the case of primary endodontic involvement, hypermobility is usually present, which disappears within a week of initiating endodontic therapy. Tooth mobility resulting due to loss of periodontal support in case of periodontal lesion varies according to the severity of periodontal destruction.
Radiographs:
Radiographic examination plays an important role in the determination of location and pattern of bone loss around the involved teeth. In lesion of endodontic origin, the periapical bone loss is evident. In the case of periodontal disease, the crestal bone loss can be seen which extends apically according to the severity of periodontal disease. However, when the radiograph shows bone loss extending from the level of crestal bone to or near the apex of the tooth, it becomes difficult to determine the cause 56-58.
Pulp testing:
In the endodontic involvement of the tooth, the pulp vitality tests such as cold test, electric test, blood flow tests and cavity test provide valuable information regarding the status of the pulp. These results of tooth vitality test are more accurate in teeth with single canal. However, in case of teeth with multiple canals, the accuracy of pulp vitality tests reduces in determining the presence or absence of vital tissue in the root canals 59.
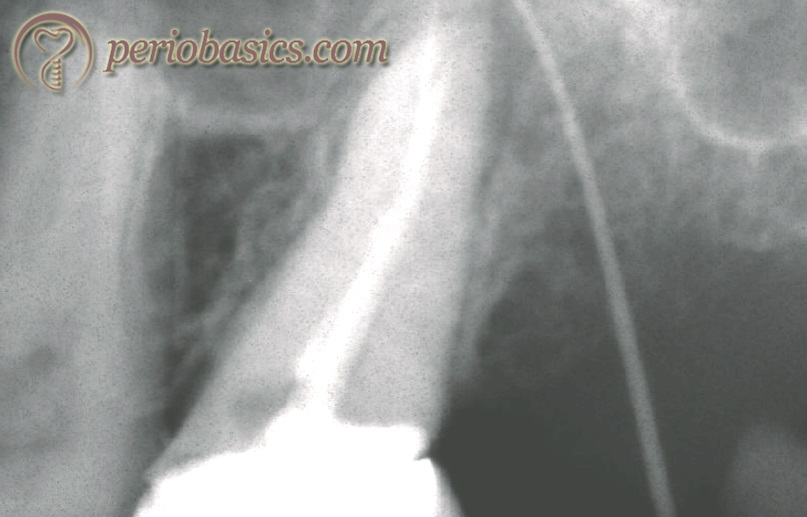
Fistula tracking:
A sinus tract is formed for the drainage of inflammatory exudates. It is formed through the structures of minor resistance and open anywhere on the oral mucosa or facial skin. It can be seen in the buccal vestibule in attached gingiva or alveolar mucosa. A fistula tracking is done by inserting a semi-rigid material like a gutta-percha cone from its opening in the buccal vestibule until resistance is met. After inserting GP cone, a radiograph is taken which shows the exact location of the source of this inflammatory exudate 52.
Prognosis
The prognosis of an endo-perio case to a great extent depends on the periodontal status. If the disease is primarily pulpal and there is minimal periodontal involvement, the prognosis is good or excellent. But, if the disease is primarily periodontal with secondary involvement of pulp, the prognosis depends on the status of the periodontium. Reason being in primary endodontic disease, the lesion completely resolves after root canal debridement and disinfection whereas in primary periodontal …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Management of endo-perio lesions
The management of an endo-perio lesion should follow a thorough clinical and radiographical examination. The primary or secondary involvement of the pulp or the periodontium should be determined. If the primary disease of one tissue is present and the secondary involvement of the other tissue is just starting, the primary disease should be treated. It usually resolves the secondary involvement of other tissue.
General aspect of treatment planning:
The prognosis of the involved tooth should be considered before the commencement of any kind of advanced restorative work to treat an endo-perio lesion. Many factors should be considered while determining the prognosis such as whether there is furcation involvement, which needs to be addressed, whether the tooth is …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Another rule of thumb is wherever endodontic treatment is indicated with periodontal therapy; the best sequence of treatment is that endodontic treatment should precede periodontal therapy. It has been shown that after debridement and disinfection of the root canal, reattachment of the soft tissue after periodontal therapy is improved 60.
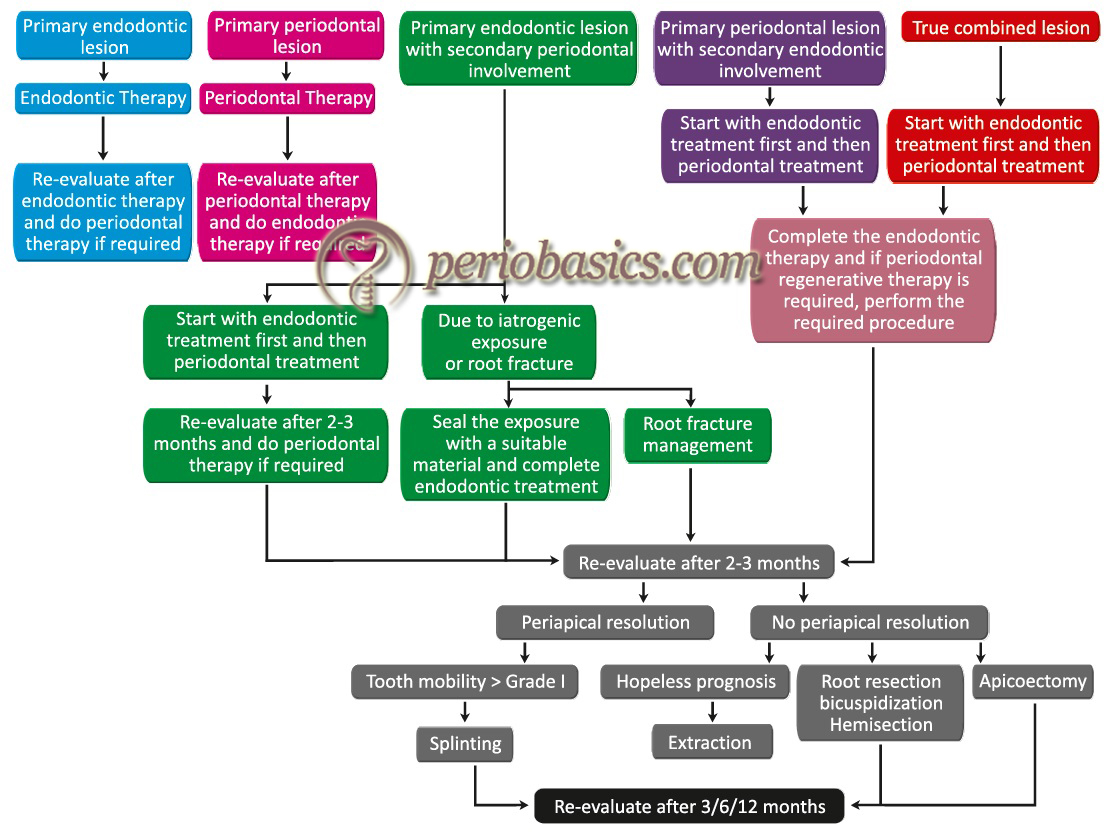
Let us now discuss treatment protocol in different types of endo-perio lesions,
Treatment of primary endodontic and secondary periodontal involvement:
In the majority of cases, the endodontic treatment precedes the periodontal treatment. When the disease is endodontic in origin and periodontal involvement is secondary, endodontic treatment resolves the periodontal disease in most of the cases. Surgical endodontic therapy is not necessary, even in the presence of large peri-radicular radiolucencies and periodontal abscesses. Periodontal treatment may not be required in these cases. Despite extensive endodontic treatment, if primary endodontic lesions persist, the lesion may have secondary periodontal involvement or it may be a true combined lesion.
However, it must be remembered that to what extent the periodontal tissue has been destroyed cannot be determined clinically. So, there should be an observation period after debridement and disinfection of the root canal system to assess the periodontal healing. Within a couple of weeks, the periodontal pocket depth should reduce and clinical features of …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
If the endodontic involvement is well established, first the root canal therapy is instituted and after the debridement and disinfection of the root canal, calcium hydroxide paste is filled in the canal. Calcium hydroxide has bactericidal, anti-inflammatory and proteolytic property, inhibiting resorption and favoring repair. It also has an inhibitory effect on contamination of root canals from periodontium via patent accessory canals. The tooth is then observed for next 2-3 months and afterward, if required periodontal therapy should be initiated.


Treatment of primary periodontal and secondary endodontic involvement:
When primary periodontal involvement is there with secondary endodontic involvement, the treatment depends on the clinical presentation of the case. In acute pain which is usually of endodontic origin, root canal debridement and disinfection is initiated first. Simultaneously, periodontal therapy is initiated to eliminate the plaque and calculus, thus reducing bacterial load in the periodontium.
In the case of primary periodontal involvement and initial endodontic involvement, non-surgical periodontal therapy is initiated with scaling and root planing. The root canal therapy is not indicated unless pulp vitality test results show changes. If pulp pathology is suspected, root canal treatment should be initiated along with periodontal therapy. After completion of the non-surgical periodontal therapy, the surgical phase is initiated. Various procedures which can be performed depending on case to case include gingivectomy, apically displaced flap, new attachment techniques, and hemisection or root resection.
If endodontic treatment has not been done, after completion of the periodontal therapy, the patient is re-evaluated for possible retrograde endodontic problems. In these cases, the prognosis entirely depends upon …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Treatment of true combined lesion:
The true combined lesion is treated in the same way as the primary endodontic lesions with secondary periodontal involvement. The prognosis of a true combined endo-perio lesion is often poor or even hopeless, especially when periodontal lesions are chronic, with extensive loss of attachment. Depending upon the clinical presentation of the case, the non-surgical periodontal …… Contents available in the book …… Contents available in the book …… Contents available in the book …… Contents available in the book …..
Treatment of iatrogenic lesions:
The iatrogenic lesion such as perforation during root canal instrumentation requires sealing of the perforation. If a perforation happens during root canal treatment or post and core treatment, it can be sealed by placing zinc oxide eugenol, glass ionomer or mineral trioxide aggregate sealing material immediately.
Conclusion
Endodontic-periodontal lesions commonly present a dia-gnostic and treatment dilemma. Sometimes it becomes really difficult to determine the primary source of infection in a combined lesion, i.e. periodontal or endodontic. However, with careful diagnosis and treatment planning, in most of the cases, the involved tooth/teeth can be saved with a good prognosis. Some cases may require only endodontic therapy or periodontal treatment while others may require a combined approach. The re-evaluation of eno-perio cases is essential to find out any remaining infection in endodontic or periodontal region. Periodic necessary treatment should be provided to the patient as indicated.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

