Introduction to gingival enlargement
Gingival enlargement or gingival overgrowth is the increase in the size of gingiva. It is a common clinical condition usually seen in acute and chronic gingival inflammation. The enlargement of the gingival tissue may also occur due to many other reasons, which include drug intake associated, conditioned, neoplastic or false enlargements. Many genetic conditions have gingival enlargement as one of their clinical features. In the following discussion, we shall study in detail about the different types of gingival enlargement.
Classification of gingival enlargement
According to the etiology and pathologic changes:
I. Inflammatory gingival enlargement:
Acute
Chronic
II. Fibrotic gingival enlargement:
Drug-induced
Idiopathic
III. Combined gingival enlargement (fibrotic + inflammatory)
IV. Gingival enlargement associated with systemic conditions/ diseases
a) Conditioned gingival enlargement:
Pregnancy
Puberty
Vitamin C deficiency
Plasma cell gingivitis
Nonspecific conditioned enlargement
b) Gingival enlargement associated with systemic diseases:
Leukemia
Granulomatous diseases (Wegener’s granulomatosis, Sarcoidosis)
V. Gingival enlargement associated with genetic disorders
VI. Neoplastic gingival enlargement (gingival tumor):
Benign tumors
Malignant tumors
VII. False enlargement.
According to the location and distribution:
Localized: Involving a single tooth or a group of teeth.
Generalized: Involving the gingiva throughout the mouth.
Papillary: Confined to the interdental papilla.
Marginal: Confined to the marginal gingival.
Diffuse: Involving the marginal and attached gingivae and papillae.
Discrete: Isolated sessile or pedunculated (tumor-like) enlargement.
Let us now discuss various gingival enlargements in detail,
Inflammatory gingival enlargement
Inflammation in gingival tissue can cause enlargement of the gingiva that is called as an inflammatory gingival enlargement. More accurately, it is edematous gingival enlargement, as it is caused by the accumulation of fluids in the inflamed gingival connective tissue. The fluid is primarily serum that has emerged from blood vessels due to increased permeability because of local inflammation. Gingivitis and periodontitis are two common inflammatory periodontal conditions found in the majority of the population. The commonest sign of either gingivitis or periodontitis is bleeding gums, which can be provoked by tooth brushing, flossing, and eating hard foods, but can also be spontaneous. Inflammatory gingival enlargement can be acute or chronic.

Acute gingival enlargement
The acute gingival enlargement is usually associated with specific infections or trauma. The forceful embedding of foreign substances such as toothbrush bristles, a piece of apple core or a fragment of lobster shell results in the placement of bacteria deep into the tissue. The inflamed gingiva appears reddish with smooth and shiny surface. Within 24-48 hours, the inflammatory lesion usually becomes fluctuant and with due course of time, the purulent exudate is expressed from a pointed orifice in the swelling.
Chronic inflammatory enlargement
Chronic inflammatory gingival enlargement can be localized or generalized. Localized gingival enlargement originates as a slight ballooning of the interdental papilla or gingival margin. In early stages, it appears as a life-saver like bulge around the involved tooth/group of teeth. Later on, the interdental papilla and gingival margin increase in size until it covers a part of the crown. This process progresses slowly and painlessly unless it is complicated by infection or trauma. Later on, it may progress to achieve generalized form.
Gingival changes associated with mouth breathing
Mouth breathers usually present with gingival enlargement. The gingiva appears red and edematous with a diffuse shiny surface. The maxillary anterior region is the common site and the altered gingiva is clearly demarcated from the adjacent normal gingival. The exact manner in which breathing affects gingiva in not known, but its harmful effect is generally attributed to irritation due to surface dehydration.

Fibrotic gingival enlargement
Drug-induced gingival enlargement
“Gingival enlargement” or “gingival overgrowth” is the preferred term for all medication-related gingival lesions, previously termed as “gingival hyperplasia” or “gingival hypertrophy” 1. This condition is characterized by the accumulation of extracellular matrix within the gingival connective tissue, particularly the collagenous component, with various degrees of chronic inflammatory infiltrate 2. Drug-induced gingival enlargement was first reported in 1939 by Kimball 3, who observed …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Following is the discussion of some major drugs responsible for fibrotic gingival enlargement:
Antiepileptic drugs
Phenytoin is the drug of choice for the treatment of grand mal, temporal lobe, and psychomotor seizures. Gingival overgrowth is a common adverse effect of therapy with phenytoin, having important medical and cosmetic implications. Poor periodontal hygiene is an important risk factor for the severity of phenytoin-induced gingival overgrowth, which is a time-dependent process. Prevalence of gingival enlargement with phenytoin (Dilantin®) use has been shown to be up to 50%, while with other anticonvulsants such as valproic acid, Phenobarbital® and Tegretol®, it has been shown to be less frequent. The pathogenesis and exact mechanisms responsible for gingival overgrowth are still not fully understood.



Phenytoin is primarily metabolized to the inactive hydroxy phenytoin, 5-(4′-hydroxyphenyl)-5-phenylhydan-toin or p-HPPH by cytochrome P450 (P450) enzymes, which may be further metabolized to a catechol that spontaneously oxidizes to semiquinone and quinone species that covalently modify proteins. Another anti-epileptic drug is valproic acid, which has been reported to cause gingival enlargement. It is highly protein bound (87-95%), resulting in its low clearance (6-20 mL/hr/kg). This drug is metabolized in at least three ways in humans: glucuronidation, β-oxidation in the mitochondria (both considered major routes accounting for the metabolism of 50% and 40% of the dose, respectively), and cytochrome P450 (CYP) mediated oxidation (considered a minor route, approximately 10%) 23, 24. A relatively new anti-epileptic agent is vigabatrin that can cause gingival over-growth 25.

Calcium channel blockers
Calcium has a central role in cellular physiology. The calcium channel blocker group of drugs is used extensively as antihypertensive drugs. As discussed earlier, nifedipine was first reported in 1984 to be causatively associated with the gingival enlargement. Dihydropyridines can directly affect the gingival connective tissue cells (fibroblast-like cells), causing overgrowth of the connective tissue. Gingival enlargement with calcium channel blockers has been reported with verapamil, nifedipine, diltiazem and amlodipine 20, 26, 27.


Cyclosporine A
Cyclosporin A (CsA) is widely used for the prevention of transplant rejection as well as for the management of a number of autoimmune conditions such as rheumatoid arthritis 28, 29. CYP3A4 and to a larger extent CYP3A5 are the major iso-enzymes responsible for the hepatic metabolism of CsA. The use of CsA is associated with various side effects including neurotoxicity, hepatotoxicity, hypertension etc. Gingival enlargement is one of the side effects of long term use of CsA. Research has demonstrated that CsA increases both IL-6 and TGF-β1 levels. IL-6 or TGF-β1 treatment has …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….

Mechanisms involved in drug-induced gingival overgrowth
Direct effect on fibroblasts
Fibroblasts are responsible for collagen production as well as degradation. Studies have been done to find out the direct effect of phenytoin, nifedipine, and cyclosporin A on fibroblasts. These studies have investigated collagenous and non-collagenous extracellular matrix metabolism by gingival fibroblasts 32-36. Cyclosporin A was found to increase glycosaminoglycan secretion by fibroblasts 34 and nifedipine and phenytoin increased heparin levels 37. But many in vitro studies failed to report any differences 38-40. So, these findings suggest that this may not be the primary mechanism responsible for gingival overgrowth.
Synthesis and degradation of collagen Type I
Collagen is the most abundant protein in mammals. Its synthesis and degradation are precisely balanced by the regulatory mechanisms. It has been proposed that gingival overgrowth occurs due to the loss of homeostasis of the synthesis and degradation of collagen fibers, especially collagen Type I, resulting in the excessive accumulation of collagen fibers 41.
The immunohistochemical analysis of drug-induced gingival overgrowth in rat models has shown an excessive accumulation of collagen Type I in gingival connective tissue 42, 43. This may be due to various degrees of gingival inflammation, because of which the production of inflammatory cytokines, such as interleukin 1β is increased. This cytokine is known to stimulate the gingival fibroblast proliferation and has a potential influence on collagen metabolism of fibroblasts 44-46. Individuals taking these drugs can be categorized as “responders” and “non-responders”. Studies have shown …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….
Under normal conditions, the collagen degradation occurs via phagocytic activity in gingival fibroblasts. Collagenase-mediated degradation occurs during inflammation. Studies have shown decreased collagen phagocytosis by the fibroblasts isolated from human phenytoin-induced gingival overgrowth than those isolated from healthy gingiva. Direct inhibitory effects of nifedipine and phenytoin were also shown on the collagen phagocytosis by fibroblasts 55.
Role of cytokines
As we know that subclinical inflammation is always present in the gingival sulcus because of which gingiva is always in a process of repair and remodeling. It results in unusually high collagen turnover rate in periodontal tissues 56, 57. Various cytokines and other chemical mediators are involved in this process. Research work has demonstrated that there may be an imbalance between these cytokines in gingival overgrowth. Cytokines and growth factors found in elevated levels, in human drug-induced gingival overgrowth, include interleukin-6 (IL-6), IL-1β, platelet-derived growth factor-B (PDGF-B), fibroblast growth factor-2 (FGF-2), transforming growth factor-β (TGF-β), and connective tissue growth factor (CTGF) 37,58-64. The exact mechanism, how these drugs cause cytokine imbalance is still being studied, but the proposed mechanisms indicate the immunomodulatory effects of these drugs.
Role of α 2 integrins
Integrins are heterodimeric transmembrane cellular receptors responsible for signaling mechanism from exterior to interior of the cells. Each heterodimer consists of an α and β subunit. There are approximately 17α and 8β subunits in mammals, and through different combinations, they can form approximately 40 different integrins 65-68. The α1β1 and α2β1 integrins are cell surface receptors for collagens, and cells expressing the α1β1 integrin preferentially adhere to collagen Type IV, whereas cells expressing α2β1 preferentially adhere to collagen Type I. The α2β1 integrins have been shown to …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….
Calcium and collagen phagocytosis
Calcium is an important molecule that participates in the intracellular signaling. All the drugs which are shown to cause gingival enlargement in one or the other way, disturb the intracellular calcium flux. The calcium channel blockers are able to block the influx of calcium ions into the cells and to reduce oxygen consumption 73, 74, phenytoin act as a calcium channel antagonist and inhibit calcium ion flux 75 and cyclosporin A is reported to inhibit the release of calcium from intracellular stores, including endoplasmic reticulum and mitochondria 76.
As we know that α2β1 integrins are important molecules responsible for fibroblast attachment to collagen fibers, their expression requires intracellular signaling which in turn requires calcium ions 77. So, one more proposed pathway of pathogenesis of drug-induced gingival overgrowth is the disturbance of calcium ion flux in the cell, causing reduced expression of α2β1 integrins and reduced fibroblast attachment and phagocytosis.
Alterations in the role of matrix metalloproteinases (MMPs)
MMPs are calcium-dependent, zinc-containing endopeptidases. As already discussed, calcium has an important role in intracellular homeostasis and drugs responsible for gingival overgrowth have been shown to have inhibitory effects on calcium ion influx across cell membranes. So, it was proposed that this may lead to decreased synthesis and function of intracellular collagenases 78. An in vitro study has shown that treatment of fibroblasts with cyclosporine A caused significantly reduced levels of MMP-1 and MMP-3 secretion which can be related to the accumulation of extracellular matrix components 79.
Fibroblast subpopulations
Within the normal connective tissue, fibroblasts appear similar at the light-microscopic level; however, a lot of evidence indicates that such cells are functionally different 80-82. Discrete and phenotypically stable …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Role of androgen metabolism
One proposed mechanism of drug-induced gingival overgrowth is the activation of gingival fibroblast subpopulation by these drugs and as a result the conversion of androgens to their active metabolites. For example, it has been shown that monolayer cultures of gingival fibroblasts readily metabolize labeled testosterone to its active metabolite 5α-dihydro testosterone (5α-DHT). The addition of phenytoin/ cyclosporin to this culture further promotes the formation of active metabolites. These active metabolites can act on the “target fibroblast cell population” and can activate these cells to produce more collagen fibers or decrease collagenases activity 87, 88.
Genetic factors
The group of drugs which have been shown to be responsible for gingival overgrowth is metabolized in the body by cytochrome P450 enzyme family. Dihydropyridines and cyclosporin are metabolized by CYP3A4 89 and phenytoin is metabolized by CYP2C9 90. Genetic polymorphism is found in Cyt P450 genes. This polymorphism may lead to the variations in inter-individual drug metabolism. Although, the exact mechanism is not clear, but this may be one of the mechanisms involved in drug-induced gingival overgrowth.
Another evidence for genetic factors involved in gingival overgrowth comes from the human leukocyte antigen (HLA) expression. One investigation done on patients taking cyclosporin and/or dihydropyridine has elucidated that HLA-DR1 +ve patients had significantly lower gingival overgrowth as compared to HLA-DR2 +ve patients 91. So, higher frequency of HLA-DR2 expression is associated with moderate to severe gingival overgrowth.
Prevention and management of drug-induced gingival overgrowth
Maintenance of good oral hygiene by the patient and professional help in achieving it are the two major factors in minimizing gingival overgrowth. Gingival overgrowth increases the amount of plaque accumulation because of formation of pseudopockets. It further increases the gingival inflammation and hence inflammatory gingival hyperplasia. Investigations have shown that aggressive plaque control and routine oral hygiene help in maintaining gums, but may not prevent the onset of gingival overgrowth in some individuals 92. A frequent follow-up of the patient (bi-weekly) is also helpful in preventing or limiting gingival overgrowth.
The treatment consists of …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….
Idiopathic gingival enlargement
As the name suggests, these enlargements are due to some unidentified cause. Common terms used for these enlargements include gingivomatosis, elephantiasis, idiopathic fibromatosis, hereditary gingival hyperplasia, and congenital familial fibromatosis.

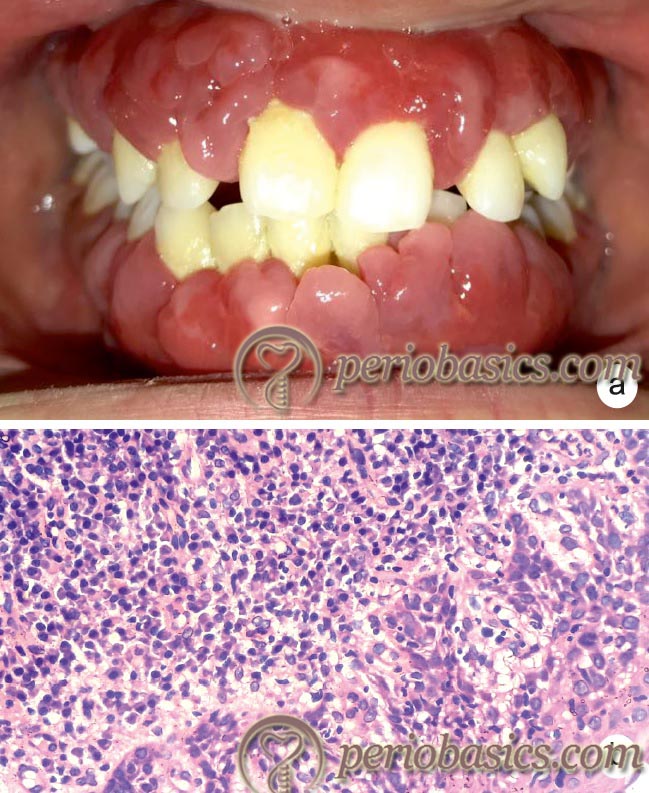
Hereditary gingival fibromatosis (HGF)
It represents a heterogeneous group of disorders characterized by progressive enlargement of the gingiva. It may appear as an isolated entity, i.e. as an autosomal dominant gingival fibromatosis or as a part of a syndrome.
Clinical presentation
Clinically, HGF develops as a slowly progressive, benign, localized or generalized enlargement of keratinized gingiva. In severe cases, the gingiva may cover the entire crown of the tooth. Both sexes are equally affected by this condition. The onset of gingival overgrowth is usually along with the eruption of permanent incisors but in some cases, it starts with the eruption of primary dentition. In the localized form of HGF, maxillary tuberosity …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….
Histology
A peculiar histopathological finding in this condition is the accumulation of excess extracellular matrix (ECM). The histologic section of gingiva presents as dense, hyperkeratotic epithelium with elongated rete ridges. Epithelial hyperplasia can also occur as a consequence of acanthosis, but this was found only in areas of chronic inflammation 98, 99. Increased numbers of bundles of collagen fibers are found randomly in all directions with a few fibroblasts and blood vessels 100, 101. There is also an accumulation of elastic and oxytalan fibers 102, 103.
Inflammatory infiltrate is found only where there are local factors (like plaque) present due to the formation of pseudo pockets. Researchers have demonstrated two types of fibroblast populations in the histological sections, one with little cytoplasm around the nucleus, which is associated with dense collagen bundles and the other contains prominent cytoplasm with well-developed organelles. These fibroblasts have been considered as inactive and active, respectively 104, 105.
Studies have demonstrated increased expression of transforming growth factor (TGF) 106. It may lead to excessive production of extracellular matrix. Along with this, there is reduced expression of matrix metalloproteinases and increased expression of tissue inhibitors of matrix metalloproteinases, which further supports the accumulation of extracellular matrix 107.
Combined enlargement (fibrotic + inflammatory)
This type of gingival enlargement occurs in patients who have a poor oral hygiene and pre-existing fibrotic gingival enlargement. Here, the gingival enlargement has both fibrotic and inflammatory components due to inadequate maintenance of oral hygiene in the presence of pre-existing fibrotic gingival enlargement.

Enlargement associated with systemic conditions/ diseases
Conditioned gingival enlargement
This type of gingival enlargement occurs when the systemic condition of the patient is such as to exaggerate or distort the usual gingival response to local irritation and produces a corresponding modification of the usual clinical features of chronic gingivitis. The specific manner in which the clinical picture of conditioned gingival enlargement differs from chronic gingivitis depends on the nature of the modifying systemic influence. Presence of plaque biofilm is necessary for the initiation of this type of gingival enlargement. The biofilm however, does not solely determines the nature of its clinical features. The conditioned gingival enlargements are usually associated with hormonal changes (pregnancy, puberty), nutritional deficiency (vitamin C deficiency), allergic (plasma cell gingivitis) and sometimes nonspecific conditioned gingival enlargement is also seen.
Pregnancy-associated gingival enlargement
The clinical manifestation of plaque-induced gingival inflammation is modulated by the hormonal imbalances during pregnancy. Hormonal changes can significantly potentiate the effects of local irritants on gingival connective tissue 108. Research has shown that by the end of third trimester, progesterone and estrogen reach peak plasma levels of 100 and 6ng/ml, respectively, which represent 10 and 30 times the levels observed during the menstrual cycle 109. The levels of sex steroid hormones in saliva also increase during pregnancy 110. The incidence of gingivitis in pregnancy varies from around 50% to 100% 111. The gingival inflammation typically begins in the second month and reaches the maximal level during the eighth month of pregnancy 112, 113.
It is important to note that pregnancy …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….

Marginal gingival enlargement in pregnancy
It is a consequence of exaggeration of existing inflammation in the pregnant patient. The clinical presentation may vary from patient to patient. It is usually generalized with the involvement of interdental papilla regions more commonly as compared to other regions of the gingiva. The involved gingiva is usually bright red or bluish in color (depending on vascularity), with the smooth and shiny surface. Bleeding may occur spontaneously or with slight provocation due to high vascularity.
Localized gingival hyperplasia associated with pregnancy
It is also known as pregnancy-associated pyogenic granuloma or pregnancy tumor or pregnancy epulis (Figure 25.10). It manifests as a painless, sessile or pedunculated, ulcerated lesion sized a few millimeters to several centimeters with a smooth or lobulated surface and purplish-red to deep blue color, according to the vascularity 115, 118. It often appears during the 2nd or 3rd month of pregnancy, presenting clinically as a tumor-like gingival enlargement due to an exaggerated conditioned response to minor trauma 119. This lesion occurs most commonly in the maxillary anterior region with the interdental papilla region being most commonly affected.
Gingival enlargement during puberty
Puberty involves a complex process of sexual maturation and it is responsible for changes in physical appearance and behavior that are related to increased levels of the steroid sex hormones, testosterone in males and estradiol in females 120. The incidence and severity of gingivitis in adolescents are influenced by a variety of factors, including plaque levels, dental caries, mouth breathing, crowding of the teeth and tooth eruption. Puberty associated gingival enlargement may occur in females as well as males and is characterized by the onset of exuberant inflammation of the marginal gingiva and, by direct extension, in the adjacent attached gingiva, especially in the interdental papillae 121,122. Bleeding from gingiva is usually the chief complaint of the patient. The enlargement is primarily present on the buccal/labial surfaces but the lingual surfaces are usually unaffected 123. The main reason for this condition, along with poor oral hygiene, is the changes in subgingival microbiota 124, 125.
Microbiological investigations have demonstrated an increase in P. intermedia in subgingival plaque. These bacteria have been shown to substitute estrogen and progesterone for vitamin K, an essential bacterial growth factor 116, 126. Other microbial species that have been shown to be increased in subgingival plaque include spirochetes, Capnocytophaga species, Actinomycetes species, and Eikenella corrodens 127, 128. The increased gingival bleeding has been shown to be associated with the increasing number of Capnocytophaga species 128.
Vitamin-C deficiency
Prolonged deficiency of vitamin-C (ascorbic acid) in the diet causes scurvy, which is characterized by general weakness, anemia, gingivitis and skin hemorrhages. Avitaminosis-C is primarily associated with defective …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
The histological features are dilated subepithelial blood vessels, engorged with red blood cells. The vessel walls are thin, and in some areas, there is hemorrhage into the surrounding connective tissue where the vessels have ruptured. There is periodontal breakdown which includes alveolar bone resorption, with the loosening and loss of teeth 132. The alveolar blood vessels lose support and develop capillary fragility which allows easy hemorrhage, caused by even minor trauma such as chewing soft food 133. Administration of Vitamin- C mediates the regeneration of collagen that facilitates the maintenance of the integrity of the tooth attachment elements.
Plasma-cell gingivitis
Plasma-cell gingivitis (synonyms: Plasmacytosis of the gingiva, Plasma cell-gingivostomatitis, Allergic gingivitis, Atypical gingivitis) 134 is a rare benign inflammatory condition of unknown etiology. Most of the times this condition has been associated with an allergic response to allergens like mint, cinnamon which are present in the toothpaste and chewing gums. Other categories of this disease can be neoplastic lesions or lesions of unknown causes 135. This condition is characterized by a sharply demarcated, erythematous, oedematous, diffuse gingivitis which often extends into the mucogingival junction. Usually, a sharp demarcation along the mucogingival border is evident. Three categories of plasma cell gingivitis have been proposed based on the etiology of the condition 136,
- Lesions caused by an allergen.
- Neoplastic lesions.
- Lesions of unknown origin.
This condition is not associated with attachment loss, but stippling is absent in the involved area of gingiva. The lesion is friable and frequently bleeds with minimal trauma 137.
Histopathological evaluation of the lesion demonstrates …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….
Nonspecific conditioned enlargement
Pyogenic Granuloma:
Pyogenic granuloma is a relatively common, soft tissue tumor of the oral cavity that is believed to be reactive and not neoplastic in nature. The name pyogenic granuloma is a misnomer, since this condition is not associated with pus and does not represent a granuloma, histologically 138. It is also called as “Granuloma gravidarum,” or “Pregnancy tumor”, when it occurs in a pregnant woman.

It is a reactive inflammatory process filled with proliferating vascular channels, immature fibroblastic connective tissue and scattered inflammatory cells. This lesion most frequently develops on the buccal gingiva in the interproximal tissue between teeth. Females are far more susceptible than males because of the hormonal changes that occur in women during puberty, pregnancy, and menopause. Clinically, it appears as a smooth or lobulated exophytic lesion manifesting as small red erythematous plaque on a pedunculated or sometimes a sessile base, which is usually hemorrhagic and compressible.
The microscopic examination reveals highly vascular proliferation that resembles the granulation tissue. Numerous small and large blood vessels are seen engorged with red blood cells. This feature makes this lesion highly vascular and it bleeds profusely after trauma or during surgical excision. There is the presence of ulcerated mucosa, covering a core of cellular fibrous connective tissue admixed with proliferating vascular channels and a mixed inflammatory infiltrate. Altho-ugh pyogenic granuloma can be diagnosed clinically with considerable accuracy, radiographic and histopathological investigations, aid in confirming the diagnosis and treatment.
Gingival enlargement associated with systemic diseases
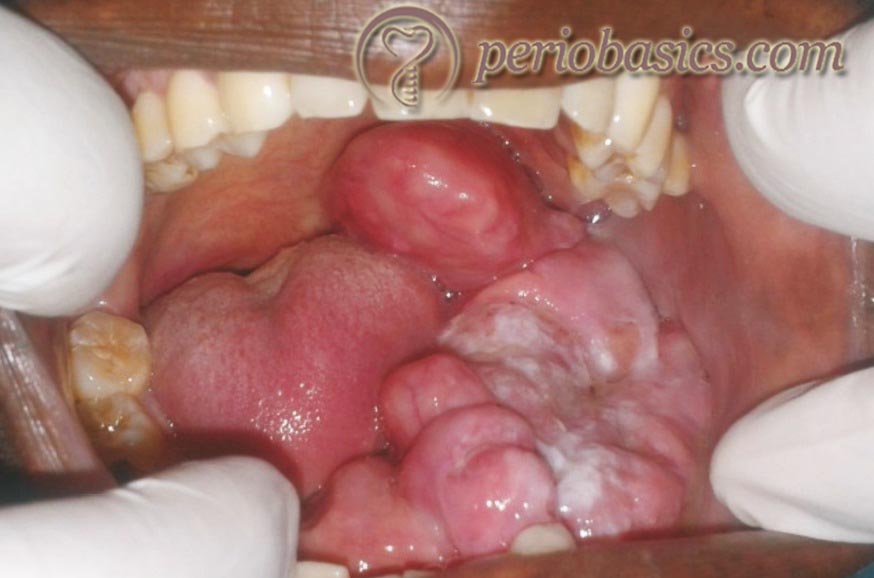
Leukemic gingival enlargement
Leukemia is a malignant neoplasm resulting from the proliferation of abnormal hemopoietic stem cells with uncoordinated differentiation, regulation and apoptosis 139. Leukemia is characterized as acute or chronic (according to its clinical behavior), and as lymphocytic and myelocytic (according to its histogenetic origin). The basic forms are acute lymphocytic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL), and chronic myeloid leukemia (CML). ALL and AML are further subdivided within the French-American-British (FAB) classification according to their degree of differentiation along cell lines and extent of cell maturation.
AML is commonly classified into 8 subgroups according to the FAB classification system. AML is the most serious condition associated with gingival enlargement. The leukemic infiltrates have been reported in the kidneys, lungs, bowels, breasts, testes, eyes, meninges, lymph nodes, liver, prostate, skin, and oral cavity 140. Gingival tissues are considered more susceptible to leukemic cell infiltration because of their microanatomy and expression of endothelial adhesion molecules which enhance the infiltration of leukocytes 141.
Gingival enlargement is more frequently seen in the context of acute rather than chronic leukemia 142, 143. Oral manifestations in a patient with leukemia have been described in all subtypes of AML, CML, ALL, and CLL 144. Gingival infiltration of leukemic cells is …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….
Pathogenesis of periodontal involvement in leukemia
Investigations have demonstrated that leukemic gingival enlargement is mostly due to plaque-induced inflammation since stringent plaque control appears to resolve the swelling 147. The gingival connective tissue is infiltrated by leukemic cells that create gingival pockets where bacterial plaque accumulates. It causes the initiation of secondary inflammatory lesion that also contributes to the enlargement of the gingiva. Gingival bleeding which is commonly seen in these patients is due to thrombocytopenia.
Clinical findings
The clinical features include enlarged gingiva with rounded margins. Gingiva appears swollen, devoid of stippling and pale red to deep purple in color. In severe cases, the interdental papillae are involved with gingival enlargement partially covering crowns of the teeth. Mucosal hemorrhages, ulcerative gingivitis, infectious gingivitis and odontalgia may be observed 148, 149. Spontaneous hemorrhage, petechiae, and ulceration have been described to occur more frequently in acute than in chronic leukemia 150.
Microscopic features
Microscopic examination of gingiva demonstrates dense, diffuse infiltration of predominantly immature leukocytes which tend to displace the normal connective tissue components of the gingiva. These cells are characterized by abundant mitotic figures. The lamina propria is densely packed with leukemia cells extending from the basal cell layer of the epithelium into the gingiva, thereby altering the normal anatomy. The blood vessels are distended and predominantly contain leukemic cells, and the RBCs are reduced in number. Epithelium covering the connective tissue may become thin or hyperplastic.
Granulomatous diseases
Wegener’s granulomatosis
It is a rare disease, in which the blood vessels and other tissues become inflamed. The hallmarks of this potentially fatal disorder are necrotizing granulomatous inflammation involving the upper and lower respiratory tract, glomerulonephritis, and vasculitis 151-154. It was first described by Klinger in 1933. In 1936 Wegener reported three patients with similar clinical features and published his findings on their distinct clinical and histopathologic findings. He postulated term ‘septic’ vasculitis 155.
In Wegener’s granulomatosis, the most characteristic oral lesion is hyperplastic gingivitis, which is typically red to purple with many petechiae (strawberry gingivitis). These lesions may remain localized in the oral cavity for unusually long periods of time before multi-organ involvement occurs 156, 157. Histopathologically, diffuse mixed inflammatory cell infiltrate comprising mostly of neutrophils, which form subepithelial abscesses, can be seen. Along with this, scattered multinucleated giant cells, some resembling Langhan’s-type giant cells with horseshoe arrangement of their nuclei can also be seen.
Gingival enlargement associated with genetic disorders
Many genetic syndromes have gingival enlargement as one of their clinical features. For the ease of understanding these conditions can be divided into four categories: hereditary gingival fibromatosis associated with syndromes, lysosomal storage disorders, vascular disorders and genetic dental abnormality disorders. The following table describes the list of genetic disorders associated with gingival enlargement,


Neoplastic gingival enlargement (gingival tumor)
The benign or malignant tumors of gingiva are also responsible for gingival enlargement. Only a brief description of some benign and malignant gingival enlargements is given here, for their detailed description readers are advised to go through oral pathology books/articles.
Benign tumors
Fibroma:
Fibromas are benign tumors that are composed of fibrous connective tissue. They are the most common“tumor” of the oral cavity. Other synonyms for this condition are irritational fibroma/traumatic fibroma/focal fibrous hyperplasia/fibrous nodule/fibroepithelial polyp. Most fibromas are sessile, although some are pedunculated. They range in size from tiny lesions that are only a couple of millimeters in diameter to large masses that are several centimeters across. Histopathological examination shows the nodular mass of fibrous connective tissue covered by stratified squamous epithelium. The collagen bundles may be arranged in a radiating, circular or haphazard fashion. The covering epithelium often demonstrates atrophy of the rete ridges because of the underlying fibrous mass. Surgical excision is the treatment of choice for this condition.

Papilloma:
It is a benign proliferation of the stratified squamous epithelium, which results in a papillary or verrucous exophytic mass induced by human papillomavirus (HPV) 158, 159. Most commonly papillomas are induced by HPVs 6 and 11 subtypes of HPV. It may occur anywhere in the mouth with a predilection for the ventral tongue and frenum area, palate, and mucosal surface of the lips. Non-keratinized lesions appear coral pink; if keratinized, they are white. Some have a cauliflower surface, whereas others have discrete finger-like projections.
Cemento-ossifying fibroma
Cemento-ossifying fibroma is a benign fibro-osseous lesion. It is most commonly seen in the third and fourth decades of life 160-162 and is more frequent in women than in men (4:1). The most common location is the mandible, counting for 70-90% of all cases 163. It starts as a slow-growing intrabony mass that is normally well delimited and asymptomatic-though over time the lesion may become large enough to cause facial deformation. Radiographically, it appears as a well delimited unilocular lesion containing variable amounts of radiopaque material. Histologically, a well-vascularized fibro-cellular tissue with the capacity to form immature bone trabeculae and cementoid tissue can be seen.
Peripheral giant cell granuloma
Peripheral giant cell granuloma is a benign hyperplastic lesion of the gingiva arising interdentally or from the gingival margin and may be sessile or pedunculated. It is also known as giant cell epulis/ giant cell reparative granuloma/ osteoclastoma/ giant cell hyperplasia. It is a reactive exophytic growth of the gingiva and the alveolar ridge which originates from the periosteum or periodontal ligament. Histological features reveal a non-capsulated mass of tissue, containing a large number of young connective tissue cells and multi-nucleated giant cells. Hemorrhage, hemosiderin, inflammatory cells, and newly formed bone or calcified material may also be seen throughout the cellular connective tissue.
Leukoplakia
It is defined as a white patch or plaque which cannot otherwise be characterized clinically or pathologically as any other disease. It appears white usually because of three main factors, alone or in combination: hyperkeratosis or excessive production of keratin (the white flakes that come off when you scratch your skin), thickening of the surface layer of cells, or the presence of pre-cancer (“dysplasia”) or cancer. One article has discussed leukoplakia in detail 164.
Malignant Tumors
Carcinoma
Oral squamous cell carcinoma (SCC) is the most common malignant tumor of the oral cavity. It accounts for about 90% of oral cancers and mostly affects adult males, predominantly alcohol, and tobacco users, between the sixth and seventh decades of life 165. The most affected sites in decreasing order are the tongue, oropharynx, lip, floor of mouth, gingiva, hard palate, and buccal mucosa 166-168. The clinical characteristics of SCC vary from case to case and include the exophytic (verrucous or papillary), endophytic, ulcerated, leukoplastic, erythroplastic or erythroleukoplastic forms. Depending on their extent and/or location, these lesions may cause painful symptoms and resorption of the adjacent bone, seen as “moth-eaten” appearance on the radiographs.
In most cases, the histopathological analysis shows malignant neoplasia of epithelial origin characterized by invasive proliferation of nests and cords of neoplastic epithelial cells. These neoplastic cells show characteristics like intense cellular and nuclear pleomorphism, nuclear hyperchromatism, loss of cell cohesion, multiple and clearly visible nucleoli, individual cell keratinization, atypical mitoses, and formation of keratin pearls.
Malignant Melanoma
Malignant melanoma is a cancer of pigmented cells, called melanocytes. Melanocytes are neural crest-derived cells that migrate to the skin, mucous membranes and several other sites. The most frequently involved sites in the oral cavity are the palate and maxillary gingiva 169, 170. Mucosal melanomas are considered to be more aggressive tumors as compared to cutaneous melanomas and they are more inclined to metastasize to regional and distant sites. They also reoccur locally or regionally, resulting in a high rate of disease-specific death.
The histopathological analysis shows proliferation of atypical melanocytes characterized by hyperchromatic and angular nuclei with infrequent mitotic activity. The melanocytes may be arranged irregularly at the epithelial-connective tissue interface or may be distributed in aggregates. The invasive pattern in which the melanoma extends into the connective tissue is represented in 30% of all oral melanoma cases.
Sarcomas
These are cancers of mesenchymal cell origin. They are rarely found in the oral cavity. However, Kaposi sarcoma has become more prevalent due to increased cases of AIDS. The details of these lesions can be studied in oral pathology books.
False enlargement
As the name indicates, false enlargements are those that do not originate from gingiva but from the underlying tissue. The gingiva is healthy and normal in size, but the enlargement is present in the underlying tissues, like bone. These enlargements may be of osseous or dental origin. The most common osseous condition is tori or exostoses. Other less common conditions include Paget’s disease, fibrous dysplasia, cherubism, central giant cell granuloma, ameloblastoma, osteoma, and osteosarcoma.

Dental conditions include “developmental enlargement”. During tooth eruption, the gingival covering of the tooth gives a false gingival enlargement like appearance. This is not a pathological condition and is resolved with the complete eruption of the crown of the tooth. However, these conditions should be carefully examined and differentiated from other pathological gingival enlargements discussed earlier in this chapter.

Treatment of gingival enlargement
In the previous sections, we discussed various causes of gingival enlargement. The treatment of various types of gingival enlargements depends upon the cause of the enlargement. The inflammatory gingival enlargement is the most common type of gingival enlargement and its treatment involves the removal of local factors, that is, plaque and calculus. Once the local factors are removed, the inflammation starts subsiding and gradually, the size of the gingiva comes to its normal state. However, if the gingival enlargement doesn’t subside after scaling and root planing, other causes of the gingival enlargement should be suspected.

Fibrotic gingival enlargement is commonly caused by drugs. Nowadays, many patients are on anti-hypertensive drugs. Calcium channel blockers can cause gingival enlargement as one of their side effects. Along with this, anti-epileptic drugs and immunosuppressants may also …….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
The treatment of other types of gingival enlargements such as those caused due to systemic diseases such as leukemia, granulomatous diseases, and benign or malignant neoplasms should be treated considering the systemic condition of the patient and extent of involvement.
Conclusion
Gingival enlargement/overgrowth is a common finding in patients. The correct diagnosis of gingival enlargement is of great importance because as discussed above, many local and systemic causes may cause gingival enlargement. Drug-induced gingival enlargement is a common side effect of some medications. Research work is going on to find out the exact mechanism of drug-induced gingival overgrowth, so that once we are clear with its pathogenesis, the treatment modalities can be worked upon.
References
References are available in the hard-copy of the website.
Suggested reading

