Introduction to the major histocompatibility complex
Cellular interactions are very important for the recognition and presentation of antigens to the immune system by antigen-presenting cells 13, 14. The primary components of these interactions are the T-cell antigen receptor (TCR) and the Major histocompatibility complex (MHC)/human leukocyte antigen (HLA) molecules. The major function of the TCR is to recognize the antigen in the correct context of MHC and to transmit an excitatory signal to the interior of the cell.
Major histocompatibility complex (MHC) classes
The MHC is highly polymorphic from individual to individual and segregates in families in a Mendelian co-dominant fashion.
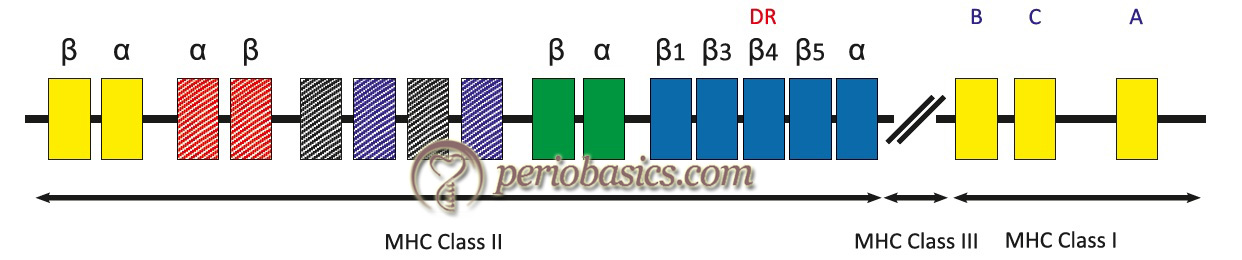
- Genes for HLA are clustered in MHC located on the short arm of chromosome 6: 6p21.
- MHC Class I gene complex contains three loci: A, B and C, each of which codes for α chain polypeptides .
- Class II gene complex contains at least three loci: DP, DQ, and DR; each of these loci codes for one α and a variable number of β chain polypeptides.
- Class III region is not actually a part of the HLA complex, but is located within the HLA region, because its components are either related to the functions of HLA antigens or are under similar control mechanisms as the HLA genes. Class III antigens are associated with proteins in serum and other body fluids (e.g. C4, C2, factor B, TNF) and have no role in graft rejection.
For MHC proteins, each individual has haplotypes i.e., one set of genes is inherited from each parent. These chains are very diverse (polymorphic) and there are many alleles of Class I and Class II MHC molecules. We have more than 47 alleles for HLA -A, 88 for HLA -B, 29 for HLA -C and 300 for HLA-D genes. An individual inherits only single allele from each locus and can make only one MHC-I and MHC-II protein. The expressions of these genes are co-dominant and are expressed. Each person can have 12 HLA proteins: 3 for Class I and 3 for Class II from each parent. In addition to HLA genes which are encoding major antigen, there are several minor antigens encoded by several genes other than HLA. These genes lead to …… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Class I MHC:
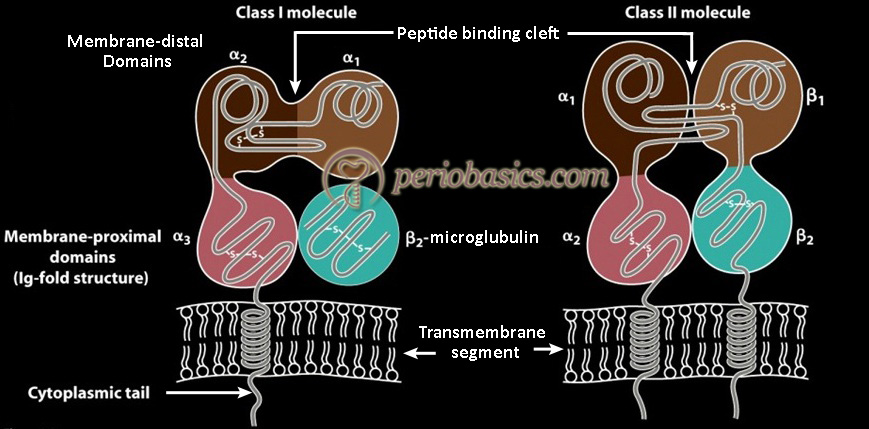
The Class I MHC molecules are glycoproteins, which are found on the surface of virtually all nucleated cells. These are composed of two separate polypeptide chains, heavier (44-47 KDa) α chain and lighter (12 KDa) β chain. The α chain is identical to immunoglobulin and has three globular domains α1, α2, and α3. It has a hypervariable region at its N-terminal region. These regions are responsible for the recognition of self and non-self antigens. The carboxyl end of α chain resides inside the cell, while the amino end projects on the surface of the cell with a short intervening hydrophobic segment, which traverses the membrane.
Structure of Class I MHC molecules
As already stated, structurally MCH I molecule consists of two polypeptide chains, a long α chain and a short β chain (β2-microglobulin). The α chain has the following four regions:
- A cytoplasmic region, containing sites for phosphorylation and binding to cytoskeletal elements.
- A transmembrane region, containing hydrophobic amino acids by which the molecule is anchored in the cell membrane.
- A highly conserved α3 immunoglobulin-like domain to which CD8 binds.
- A highly polymorphic peptide binding region formed from the α1 and α2 domains.
The β2- microglobulin in an association with α chain helps in maintaining the proper conformation of the molecule.
Class II MHC:
These are glycoproteins found primarily on the surface of the antigen-presenting cells, such as macrophages, B-cells, dendritic cells, cells of the spleen and Langerhans cells of the skin. MHC Class II molecules comprise of two non-identical and non-covalently associated polypeptide chains (α and β). These two chains have amino ends on the surface, a short transmembrane stretch, and intracytoplasmic carboxyl ends. Like MHC I, they have hypervariable regions. As already discussed, the MHC I molecule is made up of two chains where chain I (α) is encoded by MHC and chain II (β2-microglobulin) is encoded by chromosome 15. In MHC II molecules both chains are encoded by MHC II. Two polypeptide chains have a constant region where the CD4 cell is attached.
Structure of Class II molecule:
As stated above, Class II MHC molecules are composed of two polypeptide chains, an α and a β chain of approximately equal length. Both chains have four regions:
- A cytoplasmic region, containing sites for phosphorylation and binding to cytoskeletal elements.
- A transmembrane region, containing hydrophobic amino acids by which the molecule is anchored in the cell membrane.
- A highly conserved α2 domain and a highly conserved β2 domain to which CD4 binds.
- A highly polymorphic peptide binding region formed from the α1 and β1 domains.
Biological importance and function of MHC:
- The type of immune response to be generated against an antigen depends on the interactions between antigen-presenting cell and Class of MHC molecule.
- MHC Class I molecules bind to cytotoxic T- cells.
- MHC Class II molecules bind to helper T-cells.
These cells bear the responsibility to find out self and non-self cells. This is called as MHC-restriction. B-cells do not have this requirement as they can recognize the soluble antigens present in plasma with their surface-associated IgG and/or IgM, acting as receptors.
Antigen processing by antigen-presenting cells
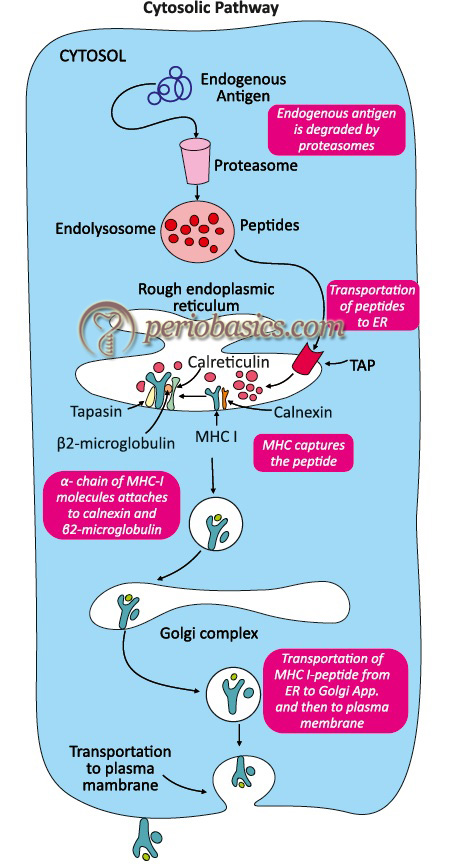
There are two different pathways by which the APCs eliminate intracellular and extracellular antigens. These are cytosolic and endocytic pathways. The antigens which are generated within the cell (endogenous antigens) are processed by the cytosolic pathway and the antigens that are taken up by endocytosis (exogenous antigens) are processed by the endocytic pathway. In the cytosolic pathway, the processed antigen is presented on the membrane with Class I MHC molecule whereas in the endocytic pathway the processed antigen is presented on the membrane with Class II MHC molecule. Let us discuss these pathways in detail.
Cytosolic pathway
In all eukaryotic cells, the intracellular protein turnover is highly regulated. There are various intracellular pathways that regulate the normal turnover of intracellular proteins. The proteins that are subjected to proteolytic degradation are often attached to a small protein, called ubiquitin. These ubiquitin-protein complexes can be then degraded by a multifunctional protease complex called a ‘proteasome’. Proteasomes are cylindrical in shape consisting of four rings with a central channel of the diameter of 10 to 50 Å. The proteasome-dependent protein degradation is an …… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
As already discussed in the previous sections, the MHC Class I molecule consists of long α and short β (β2-microglobulin) chains. Both of these chains are synthesized on polysomes along the rough endoplasmic reticulum. It should be remembered here that a stable MHC Class I molecule is formed only after the attachment of a peptide in the binding groove of the molecule. The stable MHC Class I molecule can exit the rough endoplasmic reticulum for presentation of the antigenic peptide on the cell surface. The formation of a stable MHC molecule requires several steps involving the participation of molecular chaperones. The first molecular chaperone involved in this process is calnexin. This molecule attaches to α chain of MHC molecule and promotes its folding. This assembly is present on the inner surface of the membrane of the endoplasmic reticulum. Calnexin dissociates with α chain once β2-microglobulin binds to the α-chain. Next molecular chaperones those get associated with Class I MHC molecule are calreticulin and tapasin. The primary function of tapasin is to bring TAP molecule in close proximity to MHC molecule. The formation of MHC Class I molecule and TAP molecule heterodimer promotes the peptide capture by Class I molecule before they are exposed to the endoplasmic reticulum lumen. Peptides that do not attach to the MHC Class I molecule are degraded rapidly. After the attachment of the peptide to the peptide-binding cleft, the MHC complex becomes stable and dissociate from calreticulin and tapasin. The MHC-I and peptide complex then exits from the endoplasmic reticulum and proceed to the cell surface via the Golgi apparatus.
Endocytic pathway
The endocytic pathway involves internalization of antigen by phagocytosis or endocytosis or both. Different cells have different mechanisms of antigen internalization. Macrophages internalize the antigen by phagocytosis whereas other APCs internalize antigen primarily by endocytosis. The internalized antigen is broken down into oligopeptides (13-18 residues) in the endosome by enzymatic action. Three types of endosomal compartments have been described according to the acidic environment within them: early endosomes (pH 6.0-6.5); late endosomes, or endolysosomes (pH 5.0-6.0); and lysosomes (pH 4.5-5.0). The oligopeptides are generated from the break-down of antigen bind to Class II MHC molecules. It should be noted here that MHC Class II molecules are also synthesized in the rough endoplasmic reticulum and are present on the inner surface of its membrane. But they do not attach to the endogenous antigen because their binding site is blocked by an invariant chain. The MHC Class II molecule attaches to the exogenous antigen in the endocytotic compartment after degradation of invariant chain. Finally, endocytic compartments, or portions of them that containing the MHC Class II and oligopeptides move towards the cell membrane and fuse with the membrane, thereby presenting the MHC Class II- antigen oligopeptides complex on the cell surface.
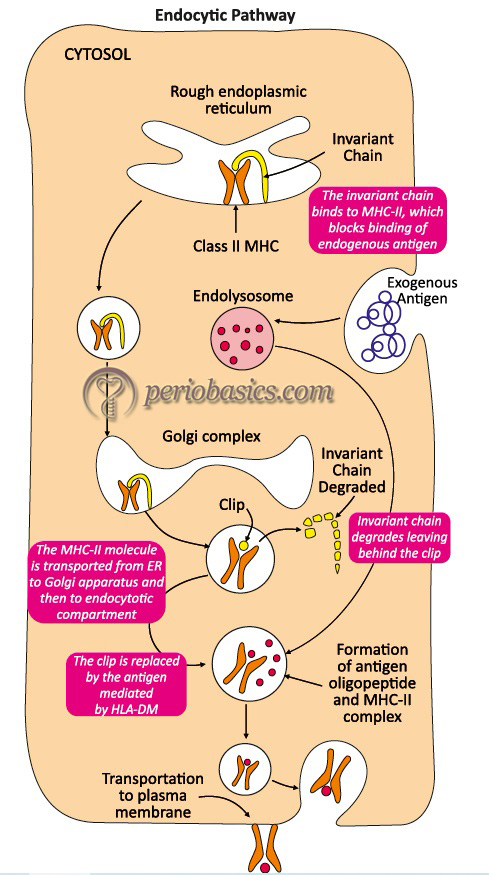
From the above discussion, it can be concluded that, mode of entry of antigen into the cell (exogenous or endogenous), and the site of its processing decides whether the antigenic peptide will associate with MHC Class I or with MHC Class II molecule.
Transplantation and graft rejection
An autograft that is transplanted on own tissue is always accepted. A synergistic graft, that is, the transfer of tissue between genetically identical individuals or identical twins, is almost always accepted. A Xenograft is the transfer of tissue between two species and is always rejected by immunocompetent cells. An allograft is tissue transfer between genetically different members of the same species i.e. from one human to another. An allograft is usually rejected unless the patient is given immuno-suppressive drugs. The severity and rapidity of rejection depend upon the difference between donor and recipient MHC loci. Following are some important points which should be remembered regarding grafts,
- Allograft rejection: Unless immunosuppressant drugs are given, the allograft is rejected by a mechanism of allograft reaction.
- Acute graft rejection: Initially graft is normal but after 11-14 days, a marked reduction in circulation and mononuclear infiltration occurs which eventually lead to necrosis this is also called as the primary reaction or first set reaction
- Hyper-acute (white graft) rejection: In this case graft is rejected very …… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
The allograft is rejected in two steps
(i) APC’s (macrophages and dendritic cells in the graft present self-proteins of the host and activate the immune response)
(ii) Donor proteins (MCH I and II) may be shed and subsequently processed by recipients antigen-presenting cells and initiate an immune response
Prior to tissue transplantation a test, “TISSUE TYPING” test is done to find the closest match between recipient and donor. Class I proteins and certain class II proteins especially DR are detected by using a panel of known antibodies. Nucleotide sequencing is done. Further matching can be done by mixed leucocyte reaction.
Graft versus host (GVH) reaction
Transplantation may be normal but in some patients, GVH develops. It occurs in those patients who are irradiated and immunocompromised. This rejection is due to the proliferation of immunocompetent cells present in the graft of the donor. These cells develop against recipient proteins and subsequently, a severe dysfunction develops. Donor cytotoxic T-cells destroy recipient cells.
Requirements for (GVH) to occur
- Graft must contain immuno-competent cells.
- Host must be immuno-compromised.
- Host must express antigen foreign to donor’s i.e. donor cells recognize recipient cell as foreign.
If donors and recipients MHC complexes are matched even then the (GVH) can occur due to minor antigens. GVH can be reduced by treating the donor graft with anti-thymocyte globulins or monoclonal antibodies before grafting. It eliminates mature T-cells from the graft.
Effect of immunosuppression on graft rejection
To reduce the chances of rejection of transplanted tissue immunosuppressive agents such as cyclosporine, tacrolimus, rapamycin, corticosteroids, azathioprine, OKT3 antibody and radiations are used.
- Cyclosporin and Tacrolimus: both have the same mode of action. It interrupts signal transduction by inhibiting calcineurin. Tacrolimus is more immunosuppressive and has more side effects. Cyclosporin is widely used.
- Rapamycin: Inhibits transduction but at some other site than cyclosporine.
- Corticosteroids: These act primarily by inhibiting Cytokine e.g. IL-1 &TNF.
- Azathioprine: Inhibit DNA synthesis and block growth of T cells.
- OKT3: is a monoclonal antibody against CD3 protein that can block T-cell function as well as lysis of T-cells is carried out by these antibodies.
Immunosuppression increases the risk of development of neoplasm by 100 times and also the development of opportunistic disease and infections take place.
Summary of MHC complex
- As Each MHC molecule has only one binding site, only one peptide can bind to it at a time.
- A peptide must associate with a given MHC of that individual; otherwise no immune response can occur.
- Mature T-cells must have a T-cell receptor that recognizes the peptide associated with MHC.
- MHC molecules are membrane-bound so recognition of these molecules by T-cells requires cell-cell contact.
- MHC gene alleles are co-dominant so their product is expressed on the cell surface of an individual nucleated cell.
- Cytokines (especially interferon-γ) increase the level of expression of MHC.
- Class I MHC is recognized by cytotoxic T-cells (CD-8 cells). Class II MHC is recognized by helper T-cells (CD-4 cells).
- Polymorphism in MHC is important for the survival of the species.

