Introduction to bone destruction in periodontitis
Microbial etiology of periodontal diseases is well established, but the present data strongly suggest an equally important role of host immune response in the pathogenesis of periodontal diseases. The initial response to bacterial infection is a local inflammatory reaction that activates the innate immune system, causing the release of an array of cytokines and other mediators and propagation of inflammation through the gingival tissues 1, 2. Due to initiation of bacterial and host immune interaction, destruction of periodontal connective tissue results which continues until the source of infection, i.e. plaque, is removed. The exaggerated immune response in some patients, due to genetic factors can cause rapid breakdown of the tooth-supporting structures. In the following sections, we shall study various patterns of bone loss in periodontal diseases.
Periodontal bone architecture
In healthy periodontium, the alveolar bone roughly follows the cementoenamel junction (CEJ) on tooth surface 3. Normally, the interdental bone is 1.0 mm apical to the CEJ and this distance increases with age up to 2.8 mm 4. The interdental bone is placed coronally to the radicular bone. It forms a scalloped bony outline referred to as ‘positive’ architecture. In posterior areas, the interdental bone is less coronally projected as compared to anterior areas.

In periodontitis, bone loss may result in a situation where the interdental bone is placed apical to the radicular bone. This bony architecture is referred to as ‘negative’ or ‘reverse’ architecture. In the case where the interdental and radicular bone is at the same level, the bony architecture is referred to as ‘flat’ architecture. Ideally, the interproximal bone should be coronal to the facial and lingual bone with similar interdental bone level and a gradual slope.

Terminologies used to describe bony defects
Intrabony defect:
A periodontal defect surrounded by two or three bony walls or a combination of these.
Circumferential defect:
A vertical defect that includes more than one surface of a tooth, e.g., a vertical defect that includes the mesial and lingual surfaces of a tooth.


Interdental crater:
It describes the depression in the bone crest between adjacent teeth, composed of buccal and lingual walls and two other walls created by the roots of the adjacent teeth.
Horizontal bone defect:
In this type of defect, bone loss is perpendicular to the long axis of the tooth, along the whole length of the alveolar bone crest, with the occurrence of resorption of the buccal and lingual cortical plates, including the interdental bone.

Vertical bone defect:
It is located in the interdental bone and is defined by an oblique or angular orientation of the bone resorption in relation to the long axis of the tooth, in an apical direction.
Hemiseptal defect:
A vertical defect in the presence of adjacent roots; thus half of the septum remains on one tooth.
One wall, two wall, and three wall defects:
Intrabony defects are classified as one wall, two wall and three wall defects, depending on walls remaining around the defect (described later).
Trench-shaped defect:
A bony defect completely circumscribing the tooth like a trench.
Funnel-shaped defect:
An intrabony resorptive lesion involving one or more surfaces of supporting bone; may appear moat-like.
Role of bacteria and inflammation in periodontal bone destruction
Accumulation and maturation of plaque bacteria in the gingival sulcus initiate an inflammatory response characterized by infiltration of leukocytes, which limit the level of bacterial invasion. The factors that regulate leukocyte infiltration include bacterial products, cytokines, cross-talk between innate and adaptive immune responses, chemokines, lipid mediators, and the complement system. The following section describes the historical aspect of our understanding of the etiopathogenesis of inflammatory periodontal diseases.
Initial studies identified a relationship between plaque accumulation and gingival inflammation. Löe et al. (1961) 5 and Theilade et al. (1966) 6, demonstrated a direct relationship between bacterial plaque accumulation and gingival disease. During the same time period, animal experiments demonstrated a relationship among microbial plaque, inflammation, and periodontal bone loss 7-9. Other animal studies showed that treatment with antibiotics or topical application of chlorhexidine reduces the bacterial load and significantly reduces bone resorption 10, 11.
Then, with time different microorganisms which cause ……..Contents available in the book…….Contents available in the book…….Contents available in the book…….Contents available in the book…….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Page and Schroeder (1982) 16 have associated the rapid bone loss during active periods to subgingival ulceration which elicits an acute inflammatory response.
Seymour et al. (1978) 17 have associated rapid bone loss with the conversion of the predominantly T-lymphocyte lesion into a predominantly B-lymphocyte lesion.
Saglie et al. (1987) 18 have postulated that connective tissue invasion by various bacterial species elicits an advanced host response, leading to rapid bone resorption.
Newman et al. (1979) 19 have associated rapid bone loss with increased presence of loose, unattached and motile, Gram -ve bacterial species in pocket anaerobic flora.
The extent, to which bacterial plaque can cause bone resorption, was also investigated. Page and Schroeder (1981) 20, showed that bone resorption from the site of bacterial plaque accumulation is up to 2.5 mm and beyond that it is caused by bacterial invasion of gingival connective tissue. These bacteria activate an inflammatory response and hence, closer the cells of the inflammatory infiltrate to the bone, greater the number of osteoclasts formed resulting in the greater amount of bone degraded 21, 22.
In health, the amount of bone formation is equal to the amount of resorption that occurs and is referred to as coupling. This coupling is broken during inflammation, resulting in net bone loss 23, 24. With the improvement in our understanding regarding the host immune response, research work was focused on the role of host response in periodontal destruction. Later on, the role of cytokines and other chemical mediators was identified in bacteria-induced periodontal bone resorption. Presently, the role of cytokines like, IL-1β, TNF-α, and other chemical mediators is well established. A detailed description of molecular mechanisms involved in periodontal bone resorption in inflammation is given in “Osteoimmunology in periodontal health and disease”.
Spread of inflammation into the bone
The spread of inflammation from the gingival margin to underlying connective tissue and bone is responsible for bone resorption. The spread of inflammation occurs along the collagen fiber bundles and then following the course of blood vessels through loose connective tissue surrounding them into the alveolar bone 25. In inter-proximal areas, the inflammation may spread directly from the gingiva to the bone or from gingiva to the periodontal ligament and then into bone or from gingiva to the bone and then to the periodontal ligament. Facially and lingually, the inflammation spreads from gingiva along the outer periosteum into the bone and into periodontal ligament.
With the extension of inflammation into the underlying connective tissue, degradation of the gingival and trans-septal fibers take place. These are broken down and their fragments can be seen in between the inflammatory infiltrate 26. Along with their destruction, repair also takes place to re-establish them. This is why; even in advanced periodontal destruction, these fibers can be seen. As the inflammation spreads into the bone marrow, it gets infiltrated by inflammatory cells such as, leukocytes and mononuclear cells. The osteoclast differentiation is increased and the inner surface of the bone lining is made up of these cells. Subsequently, the fatty bone marrow is partially or completely replaced by fibrous bone marrow. The inflammatory process creates an environment for bone resorption, thus creating Howship lacunae. In persistent inflammation, loss of bone takes place, thus reducing bone height in that area.
Kronfeld (1935) 27 in a classic study, demonstrated that bone destruction taking place in periodontitis is not bone necrosis. The reason being, this whole process is being executed by living cells along the viable bone. These findings were further supported by Orban (1939) 28. So, bone loss in periodontitis is not by necrosis of bone, but by resorption of bone. The available bone is not infected or necrotic and should be preserved, if possible.
Know More…
Radius of action:
This term was first used by Garant and Cho (1979) 29. They pointed out that bone resorption stimulators produced by microbial plaque have a finite radius of action. Waerhaug 30-33 investigated this principle on human periodontitis cases by doing histological sections, measurements on radiographs and extracted teeth to find out the distance between microbial plaque and bone surface . His research has demonstrated that bone margin is never located closer than 0.5 mm to plaque and not farther than 1.5-2.5 mm from plaque.
These findings indicate that when microbial plaque comes as close as 0.5 mm to the bone surface, bone resorption takes place. On the other hand, the bone resorption stimulated directly or indirectly by microbial plaque is only effective for a distance up to 1.5-2.5 mm.
Local factors determining patterns of bone resorption
Bone thickness:
Teeth are surrounded by a variable thickness of alveolar bone on different surfaces. In addition, the blood supply is variable in different parts of the alveolar bone. For this reason, pattern of bone resorption is random. Resorption follows the pathway of inflammation, but that pathway may be different around different teeth. The pattern of bone resorption to a large extent depends on the mass of alveolar bone present in the region. Dehiscence is usually seen in areas with a thin labial plate, where inflammation extends from marginal gingiva in apical direction.
In the same way, if the investing bone is thick and marginal inflammation extends apically, the resultant pattern of bone resorption would be like a trench or well. So, funnel-shaped defect results only when there is a sufficiently thick mass of bone present and inflammatory process slowly cause bone resorption along the tooth; otherwise, dehiscence will result.
Anatomical factors:
Another major factor determining the bone resorption is anatomical location and tooth anatomy. Take an example of ……..Contents available in the book…….Contents available in the book…….Contents available in the book…….Contents available in the book…..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Presence of lingual tori and buccal exostosis:
Both lingual tori and buccal exostosis produce a similar situation as explained above in the case of maxillary and mandibular molars. A thick bony mass present around teeth makes a conducive environment for pocket formation and later a funnel-shaped defect.
Know More…
Crater formation:
A major requirement for crater formation is the presence of a thick mass of bone with guarding and thick buccal and lingual plates. This requirement is fulfilled by posterior teeth, where the interproximal bone is sufficient to result in such kind of defect. Once the crest of the cortical plate is destroyed, the formation of the bony crater is quite rapid in these areas during chronic inflammation.
Presence of thick or thin periodontium:
The thickness of periodontium plays an important role in the formation of osseous defects. A thin periodontium is commonly found around the anterior teeth. Roots of teeth are embedded in relatively thin bone with a thin overlying soft tissue. This situation is not favorable for the formation of craters, rather dehiscence or pyramidal bone loss are commonly found in this situation. After treatment, these areas usually show gingival shrinkage and recession.
On the other hand, thick periodontium presents an entirely different clinical situation. Here, the investing structures of the tooth are thick with thick alveolar housing around the teeth. Inflammation of the periodontium in these areas causes a circumferential bone loss around the teeth, which may vary according to the direction of spread of inflammation and other anatomical factors like root anatomy and tooth positioning.
Presence of trauma from occlusion (TFO):
TFO has been defined as structural and functional changes in the periodontal tissues caused by excessive occlusal forces. Occlusal trauma is the overall process by which traumatic occlusion (occlusion that produces forces that cause injury) produces injury to the attachment apparatus. It may cause a thickening of the cervical margin of the alveolar bone or a change in the morphology of the bone.
Irrespective of the presence or absence of inflammation, TFO causes bone destruction. In the absence of inflammation, TFO causes compression and tension on the periodontal ligament. Excessive forces on periodontal ligament cause necrosis in the affected areas and osteoclastic activity is also initiated causing bone resorption. Resorption of tooth structure can also result due to the extension of osteoclastic activity. These changes are reversible and if offending forces are removed, repair of the injured tissues takes place. But, if the abnormal forces are not removed and the tooth is under trauma for a long duration of time; a funnel-shaped widening of the periodontal ligament can be seen in the crestal areas, which later on causes bone resorption, resulting in an angular bone defect. If TFO is associated with inflammation, the destructive effects of inflammation are enhanced. TFO modifies the spread of inflammation into the connective tissue, resulting in aggravated tissue destruction. A complete description of TFO has been given in “Trauma from occlusion”.
Know More…
Bone factor concept:
The bone factor concept was given by Irving Glickman (1949) 36. According to this concept, there is a dynamic relationship between the local and systemic factors in the maintenance of normal physiology of the bone. Now, if an individual has a generalized tendency for bone resorption, aggravated bone destruction can be seen in local inflammation. This concept helps us in the determination of prognosis of an individual with periodontitis. For example, in post-menopausal women, the protective action of estrogen on the bone is down-regulated because of its decreased levels. So, the bone factor and local inflammation, in this case, may cause more bone destruction as compared to pre-menopausal women.
Role of systemic factors in bone destruction
Systemic factors, along with local factors play an important role in the maintenance of normal bone physiology. Systemic factors may accelerate the rate of bone resorption by adding up into the local inflammatory component. Osteoporosis is a common condition in post-menopausal women, which shares many common risk factors with periodontitis. Various studies have shown a relationship between skeletal bone density and oral bone density 34, 35. Various other systemic diseases such as hyperparathyroidism, leukemia, Langerhan’s cell histiocytosis etc. also cause bone loss but in a totally different way as compared to periodontitis. Hence, while examining a patient, a detailed medical history should be recorded to identify any such systemic factor.
Classification of bone defects
Goldman and Cohen (1958) 37, classified bony defects as suprabony, when the base of the pocket was present coronal to the alveolar crest and infrabony, when the base of the pocket was present below the alveolar crest. Infrabony defects are of two types, intrabony defects, and craters. Intrabony defects are bony defects, wherein ……..Contents available in the book…….Contents available in the book…….Contents available in the book…….Contents available in the book…
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
It is a broad classification of intrabony defects. Many times, more complex bone defects are encountered, where a three-wall defect in the apical portion becomes two or one wall defect in the coronal region. This is then referred to as a combined osseous defect.








Clinical aspect of osseous defects and deformities
In periodontal disease progression, there are active periods of periodontal destruction which may be episodic or intermittent in fashion with periods of inactivity or quiescence. During active periods, signs of inflammation are evident with microscopic evidence of acute inflammatory reaction and ulcerations. There is a loss of collagen and alveolar bone, depending on the disease activity. During inactive periods, signs of inflammation are minimal and the reparative process is initiated. Bone formation can be seen immediately adjacent to the site of bone resorption and along the trabecular surfaces at a distance from the inflammation. This bone formation is an effort to strengthen the remaining bone, also known as “buttressing bone formation”. This repair causes the formation of different bony deformities which can be seen clinically during surgical procedures.
Know More…
Defect morphology and regeneration potential:
The morphology, or shape, of a periodontal defect, directly impacts the prognosis for regenerative therapy. As already stated, ‘wall’ defects signify the number of remaining bony walls that surround the area of the root affected by bone loss. For example, a three-wall intrabony defect on the distal aspect of a tooth would have a buccal, lingual and distal ‘wall’ surrounding the area of severe bone loss. The bone ‘walls’ of a defect provide physical support and containment for the regenerative materials and are a source of osteoprogenitor cells in addition to cells derived from the PDL. Thus, an intrabony defect with more number of remaining bony walls has more potential for bone fill and regeneration. Three wall defects have the best results with regenerative therapy, whereas, one wall defects have poor results with regenerative therapy.
Along with the number of remaining walls, the size or depth and width of the periodontal defect also plays a significant role while attempting regenerative therapy. Because the bone walls and PDL are the primary sources of bone-forming cells, a wide defect presents a greater challenge to bone regeneration as the cells have to migrate further, to make new bone. On the contrary, a narrow defect facilitates cellular migration. Hence, narrow and deep intrabony defects have been shown to respond more favorably to regenerative therapy than wide, shallow defects.
Various bone destruction patterns in periodontal diseases
Periodontal diseases alters the morphological features of the bone in addition to reducing bone height. An understanding of the nature and pathogenesis of these alterations is essential for effective diagnosis and treatment. Following patterns of bone loss are seen in periodontitis,
• Horizontal bone loss
• Furcation involvement
• Osseous craters
• Bulbous bone contours
• Reversed architecture
• Ledges
Horizontal bone loss:
Normally, the crestal bone is situated 1 to 2 mm apical to the CEJ. In periodontitis, due to bone loss, the crestal bone is more than 2 mm apical to the CEJ. Bone loss is considered horizontal when the crest of the proximal bone remains parallel to an imaginary line drawn between the CEJ of adjacent teeth. The horizontal bone loss may be localized or generalized. It is usually associated with suprabony pockets.
Vertical/angular bone loss:
Bone loss is considered vertical (angular) when the crest of the proximal bone is not parallel to the imaginary line drawn between the CEJ of adjacent teeth. The vertical bone loss is usually localized and related to factors such as TFO, calculus, subgingival plaque, overhanging restorations, and food impaction. It is associated with the intrabony pocket formation. As already stated, vertical defects are broadly classified as one wall, two wall, and three wall defects. A vertical defect that involves more than one surface of the tooth is referred to as circumfrential defect.

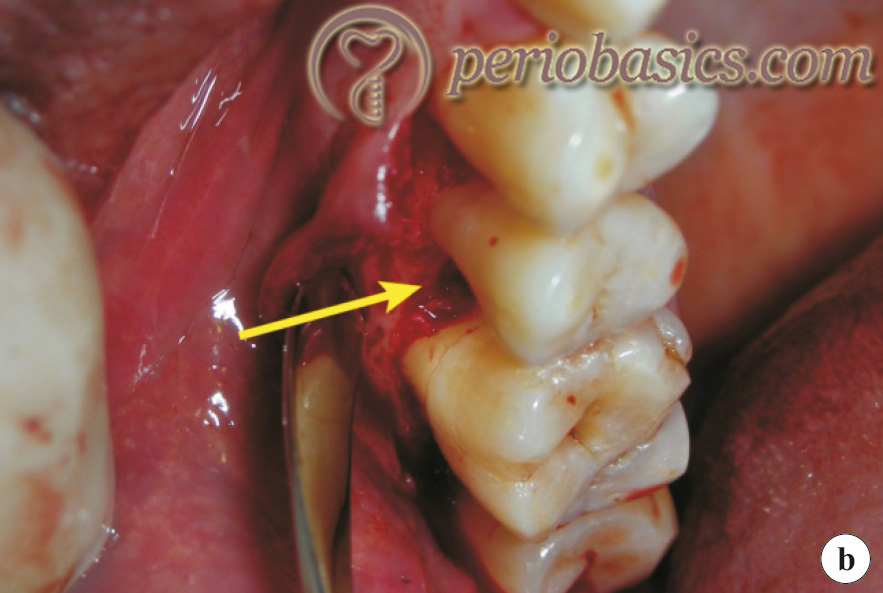
Vertical bone defects can be visualized on radiographs but in cases where thick buccal or lingual plates are present, it may be obscured. So, the most authentic way to correctly determine the bone defect is surgical exposure of the area. It has been shown that the frequency of occurrence of vertical bone defects increases with age 38, 39 and these are found more commonly on the distal 40 and mesial surfaces of the teeth 38, 39 as reported by different researchers.
Furcation involvement:
Furcation involvement refers to the commonly occurring conditions in which the bifurcations and trifurcations of multirooted teeth are invaded by the disease process. Furcation involvement is a stage of progressive periodontitis in which the apical extension of inflammation causes progressive attachment loss. The involved furcation may be visible clinically or it may be covered by the soft tissue. Other factors that may play a role in furcation involvement are:
• Trauma from occlusion.
• Presence of enamel projections.
• Proximity of the furcation to the CEJ.
• Presence of accessory pulpal canals in the furcation area.

A detailed description of furcation involvement is available in “Furcation involvement and its management”.
Osseous craters:
These are concavities in the crest of the interdental bone confined within the facial and lingual walls. These are one of the most commonly found bone defects which make around one-third (35.2%) of all the defects and about two-thirds (62%) of all the mandibular defects. Their frequency of occurrence is twice in the posterior segment as compared to the anterior segment 41, 42.
Bulbous bone contours (exostosis):
These are bony enlargements caused by exostoses, adaptation to function or buttressing bone formation. These are found more frequently in the maxilla than in mandible.
Reversed architecture:
As stated earlier, it is produced by the loss of interdental bone, including the facial and lingual plates without loss of radicular bone.
Ledges:
A ledge refers to a plateau-like bone margin caused by the resorption of thickened bony plates.

Bone formation in periodontal diseases
It must be remembered that in periodontitis, along with periodontal bone resorption, the reparative process is also present to reinforce the remaining bone. The areas of bone formation can be seen immediately adjacent to the sites of bone resorption along the trabecular surfaces. This type of bone formation is also referred to as, ‘Buttressing bone formation’. Various animal 44 and human 45, 46 histological studies have demonstrated the osteogenic response adjacent to the areas of bone resorption. Hence, bone loss in periodontitis is not just a resorptive process, but a relative predominance of the resorptive process over the bone formation. Furthermore, bone formation also occurs on ……..Contents available in the book…….Contents available in the book…….Contents available in the book…….Contents available in the book…….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Conclusion
The pathophysiology involved in different patterns of bone destruction in periodontal diseases is a combination of destructive and reparative processes. The host response tries to repair the injury for re-establishment of normal structure and function of the tissue. But, if the infection is persistent, then these processes do not come to rest and various patterns of tissue response to the injury can be observed. The reestablishment of the normal physiological bone contour is desired in surgical periodontal therapy. A detailed description of the procedures involved in bone recontouring and reshaping has been given in “Osseous resective surgeries”.
References
References are available in the hard-copy of the website.

