Introduction to oral manifestations of HIV
The oral manifestations of HIV infection are important components of AIDS. These are seen in approximately 30 to 80 percent of the affected patient population 32-34. There are various factors which predispose an HIV-infected patient for oral lesions. These include CD4 counts < 200 cells/mm3, viral load > 3000 copies/mL, xerostomia, poor oral hygiene and smoking 35, 36. The oral manifestations include fungal, bacterial or viral infections, neoplasms or non-specific lesions.
Fungal infections
The fungal infections are commonly seen in immunocompromised patients, especially suffering from AIDS. The most common fungal infection of the oral cavity in AIDS patients is Candidiasis. Other less common fungal infections include Histoplasmosis, Cryptococcosis, Coccidioidomycosis and Linear gingival erythema.
Candidiasis
The oropharyngeal candidiasis is the most common fungal infection seen in AIDS patients 37, 38. Candida albicans is the predominant causative agent of all forms of mucocutaneous candidiasis. Other Candidal species which may be associated with candidiasis are C. glabrata, C. parapsilosis, C. tropicalis and C. krusei. The presence of oral candidiasis is significantly associated with lower CD4 : CD8 ratio and a reduced CD4 cell count below 200 cells/mm3 (39, 40). The oral candidiasis is frequently seen in three different forms: erythematous candidiasis, pseudomembranous candidiasis, and angular cheilitis. In patients with full-blown AIDS, the ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Clinically, it appears as a red, flat, subtle lesion either on the dorsal surface of the tongue and/or the hard/soft palates. The pseudomembranous candidiasis is characterized by creamy white curd-like plaques on the buccal mucosa, tongue, and other oral mucosal surfaces that can be wiped away, leaving a red or bleeding underlying surface. Another form of candidiasis, hyperplastic candidiasis is differentiated from the pseudomembranous candidiasis by the clinical feature that the white plaques cannot be removed by scraping and is common on the buccal mucosa and lateral border of tongue. Pseudomembranous candidiasis should be differentiated from oral hairy leukoplakia, which is usually located at the sides of the tongue and cannot be scraped off. The angular cheilitis is characterized by cracking, peeling, or ulceration involving the corners of the mouth. This form of candidiasis is commonly present with other forms of candidiasis. The patient is more likely to be symptomatic with complaints of burning pain while eating spicy foods or drinking acidic beverages.

Diagnosis:
The diagnosis of candidiasis is made by exfoliative cytology by utilizing 10% potassium hydroxide (KOH) slide preparation of a scraping from an active lesion and/or periodic acid-Schiff / Papanicolaou-stained preparations which demonstrate fungal pseudohyphae. A positive exfoliative cytology is most commonly seen with a smear of pseudomembranous candidiasis 43. Culture is not routinely indicated, but if performed, it identifies the Candida species and helps to predict resistance. It also helps in determining the drug resistance in case of recurrent and refractory infections.

Treatment:
In mild to moderate cases of both erythematous and pseudo-membranous candidiasis, topical agents including clotrimazole troches, nystatin oral suspension, and nystatin pastilles are used. It should be remembered that regular nystatin oral suspension contains 50% sucrose, which is cariogenic. On the other hand, clotrimazole oral treatment is formulated with fructose, which is less cariogenic.
In severe cases, systemic anti-fungal therapy is given. Most widely used systemic anti-fungal drug is fluconazole. Other drugs are itraconazole and voriconazole. Voriconazole is given in cases of resistance to fluconazole. The golden rule to be remembered while giving local or systemic anti-fungal therapy is that therapy must be continued for at least 2 weeks in order to reduce organism colony-forming units to the levels low enough to prevent recurrence 44.
The introduction of ‘azoles’, most importantly fluconazole has led to increased incidences of resistant Candida albicans as well as the emergence of non-albicans species such as Candida glabrata, which are inherently resistant to this class of drug 45. Other factors which are associated with the development of azole-resistant strains of Candida include ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Refractory Candidiasis
Refractory candidiasis refers to candidiasis which fails to respond to antifungal treatment with appropriate doses for a standard duration of time 48. The most clinically significant refractory candidiasis is fluconazole-refractory disease which is associated with significant morbidity. The factors associated with refractory candidiasis are advanced HIV disease (CD4 lymphocyte counts <50 cells/µL) and previous exposure to chronic antifungal therapy 48. The treatment of refractory candidiasis is often difficult, especially when the patient becomes unresponsive to the treatment over a period of time. In the management of an unresponsive case, the most important step is to identify the drugs that have already been tried on the patient with their dosage, whether with that dosage the condition was resolved or increasing the dosage was required to resolve the condition. Generally, patients who are not responsive to ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Histoplasmosis
Histoplasmosis is caused by inhalation of H. capsulatum microconidia into the lungs. After inhalation, the micro-conidia rapidly convert to the yeast phase within the lung parenchyma. In patients with an appropriate cell-mediated response, the infection remains focused with either caseating or noncaseating granuloma formation. In patients with a defective cell-mediated response and in HIV-infected individuals, particularly those with lower CD4 counts, the infection spreads widely in the body. Within next two to three weeks the infection spreads throughout the reticuloendothelial system. It has been proposed that in an attempt to clear the infection, macrophages phagocytose the yeast and carry them to regional lymph nodes 49.
Oral manifestations:
Oral lesions are rarely seen in histoplasmosis and are more frequent with disseminated histoplasmosis. Goodwin et al. (1980) 50 have shown that up to two-third of patients with chronic disseminated histoplasmosis have oropharyngeal involvement. The most commonly affected areas are buccal mucosa, tongue, palate, gingiva, and lips 51-54. It has also been reported that patients with initial oropharyngeal involvement, subsequently developed disseminated disease. Hence, periodic re-evaluation is ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Diagnosis:
The diagnosis of histoplasmosis is based on clinical findings, histopathology, cultures, serologic test, including complement fixation test, immunodiffusion, and histoplasmin skin test. A positive culture provides the strongest evidence for the disease, but the culture is mostly positive in chronic disease rather than after the initial infection. In HIV-infected patients, the serological tests are of limited significance due to less production of antibodies. In these patients, direct immunofluorescence is the test of choice for diagnosis 57.
Treatment:
In immunocompetent patients, the disease is self-limiting 53. In HIV-infected patients with disseminated histoplasmosis, the mortality rate is high. Many of these patients are those who have never received ART before the diagnosis with histoplasmosis 58-60. The prophylactic treatment should be given to those patients who have advanced HIV infection and who live in areas where histoplasmosis is highly endemic 61. A prophylactic dose of itraconazole, 200 mg daily can be considered for patients with CD4 counts <150 cells/mm3. The prophylactic treatment can be stopped if the CD4 counts remain >150 cells/mm3 for 6 months. The treatment of the disease involves administration of IV liposomal amphotericin B (3 mg/kg daily) for at least 2 weeks or until the patient clinically improves. In the case of less severe disease, oral itraconazole, 200 mg 3 times daily for 3 days followed by ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Cryptococcosis
In HIV-infected patients, this disease is most commonly caused by Cryptococcus neoformans, but occasionally by Cryptococcus gattii. The presence of C. neoformans is worldwide whereas C. gattii is commonly found in Australia and similar subtropical regions and in the Pacific Northwest. C. neoformans is encapsulated round-to-oval yeast. It is surrounded by a polysaccharide capsule ranging in size from 1 to >30 microns, when cultivated in the laboratory 67. It has been proposed that this fungal infection occurs via inhalation of the basidiospores or unencapsulated forms, leading to colonization in the airways and subsequent respiratory infection 68, 69. The absence of an intact cell-mediated response in patients with severe HIV infection results in systemic dissemination and increased cryptococcal burden. Following systemic dissemination, the disease may involve any organ of the body. Cryptococcosis in ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Oral manifestations:
The oral cavity is rarely involved in cryptococcosis and only a few case reports are available in the literature so far 71, 72. The lesion clinically appears as ulceration in the oral mucosa, but a definitive diagnosis cannot be made depending on the clinical appearance of the lesion, since microbial infections and trauma may have a similar clinical appearance. Definitive diagnosis is made by taking a biopsy of the lesion and its examination.
Diagnosis:
The diagnosis of cryptococcosis is made by blood/CSF (cerebrospinal fluid) culture, CSF microscopy with India ink staining, or cryptococcal antigen (CrAg) detection. In HIV-positive patients having a cryptococcal infection, the blood cultures are positive in approximately 55% of all blood cultures and the CSF cultures are positive in approximately 95% of all CSF cultures. Within 7 days, visible colonies can be seen in the culture.
Treatment:
The drugs of choice for the treatment of cryptococcosis are amphotericin B, flucytosine, and fluconazole.
Coccidioidomycosis
Two fungal species implicated in causing coccidioidomycosis are Coccidioides immitis and Coccidioides posadasii. These fungi grow as a mold in the soil and develop hyphae in their saprobic form, producing arthroconidia. The inhalation of these arthroconidia leads to the infection in both humans and animals. In immunocompetent patients, this pulmonary infection is self-limiting but in immunocompromised patients such as in HIV infection, the disease may present as a fulminant, disseminated infection.
Oral manifestations:
The oral lesions are rarely present in this disease. The lesion may be ulcerative or nodular, commonly involving tongue and buccal mucosa. The ulcers are often deep with indurated borders and may mimic carcinoma.
Diagnosis:
The diagnosis of this condition is made on the basis of microscopic examination of the involved tissue, culture, serologic test and a coccidioidal skin test conversion from negative to positive after the onset of clinical signs and symptoms 73. The microscopic examination ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Treatment:
Amphotericin B has been used traditionally for the treatment of coccidioidomycosis. Once the acute symptoms of the disease subside, lifelong suppressive therapy with keto-conazole (400 mg/day orally) or fluconazole (400-600 mg/day orally) must be instituted in immunosuppressed patients to prevent relapses.
Linear gingival erythema (LGE)
LGE is also referred to as “red band gingivitis”. The LGE is limited to the soft tissue of the periodontium and clinically appears as an erythematous linear band that extends approximately 2 mm to 3 mm from the free gingival margin. The area with the red band may or may not be associated with bleeding or discomfort. The anterior teeth are most commonly associated with this condition, but it may extend to posterior teeth also. The disease may also appear as a diffused erythematous zone from the gingival margin into the vestibule. The LGE is not significantly associated with dental plaque. Bleeding is usually present after gentle probing. It has been demonstrated that there may be a relationship between LGE and presence of subgingival colonization of Candida species in patients with HIV infection 74. The latest classification of periodontal diseases by the American Academy of Periodontology has also grouped this condition under “gingival disease of fungal origin” 75……….. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Treatment:
The treatment includes professional oral prophylaxis and improved maintenance of at home oral hygiene. Twice-daily rinse with 0.12% chlorhexidine gluconate suspension for 2 weeks is recommended in these patients.
Gingival and Periodontal Diseases
Periodontitis
The development of periodontitis is a result of host-microbial interaction resulting in the destruction of periodontal supporting structures. In HIV infection, the host immune system is compromised because of which the microbial component of the host-microbial interaction overrides the host response, resulting in the progressive destruction of periodontal tissues. A lot of research has been done to understand the exact etiopathogenesis of periodontitis in HIV-infected patients. The first and foremost question to be addressed is if the subgingival microbiota in HIV-positive patients different from uninfected individuals.
The results of studies which have investigated the subgingival microbiota in HIV-positive patients and uninfected individuals have provided quite diverse findings. Some studies have shown a higher prevalence of putative periodontal pathogens such as Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Fusobacterium nucleatum, Tannerella forsythia, Prevotella intermedia and Treponema denticola, in HIV-positive patients as compared to uninfected patients 76-79. On the other hand, some other studies have shown no significant difference between the subgingival microbiota in HIV-positive and uninfected patients 80-84. Studies have also demonstrated some uncommon microbial species in HIV-infected individuals which are not commonly seen in uninfected individuals. These include Enterobacter faecalis 80, 82, Clostridium clostridioforme 80, Klebsiella pneumoniae 80, 82, 85, Clostridium difficile 80, 82, Mycoplasma salivarium 80, 82, 86, Pseudomonas aeruginosa 82, Enterobacter cloacae 82, 85, Candida spp. 87 and Acinetobacter baumannii 88.
However, the role of these uncommon microbial species in the etiopathogenesis of periodontitis in HIV-infected patients is not clearly understood. T. forsythia, P. gingivalis and P. intermedia which are considered as putative periodontopathogenic bacteria, have also been investigated for their presence in HIV- infected and uninfected individuals. The results of the studies are again variable. Some studies suggest that ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
The second aspect of periodontitis in HIV-positive patients is the immune response and the question addressed is regarding any significant difference in the immune response against periodontopathogens in HIV-infected patients as compared to uninfected individuals. It has been well established that most of the connective tissue destruction in periodontitis is caused by host response 92, 93. In HIV-positive patients, higher levels of pro-inflammatory mediators have been detected in GCF and their levels in GCF have been suggested as prognostic factors for the progression of tissue destruction in these patients. Studies have reported significantly increased levels of interferon-γ 94, prostaglandin E2 (PGE2) 95 and matrix metalloproteinase -1 (MMP-1) in HIV-positive patients.
Necrotizing ulcerative gingivitis and periodontitis
The necrotizing ulcerative gingivitis (NUG) is a non-contagious infection of the gingiva characterized by gingival necrosis, bleeding, and pain. Acute necrotizing ulcerative gingivitis (ANUG) is the acute presentation of NUG, which is the usual course the disease takes. Necrotizing ulcerative periodontitis (NUP) may be an extension of NUG into the periodontal structures resulting in attachment loss. However, many authors suggest that NUG and NUP may be different diseases. The primary pathogens for this disease are anaerobic bacteria such as P. intermedia and Fusobacterium as well as spirochetes, such as Treponema. Along with this fungal species have also been isolated from ANUG/ANUP lesions.

The characteristic feature of the disease is ulceration of the interdental papillae which rapidly progresses to the destruction of underlying alveolar bone. There is spontaneous bleeding from the lesion and it is associated with severe pain. In highly immunocompromised patients, extensive destruction of tissue is seen which involves exfoliation of teeth within 3-6 months of disease onset, with the sequestration of necrotic alveolar bone and necrotic involvement of the adjacent mandible and maxilla. A detailed description of the management of ANUG/ANUP patients has been given in “Acute gingival and periodontal lesions”.
Viral infections
Herpes Simplex
The etiological agent of herpes simplex is herpes simplex virus (HSV) which belongs to herpesviridae family. The herpesviridae family consists of viruses responsible for various diseases in humans. There are eight known human herpesviruses (HHV). The viruses in the herpesviridae family have been divided into α, β, and γ herpesviridae subfamilies on the basis of their biological properties including host range, replication cycle and cell tropism 96. The herpes simplex viruses (HSV)-1 and -2 (HHV-1 and HHV- 2), and varicella-zoster virus (VZV; HHV-3) belong to α subfamily. Cytomegalovirus (CMV; HHV-5), HHV-6 variants A and B, and HHV-7 belong to β subfamily. Epstein-Barr virus (EBV; HHV-4) and Kaposi sarcoma-associated herpesvirus (KSHV; HHV-8) belong ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
The HSV-1 infection is acquired in the childhood and is responsible for orolabial ulcers. HSV-2 causes anogenital ulcers and is transmitted sexually. However, HSV-2 associated oral lesions and HSV-1 associated genital lesions are also seen which are caused due to orogenital sexual practice. Once infected, the individual harbors the infection throughout life because the virus becomes permanently latent in the nerve root ganglia corresponding to the site of inoculation of the virus (the trigeminal ganglia for orolabial infection and the sacral ganglia for genital infection). A detailed description of HSV-induced oral ulcers is available in “Acute gingival and periodontal lesions”.
Many recent studies have suggested that genital HSV-2 is facilitating the acquisition of HIV-1 infection. In a meta-analysis, it was concluded that HSV-2 infection increases the risk of HIV-1 acquisition approximately 3-fold in both men and women and individuals with primary HSV infection are even more susceptible to HIV-1 infection 101.
Clinical manifestations of HSV in HIV-infected patients:
The HSV reactivation among the HIV-1-infected individuals clinically presents with vesicular and ulcerative lesions of the oral and anogenital areas which are similar to as seen in HIV-1-uninfected individuals. The anogenital lesions in HSV reactivation may often remain unrecognized because early lesions are small and may manifest as hypersensitive erythematous papules in the case of perianal internal lesions in women, which are difficult to visualize. The declined CD4 count is ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book………..
Treatment:
The anti-viral agents recommended in HSV infection include nucleoside analogs such as acyclovir, valacyclovir, and famciclovir. These agents inhibit HSV-1 and HSV-2 replication through specific inhibition of a virally encoded thymidine kinase.
Varicella-Zoster
Varicella-zoster virus (VZV) belongs to the herpesvirus family. Like other herpesviruses, VZV has the capacity to persist in the body after the primary (first) infection, as a latent infection. VZV persists in sensory nerve ganglia. Its primary infection causes chickenpox in children and reactivation results in herpes zoster (shingles). The clinical presentation of varicella in children infected with HIV is usually similar to that seen in immunocompetent children. However, the duration of the lesion formation is longer and resolution is delayed in HIV-positive patients 104-106. Also, the reactivation of the infection is more common in HIV infected immuno-compromised individuals as compared to healthy immuno-competent individuals. The most common complication in immunocompromised individuals with varicella is cutaneous bacterial super-infections 107.
In HIV-infected adults, the chances of herpes zoster are much more as compared to non-infected individuals. It has been reported that the incidence rate of herpes zoster among HIV-infected patients is 30-50 cases per 1000 persons/years 108-110. The usual presentation of herpes zoster among HIV-infected patients is similar to that of uninfected individuals with one sticking difference which is a higher frequency of shingles recurrences. It has been reported that around 20%-30% of HIV-infected patients develop one or more subsequent episodes of herpes zoster which may involve same or different dermatomes 108, 110. Further, these patients ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Oral lesions:
Intra-oral vesicles of varicella, when present, are seen on the tongue, buccal mucosa, gingiva, palate, and oropharynx. They generally are not very painful. After resolution of the condition, the virus becomes latent in the sensory ganglia. Reactivation of the virus is characterized by pain and tenderness in the dermatome, corresponding to the affected sensory ganglion. The facial and oral presentation of the disease is characterized by the formation of vesicles on the side of the face or in the oral mucosa in one of the divisions of the trigeminal nerve. These painful vesicles end abruptly in the midline. The vesicles ulcerate within three to four days and form pustules. Healing takes place within 7-10 days with scar formation with hypo/hyperpigmentation areas.
Treatment:
The primary drugs used for the treatment of VZV infection is acyclovir (800 mg, administered 4 times per day). Preferably, treatment should begin as soon as possible (within 72 hours of onset of skin rash) and continued for at least 7 days or until all lesions have dried and crusted. In the case of disseminated VZV infection, intravenous administration of acyclovir is recommended.
Human Papillomavirus (HPV)
Human papillomavirus (HPV) is one of the most common agents of sexually transmitted diseases worldwide 116. More than 50 strains of HPV exist. The most common genotypes found in the mouth of patients with HIV infection are 2, 6, 11, 13, 16 and 32. Studies have found an increased prevalence of HPV in individuals who are also HIV-infected 117. It has been demonstrated that in immunocompetent individuals, abnormalities such as papillomas associated with HPV are uncommon. However, in HIV-infected immunocompromised patients, oral mucosal abnormalities such as papillomas are more common 118. The HPV infection is primarily ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Cytomegalovirus (CMV)
CMV is usually an uncommon cause of intraoral ulceration in patients with HIV disease. It must be noted that intraoral ulcerations with CMV are indicative of systemic dissemination of CMV infection 121. The early diagnosis of CMV infection is important because of the serious consequences of systemic involvement such as retinitis and meningitis. In around 90% of the patients who die because of AIDS, CMV has been detected in one or more organ systems 122. In the oral cavity, CMV lesions may be present as a single large necrotic painful ulcer and less often as multiple ulcers, present for weeks or months and any site may be involved 123. The most common sites involved are buccal and labial mucosa. Often the ulcerations are indistinguishable from the non-specific ulceration caused due to chronic HSV and major aphthous ulceration. It has been suggested by some authors that ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Oral hairy Leukoplakia (OHL)
OHL is an Epstein-Barr virus (EBV)-associated disease which is almost exclusively seen in people with immunosuppression, particularly in HIV-infected individuals. The disease was first observed in 1981 and reported in 1984 as a common, benign, asymptomatic, white, non-removable lesion of the lateral borders of the tongue in patients with HIV infection 128. The lesions cannot be rubbed off and are mostly symptomless. It occurs in up to 50% of the patients with untreated HIV, particularly those with CD4 count less than 0.3 × 109/L 129.
Clinical features:
OHL lesions are often bilateral or sometimes unilateral, white or gray patches which cannot be rubbed off, present mainly on the lateral lingual margins and sometimes on the dorsum or ventrum of the tongue. The term ‘hairy’ used to describe this leukoplakia signifies corrugated appearance or projections (hairy projections) on the surface of white patches. Lesions on the inferior surface of the tongue are flat. Most commonly the lesions are asymptomatic but in some cases, patient complains of burning sensation 130.
Etiopathogenesis:
Although exact etiopathogenesis of OHL still needs to be elucidated, EBV infection facilitated by immunodeficiency in HIV-infected patients has been suggested to be the primary etiology of this disease. EBV is acquired by over 90% of the world population during childhood/adolescence. Following infection, the infected individual remains a carrier for a lifetime. The virus is shed in saliva. It has been proposed that ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Evidence for the involvement of EBV in the etiopathogenesis of OHL comes from immunohistochemical 133, 134 analysis and EBV-DNA identification using molecular techniques such as Southern blotting and in situ hybridization (ISH) 134-137, which have demonstrated EBV antigens in the tissue sections. Studies have demonstrated herpes virus particles in the intercellular spaces using negative staining electron microscopy on thin tissue sections 128, 135, 138, 139. The transcripts expressed from the EBV BHLF1 and BCRF1 genes, which in cultured lymphoid cells are associated with the lytic replication cycle, have also been demonstrated indicating active viral replication 140. Further, it has been demonstrated that hyperplasia and acanthosis seen in OHL are directly related to the combined action of EBV-encoded proteins.
Experiments done on transgenic mice expressing the EBV BNLF-1 gene product, latent membrane protein-1, have been shown to develop lingual epithelial hyperplasia associated with expression of hyperproliferative keratin 6 141. The OHL tissue has also been demonstrated to express BHRF1 which is an immediate early protein bearing homology to the antiapoptotic Bcl-2 oncogene. This protein has been shown to delay the terminal differentiation of cells in squamous cell carcinoma cell line when this protein is transfected into these cells 142. This is an effective strategy developed by EBV in order to facilitate its intense replication in the host cells without lysis of these host cells. However, the exact mechanism of initiation of OHL by EBV has not been elucidated yet.
Another possible etiological agent is Candida. Around 43% to 80% of the OHL lesions have demonstrated candidal hyphae 136, 138, 143. However, aggressive antifungal therapy ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Histopathology:
Microscopic examination demonstrates ballooning degeneration of the keratocytes of the upper stratum spinosum, hyperkeratosis, and mild or absent subepithelial inflammation. Keratinized ”hair-like” projections can be seen. Koilocytosis with pyknotic nuclei and perinuclear halos in the prickle cell layer are visible. Intranuclear inclusions can be seen. Frequently, Candidal hyphae and leukocytes surrounding the hyphae can be seen in the histological section 133, 143.
Diagnosis:
Whenever a patient with clinical finding of OHL comes to the clinician, it is mandatory to go for the evaluation of the immune status of the patient. If the immunosuppression is diagnosed, further investigations should be done to find out the underlying cause of immunosuppression. Provisional diagnosis can be made, based on ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Definitive diagnosis of the OHL is made by the detection of replicating EBV in tissue. In most instances in situ hybridization of biopsy specimens with the use of EBV-specific DNA probes to detect EBV antigens is adequate. The findings from exfoliative cytology demonstrate nuclear beading in the vacuolated or ballooned squames which indicate viral replication. The exact diagnosis requires ultrastructural examination of the EBV 139, 146. However, clinically the requirement of a definitive diagnosis of OHL in the management of HIV-infected patients is rare.
Treatment:
Treatment of the OHL is seldom required because the lesion is usually asymptomatic, has not been shown to undergo any malignant transformation 147 and may resolve spontaneously 128. In HIV-infected patients on HAART, the lesion usually resolves spontaneously. Application of topical retinoids (e.g., 0.1% vitamin A) has been shown to improve the appearance of OHL-affected oral surfaces 148. Other treatments include topical podophyllin application 149, surgical excision 150 and cryotherapy 151, but none prevents the recurrence of the lesion after therapy. Antifungal therapy may reduce the extent of the lesion but does not eradicate the infection.
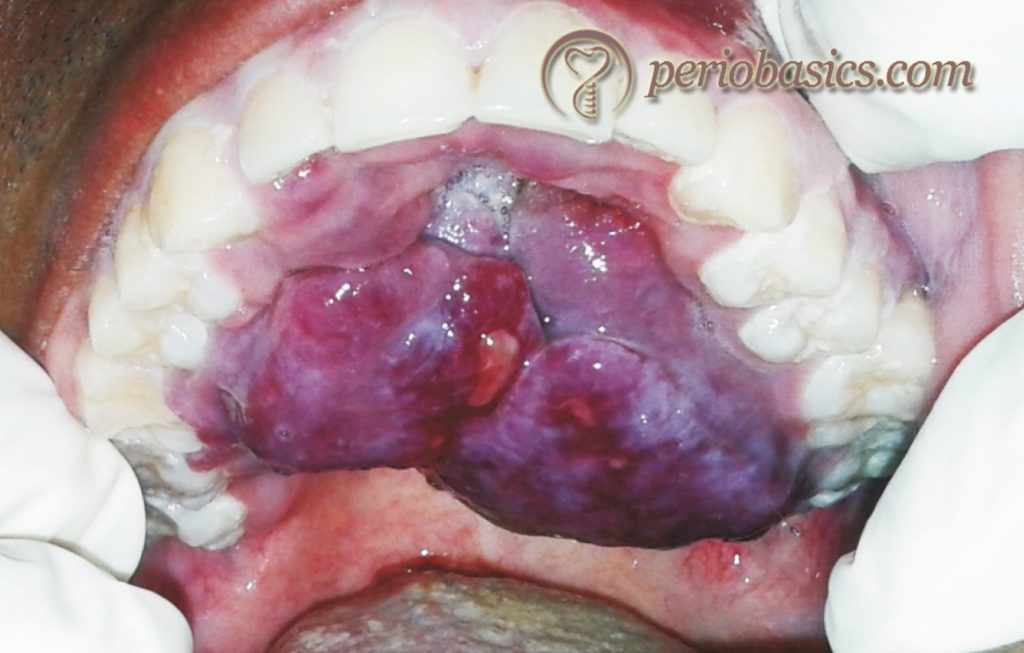
Kaposi’s Sarcoma (KS)
It is the most common malignancy associated with HIV infection. It is a malignant, multifocal systemic disease that originates from the vascular endothelium and has a variable clinical course. This malignancy was first described by Moritz Kaposi, a Hungarian dermatologist in 1872. Human herpesvirus 8 (HHV-8) is a crucial factor in disease pathogenesis, however, the exact mechanism of disease pathogenesis has not been elucidated 152. Skin is most commonly involved in KS. Other than skin, mucous membranes, lymphatic system, and viscera, in particular, the lung and gastrointestinal tract may also be ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Pathogenesis of KS:
A lot of research has been done to understand the pathogenesis of KS and its association with HIV infection. From the present evidence, it is clear that proliferating KS spindle tumor cells are of endothelial origin. The circulating blood mononuclear and endothelial ”progenitor cells” are believed to be the source of early KS lesions 154. Two well-accepted concepts of the pathogenesis of KS are altered cytokine expression and associated herpesvirus with KS.
Altered cytokine expression:
In HIV infection, there is a loss or impairment of CD4 cell function 155. As a result, there is an altered expression of cytokines including interleukin-1, tumor necrosis factor-α, and interleukin-6 156. In HIV-infected patient, these cytokines in blood have been shown to induce vascular endothelial cells to assume the characteristic spindle shape 157. Also, it has been demonstrated in various in vitro studies that these cytokines are associated with increased expression of a number of angiogenic growth factors (eg, basic fibroblast growth factor). Finally, the transactivating protein, HIV Tat, which is derived from HIV virus in HIV-infected patient, synergistically in combination with basic fibroblast growth factor, results in the………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Association of Herpesvirus 8 with KS:
Kaposi’s sarcoma-associated herpesvirus (KSHV; HHV-8) which belongs to γ subfamily of herpesviridae family has been found to be associated with various human cancers, including Kaposi sarcoma (KS) 159, 160, primary effusion lymphoma (PEL) 161, and the plasmablastic variant of multicentric Castleman disease (MCD) 162, 163.
There is strong evidence that KS is linked with the sexually transmitted virus, human herpesvirus 8 (KSHV). This association was first reported by Chang et al. (1994) 159 who found that more than 90% of HIV-KS tissue samples were positive for herpesvirus-like DNA sequences. The polymerase chain reaction analysis have demonstrated the presence of KSHV genomic DNA in the lesions, semen, and peripheral blood of patients with KS 164.
Clinical presentation:
The skin lesion of KS clinically appears as red, blue, or purplish lesions that are flat or nodular, and solitary or multiple. There are multiple clinicopathologic forms of skin associated KS which include patch, plaque, nodular, lymphadenopathic, infiltrative, florid, telangiectatic, ecchymotic, keloidal, angiomatous etc. The most common oral site of the lesion is hard palate, but it can also occur on the gingival surfaces and elsewhere in the mouth. The lesion may get easily ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….

Histopathology:
The definitive diagnosis requires histological examination. The histopathological picture is characterized by the proliferation of both spindle cells and blood vessels. The blood vessels are dilated and eosinophilic hyaline globules are present. Hemosiderin deposition is prominent. Extravasated red blood cells can be seen surrounding the blood vessels.
Treatment:
The first line of treatment of KS is antiretroviral therapy. It reduces the HIV viral load and raises the CD4+ T cell count, both of which indirectly contribute to the pathogenesis of KS. Along with the reduction in viral load, some of the protease inhibitors have been shown to have specific antineoplastic effects 165, 166. Other therapies for the treatment of KS include immunotherapy, radiation, intralesional chemotherapy, interferon therapy, cryotherapy and occasionally lasers.
Other diseases associated with HIV infection
Bacillary (Epitheloid) Angiomatosis
Bacillary epithelioid angiomatosis (BEA) is a rare cutaneous/mucosal disorder usually affecting patients infected with HIV. This lesion is often misdiagnosed as a vascular tumor. This angioproliferative disease was first described by Stoler et al. in 1983 167. The disease is caused by two species of Gram-negative bacilli: Bartonella (Rocha-limaea) henselae and Bartonella (Rochalimaea) Quintana 168. Skin and regional lymph nodes are most commonly involved in this disease. Other less commonly involved organs are liver, spleen, bone, oral mucosa, gastrointestinal tract, lung and brain 169-173. In the most common presentation of the disease, the skin lesions are multiple and reddish in color. Because of the dermatological manifestations, bacillary angiomatosis may be mistaken for Kaposi’s sarcoma. The differentiation of bacillary angiomatosis from Kaposi’s sarcoma is made by histological examination. Histopathological picture of BEA reveals an “epithelioid” proliferation of ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Non-Hodgkin’s lymphoma (NHL)
Non-Hodgkin’s lymphoma is the second most common malignancy associated with HIV infection. It has been observed that > 90% of HIV-associated NHL cases are derived from B-cells and the majority are high-grade. In most of the cases (70% to 80%) NHL has an extra-oral presentation. Oral NHL is seen only in 3% of cases 175. Clinically, the lesion may appear as soft-tissue masses with or without ulceration and tissue necrosis. Oral NHL commonly involves the gingival, palatal and alveolar mucosa.
Diagnosis of NHL is made with incisional tissue biopsy which demonstrates diffused and aggressive lymphoid infiltration with the replacement of the normal tissue by the proliferation of large cells with hyperchromatic central round nuclei, several nucleoli near the basal membrane and abundant eosinophilic cytoplasm. The radiographs demonstrate widening of the periodontal ligament space, loss of lamina dura and bone destruction.
Management of NHL in HIV-infected ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Squamous cell carcinoma (SCC)
The factors which have been linked with the development of SCC in patients with HIV infection include the use of tobacco/alcohol, HPV infection, immunodeficiency and possibly genetic factors 177. It has been demonstrated that HIV-positive patients are more likely to have a more advanced stage of oral SCC and poorer survival (57% survival at 1 year and 32% at 2 years) as compared to patients who are HIV negative (74% and 59%, respectively) 178. The proposed etiological factors associated with the development of SCC in HIV-infected patients are increased cellular growth and proliferation caused by viral interference with tumor suppressor proteins (p53, Rb), the activity of the HIV transactivator of transcription protein and role of human papillomavirus.

The oncogenic HPV-16 and HPV-18 have been frequently found associated with oral warts 179. One investigation demonstrated the presence of EBV in 17.59 % of all oral tumors and in 63.1 % of SCC of the tongue in 12 patients, suggesting its potential association with etiopathogenesis of oral SCC 180.
Oral hyperpigmentation
The color of the oral mucosa and skin is determined by the melanogenic activity of melanocytes, rather than the number of melanocytes in the epithelium. The melanin pigment is present in epithelial basal cells and particularly in subepithelial connective tissue. Melanin is synthesized in melanocytes with the help of enzyme tyrosinase which plays a critical role in the biosynthesis of both brown/black eumelanin and yellow/red pheomelanin. The production of melanin is controlled by various locally produced factors such as proopiomelanocortin and its derivative peptides, particularly α-melanocyte-stimulating hormone (α-MSH), melanocortin 1 receptor (MC1R), adrenergic and cholinergic agents, growth factors, cytokines, and nitric oxide 181. Melanocytes can produce both eumelanin and pheomelanin. The proportion of their synthesis depends on ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Hyperpigmentation of oral mucosa in HIV-infected patients can be seen as brown-black macules and diffuse areas of melanosis, seen primarily on the buccal mucosa, gingiva, hard palate, and lateral borders of the tongue. The systemic administration of zidovudine, ketoconazole, and clofazimine has been found to be associated with oral hyperpigmentation. However, in most of the patients, the cause is unknown 182.
Atypical ulcers
The deterioration of immunoregulation in HIV-infected patients is also associated with abnormally activated immune system. The abnormal activity of the immune system may induce injury to the self-antigens. Major aphthous ulcers are primarily caused because of this inappropriate activity of the immune system. They occur in approximately 2-3% of HIV-infected individuals. The clinical presentation of these ulcers is same as seen in uninfected individuals. The ulcers are large solitary or multiple, chronic, deep and painful. However, the ulcers in HIV-positive patients last longer and are less responsive to therapy.
Another reason for oral atypical ulcers is viral infections. As already discussed in the section of viral infections in HIV, various viral infections such as HSV, VZV, EBV, CMV etc. may present with atypical ulcers in the oral cavity. It has been shown that the persistence and severity of oral lesions is more in patients with low CD4 count and oral CMV-induced ulcers are indicative of systemic CMV infection 183.
The recurrent aphthous stomatitis is more common in HIV-infected patients as compared to uninfected persons. It presents with painful, recurring ulcers of the oral cavity. The systemic conditions associated with recurrent aphthous stomatitis are Crohn’s disease, ulcerative colitis, gluten-sensitive enteropathy, Behcet’s syndrome, Reiter’s syndrome, Sweet’s syndrome, cyclic neutropenia and nutritional deficiencies 184.
The treatment for oral atypical ulcers includes administration of systemic or intralesional corticosteroids, antimicrobial mouth rinses, oral tetracycline rinses and topical amlexanox. In severe ulcers, systemic corticosteroid therapy is given. Amlexanox (Lexanox), is a topical anti-inflammatory agent which has been found to be effective in the management of minor aphthous ulcers 185. In the case of suspected viral etiology of atypical ulcers, the identification of the causative virus is necessary. The virus can be identified by viral culturing and anti-viral drugs are used for appropriate treatment. Most commonly used ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
HIV-related salivary gland diseases
Salivary gland diseases in patients with HIV infection result in adverse effects on oral health. The conditions associated with salivary gland involvement primarily include xerostomia and salivary gland enlargement due to various pathologies like lymphoepithelial lesions, cysts involving the salivary gland tissue and/or intraglandular lymph nodes, Sjögren’s syndrome-like conditions, diffuse infiltrative lymphocytosis syndrome (DILS). In European and North American studies, the prevalence of salivary gland enlargement in HIV-infected patients has been reported to be around 1%-10% 186, with benign lymphoepithelial lesions (BLEC) present in 3%-6% of these cases 187, 188. Whereas, the average prevalence of HIV-associated salivary gland diseases in Africa was estimated to be 19% 189.
Salivary gland enlargement
The salivary gland involvement is most commonly associated with enlargement of the salivary gland with or without xerostomia 190. Inflammation and infection of salivary glands are the second most common reasons for salivary gland involvement followed by neoplasms 191. The exact etiopatho-genesis of salivary gland enlargement in HIV-positive patients is still not clear. However, the development of BLEC within the parotid gland seems to be the commonest etiology. BLEC are single or multiple cysts within lymph nodes situated mainly along the tail of the parotid gland that get entrapped in the tissue during parotid gland embryogenesis. The enlargement of the parotid gland may also result from the proliferation of glandular epithelium which gets trapped within the intra-parotid lymph nodes. It has been demonstrated that HIV has a predilection for lymphoid tissue and increased concentration of virus is present in these lymph nodes 187, 192, 193. Another reason for salivary gland enlargement in HIV-positive patients is “Diffuse infiltrative CD8 lymphocytosis syndrome”. This disease is characterized by ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Treatment:
There is no specific treatment for salivary gland enlargement in HIV-infected patients. Occasionally, the disease may resolve with HAART. The indicated surgical treatment is superficial parotidectomy. However, it is associated with significant morbidity, so its application is limited. Aspiration of cystic lesions has been suggested, however, it may also be of limited use because of multiple cysts 195. Radiotherapy, with 24 Gy in 1.5 Gy daily fractions has been reported to be useful for long-term cosmetic control of the enlargement 196.
Xerostomia
One of the major factors for dental decay in HIV-infected patients is xerostomia. In these patients, xerostomia is primarily drug-induced (mainly due to nucleoside transcriptase inhibitors, protease inhibitors), as well as anticholinergics, antihistamines, decongestants, antihypertensive agents, tricyclic antidepressants and narcotic analgesics. Other reasons for xerostomia include HIV-induced salivary gland diseases, Sjogren’s syndrome etc. Approximately 30% to 40% of ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Dental management of HIV-infected children and adolescents
With the spread of HIV/AIDS pandemic, more and more pediatric population is getting infected with HIV. With the help of an early diagnosis and prompt treatment with recent therapies, quality of life and life span of HIV infected children can be significantly increased. The oral opportunistic infections significantly deteriorate the systemic health of small children because of their inability to take adequate nutrition. Thus, a combined effort of physician and dentist is required to manage children with HIV infection.
The common oral manifestations of HIV infection in children are oral candidiasis, angular cheilitis, parotid gland swelling, xerostomia, dental caries, aphthous ulcers, herpetic stomatitis, hairy leukoplakia, linear gingival erythema, necrotizing ulcerative periodontitis (NUP) and other destructive diseases.
Management of these children and adolescents infected with HIV include complete documentation of oral and extraoral findings and subsequent three-month evaluation. The continuity of oral/dental care, especially when problems are detected on routine examination must be ensured. It has been observed that the HIV-infected children fail to comply with the dental appointment, even though they may be receiving an appropriate medical attention. Young children and older phobic children may require behavioral management techniques. Their treatment may require outpatient sedation or general anesthesia. A pediatric dentist is required to evaluate the ability of these children to cooperate in the outpatient setting. The caretakers of small kids should be educated to discontinue inappropriate use of bottle feeding to induce sleep. An immediate referral to a dentist is required if any signs or symptoms of caries are noted. Certain medications used in the treatment of HIV-associated diseases may contain cariogenic ………. Contents available in the book………. Contents available in the book………. Contents available in the book………. Contents available in the book……….
Conclusion
HIV can be considered as the worst pandemic which has ever affected mankind. However, the introduction of HAART has significantly improved the lifespan and quality of life of HIV-infected patients. The oral manifestations of HIV and AIDS are usually the first indicators of HIV infection. Early recognition, diagnosis, and treatment of HIV-associated oral lesions may reduce the morbidity of the patient. We are still looking for a definite cure for this disease but till we achieve that goal, the prime objectives of every dental health professional are prevention, diagnosis, treatment, and control of oral manifestations associated with HIV infection.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

