Introduction to indices
The index is defined as a numerical value describing the relative status of the population on a graduated scale with definite upper and lower limits which is designed to permit and facilitate comparison with other populations classified by the same criteria and methods 30. With the help of indices, various populations can be compared classified by the same criteria and methods. There are a large number of indices used for recording gingiva and periodontal status. The selection of an index for a particular study depends on its reliability and validity. Reliability of an index is its ability to produce same results when applied to an individual twice or more at a particular time. The validity of an index is its ability to measure what it is intended to measure. For example, periodontal pocket depth is not a valid indicator of attachment loss. In the case of gingival enlargement, pseudo-pockets are present but attachment loss is not there. Thus, pocket depth cannot be considered as a valid indicator of periodontal disease.
There are some inherent drawbacks associated with the use of indices. Most of the diseases cannot be quantified by objective means. Furthermore, the data obtained by indices is subjected to examiner variations such as training, and clinical experience. The analysis of data obtained by many indices is complicated by the fact that most index systems follow an ordinal scale and are non-parametric in nature.
Classification and characteristics of various indices
The indices used to record gingival and periodontal status of the patient can be divided into following categories,
- Oral hygiene indices,
- Plaque and debris assessment indices
- Gingival indices
- Periodontal indices and
- Miscellaneous indices (CPITN, CPI, retention index, alveolar bone loss, and mobility index).
Oral hygiene indices
The assessment of oral hygiene with the help of indices helps the clinician to judge patient’s compliance to oral hygiene instructions and also act as a motivational tool for the patients. There are various oral hygiene indices used, including oral hygiene index, simplified oral hygiene index, modified patient hygiene performance index, plaque-free score index, oral health status index, etc. We shall discuss in detail the oral hygiene index and simplified oral hygiene index in the following sections.
Oral hygiene index (OHI):
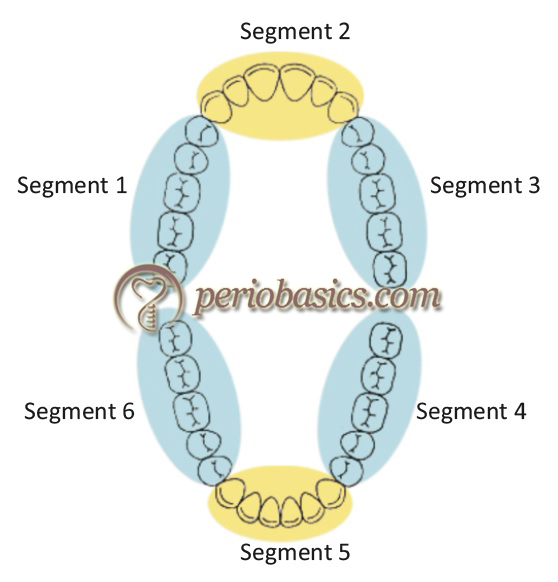
Greene and Vermillion 31 in 1960 developed this index which consisted of two components, the debris index, and the calculus index. This index assesses the oral cleanliness of an individual. The scores obtained from debris or calculus index may be used individually or in combination. The dentition is divided into six sextants as follows,
Sextant 1: segment distal to right upper cuspid
Sextant 2: upper right canine to left canine
Sextant 3: segment distal to left upper cuspid
Sextant 4: segment distal to left lower cuspid
Sextant 5: lower left canine to right canine
Sextant 6: segment distal to right lower cuspid
Each sextant is examined for debris or calculus. For each segment, buccal and lingual surface of one tooth is used for calculating the individual index for that particular sextant. The tooth having greatest amount either debris or calculus from each sextant is used for scoring.
Scoring criteria
The scoring criteria for debris and calculus index are as follows,
Debris index
| Scores | Criteria |
|---|---|
| 0 | No debris or stains present. |
| 1 | Soft debris covering not more than one-third of the tooth surface being examined or the presence of extrinsic stains without debris regardless of surface area covered. |
| 2 | Soft debris covering more than one-third, but not more than two-thirds of the exposed tooth surface. |
| 3 | Soft debris covering more than two-thirds of the exposed tooth surface. |
Calculus index
| Scores | Criteria |
|---|---|
| 0 | No calculus present. |
| 1 | Supragingival calculus present, covering not more than one-third of the tooth surface. |
| 2 | Supragingival calculus covering between one and two-thirds of the tooth surface, or scattered subgingival calculus. |
| 3 | Supragingival calculus covering more than two-thirds of the tooth surface, or a continuous heavy band of subgingival calculus around the tooth. |
The OHI score is calculated initially by calculating the DI and CI scores and dividing the total scores for each tooth by the number of sextants. The DI and CI scores are then added to determine an OHI score. Score 0 (lowest) indicates absolute oral hygiene and score 12 (highest) indicates worst oral hygiene.
Oral hygiene index simplified (OHI-S)
The oral hygiene index was simplified by Green and Vermillion 32 in 1964. In the simplified index, they included only six teeth surfaces rather than twelve. The six surfaces are selected from 4 posterior and 2 anterior teeth.
Selection of teeth:
The following criteria are used for the selection of teeth in a given sextant,
- In posterior sextants, first fully erupted tooth distal to the second bicuspid usually the first molar, but sometimes the second or third molar is selected for examination. The buccal surfaces of the selected upper molars and the lingual surfaces of the selected lower molars are inspected.
- In the anterior sextants, labial surfaces of the upper right and the lower left central incisors are scored. In the absence of either of these anterior teeth, the central incisor on the opposite side of the midline is substituted.

Scoring criteria:
The mouth mirror and shepherd’s crook or sickle type explorer are used for examining the tooth surfaces. The explorer is placed on the tooth surface to be examined and is moved obliquely from distal gingival crevice to mesial gingival crevice. Scoring criteria of teeth is similar to as explained earlier in OHI. Once the scores for debris and calculus have been recorded, the index values are calculated. For each individual, the debris scores are totalled and divided by the number of surfaces scored.
Individual scores:
Individually, DI-S and CI-S are scored as follows,
0.0-0.6 = good oral hygiene
0.7-1.8 = fair oral hygiene
1.9-3.0 = poor oral hygiene
Overall OHI-S score,
0.0-1.2 = good oral hygiene
1.3-3.0 = fair oral hygiene
3.1-6.0 = poor oral hygiene
Plaque and debris assessment indices
Many indices have been designed to specifically measure plaque and debris. These include plaque component of periodontal disease index (PDI), Schick and Ash modification of plaque criteria of PDI, plaque index, modified navy plaque index, distal mesial plaque and Turesky, Gilmore and Glickman modification of Quigley and Hein plaque index.
Plaque component of periodontal disease index (PDI)
PDI has dental plaque and calculus components which are used to calculate plaque and calculus score for a particular patient. For estimation of plaque and debris, teeth are stained with a disclosing solution and scored (discussed later in PDI).
Plaque Score (PS)
It was given by Schick and Ash 33 in 1961, designed to measure the amount of plaque on the clinical crown of the teeth. The interproximal areas are not considered in the scoring. Six teeth are used for scoring and scoring is confined to the gingival part of the facial and lingual surfaces of the index teeth. The scores are summed up for each tooth to assess plaque accumulation for each individual. The score is then divided by the maximum possible score and is then converted into a percentage.
Plaque index (PI)
PI was developed by Silness and Lӧe in 1964. The index assesses the thickness of plaque at the cervical margin of the teeth. Four areas are examined in this index: ………….. Content available in the book…………….. Content available in the book…………… Content available in the book…………… Content available in the book……
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Score interpretation:
The PI score for an individual is calculated by summing up all the scores and dividing by the number of teeth examined.
Scores are interpreted as follows,
0 = Excellent
0.1-0.9 = Good oral hygiene
1.0-1.9 = Fair oral hygiene
2.0-3.0 = Poor oral hygiene
Patient hygiene performance index (PHP)
This index was introduced by Podshadley and Haley 34 in 1968. It is used to assess individual oral hygiene performance. It is used to assess the remaining plaque and debris after the patient performs brushing. Its primary use is as a motivational and educational tool for the patient.
Selection of teeth and surfaces:
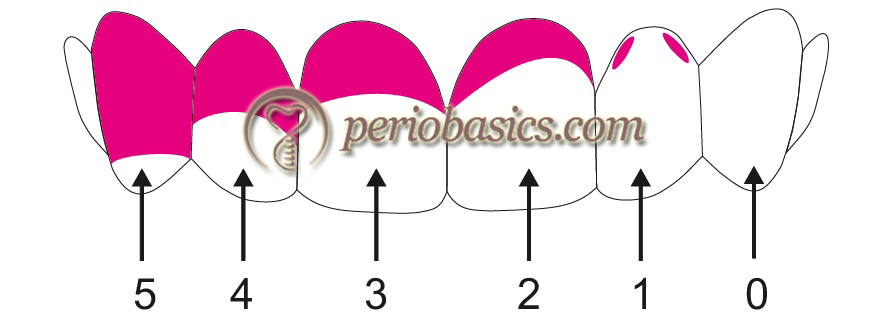
Teeth selected are same as in the OHI-S but divides each tooth surface into five principal areas as shown in figure 19.3. Each tooth surface to be evaluated is divided into mesial, middle and distal thirds. The middle third is further divided into the gingival, middle and occlusal third. Within each surface area, the debris is scored on a yes or no basis, i.e. for no debris, 0 score is given and for the presence of debris, 1 score is given.

Scoring criteria:
The scoring is done by calculating total debris score divided by the number of teeth scored. On the basis of scoring following inferences are drawn,
Turesky, Gilmore, Glickman modification of Quigley-Hein plaque index
The Quigley-Hein plaque index was defined by G A Quigley and J W Hein in 1962. It evaluated the plaque revealed on the buccal and lingual non-restored surfaces of the teeth on a scale of 0 to 5. This index focussed on the gingival third of the tooth. They examined only the facial surface of the anterior teeth using basic fuchsine mouthwash as a disclosing agent. The index was modified by S Turesky, N D Gilmore, and I Glickman in 1970. In the modified index, all teeth except the third molars are assessed. Plaque is assessed on the labial, lingual and buccal surfaces of all the teeth after using a disclosing agent. An index for the entire mouth is determined by dividing the total score by the number of surfaces examined. A score 0 or 1 is considered low; whereas, a score 2 or more is considered high. The scoring system is as follows,
| Scores | Criteria |
|---|---|
| 0 | No plaque |
| 1 | Separate flecks of plaque at the cervical margin of the tooth |
| 2 | A thin continuous band of plaque (up to one mm) at the cervical margin of the tooth |
| 3 | A band of plaque wider than one mm but covering less than one-third of the crown of the tooth |
| 4 | Plaque covering at least one-third but less than two-thirds of the crown of the tooth |
| 5 | Plaque covering two-thirds or more of the crown of the tooth |
Gingival indices
The gingival indices are used to record the gingival status of the patient. These indices primarily check the clinical signs of inflammation which are then graded, based on specific criteria. Following is the detailed description of these indices,
PMA Index (Schour and Massler)
The PMA index was developed by Schour and Massler in 1944-1947 35-37. It is probably the oldest reversible index designed for scoring gingival inflammatory status. In this index, the facial surface of gingiva around a tooth is divided into three units: Mesial interdental papilla (P), Marginal gingiva (M), and Attached gingiva (A). The sum of P, M and A for a tooth is designated as the PMA score for a tooth and the sum of PMA score for all the teeth divided by the number of teeth is considered as PMA score of the person.
Selection of teeth and surfaces:
Papillary gingiva: Papillary portion of gingiva between the teeth is numbered by the tooth just distal to it.
Marginal collar of gingiva around the tooth: It is located around the tooth between adjacent interdental papillae and demarcated from attached gingiva by the free gingival groove.
Attached gingiva: Attached portion of the gingiva overlying the alveolar bone.
The inflammation in the papillary portion denotes mild inflammation because the inflammation starts primarily in the papillary col area. Inflammation of marginal gingiva signifies moderate inflammation because after papillary, the marginal gingiva is involved. Inflammation in the attached gingiva occurs in severe gingival inflammation, where it extends from marginal to attached gingiva.
Scoring criteria:
………..Content available in the book…………. Content available in the book…………… Content available in the book…………… Content available in the book………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Modifications of the PMA index
There are many modifications which have been suggested for PMA index. In the modification suggested by Parfitt (1957) 38, buccal and lingual gingivae were added in the index and the degree of inflammation was divided into five arbitrary levels. The severity of inflammation was evaluated for both buccal and lingual aspects separately.
Further modifications were done by Mϋhlemann and Mazor (1958) 39, Arno et al. (1958) 40, Heylings (1961) 41, Jackson (1962) 42 and others 43.
Gingival index (GI)
This index was given by Loe and Silness in 1963 44, designed to assess the severity and quality of gingival inflammation in an individual or population. The gingival inflammation is assessed on the basis of color, consistency and bleeding on probing. In this index, only gingival tissue is assessed. A blunt probe is used to assess the bleeding tendency of gingiva by running it along the soft tissue wall of the entrance of gingival sulcus. The gingiva surrounding the tooth is assessed at four sites: mesio-facial papilla, facial marginal gingiva, disto-facial papilla and lingual marginal gingiva. The lingual surface was not subdivided to minimize examiners’ variability in scoring.
Scoring criteria:
0= Normal gingiva;
1= Mild inflammation: slight change in color and slight edema but no bleeding on probing;
2= Moderate inflammation: redness, edema and glazing, bleeding on probing;
3= Severe inflammation: marked redness and edema, ulceration with a tendency to spontaneous bleeding.
Teeth examined:
GI can be calculated for all the teeth or for selected teeth. When selected teeth are examined, following teeth are considered for examination,
- Maxillary right first molar
- Maxillary right lateral incisor
- Maxillary left first bicuspid
- Mandibular left first molar
- Mandibular left lateral incisor
- Mandibular right first bicuspid.
The GI of the individual can be obtained by adding the values of each tooth and dividing by the number of teeth examined.
GI scores:
After the score is calculated for an individual, the degree of gingivitis can be classified as follows,
………..Content available in the book…………. Content available in the book…………… Content available in the book…………… Content available in the book………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Modified Gingival Index (MGI)
MGI was introduced by Lobene et al. in 1986 45. In this index modifications were done by eliminating sulcus probing and by redefining the scoring system for mild inflammation. The aim of these modifications was to improve the sensitivity of the index for lower values of the index. This is one of the most widely used indices during clinical trials on therapeutic agents.
Teeth examined:
Similar to GI, in this index also full or partial mouth assessment can be performed.
Scoring Criteria:
0: Absence of inflammation
1: Mild inflammation; a slight change in color, little change in the texture of any portion of the marginal or papillary gingival unit.
2: Mild inflammation; criteria as above but involving entire marginal or papillary gingival unit.
3: Moderate inflammation; glazing, redness, edema and/or hypertrophy of the marginal or papillary gingival unit.
4: Severe inflammation; marked redness, edema and/or hypertrophy of the marginal or papillary gingival unit, spontaneous bleeding congestion, or ulceration.
The MGI score for each tooth is obtained by totalling the scores for all the recorded surfaces around that particular tooth and dividing the value by four. Totalling all the scores per tooth and dividing by the number of teeth examined provides the MGI score per person.
Sulcus Bleeding Index (SBI)
This index was proposed by Mϋhlemann and Son in 1971 46. The index was based on the fact that one of the earliest signs of gingivitis is bleeding on probing. The criteria for scoring are as follows:
Score 0: Healthy looking papillary and marginal gingiva, no bleeding on probing;
Score 1: Healthy looking gingiva, bleeding on probing;
Score 2: Bleeding on probing, change in color, no edema;
Score 3: Bleeding on probing, change in color, slight edema;
Score 4: Bleeding on probing, change in color, obvious edema;
Score 5: Spontaneous bleeding, change in color, marked edema.
Papillary bleeding index (PBI)
Later on in 1977, Mϋhlemann 47 proposed PBI. The rationale behind proposing this index was that the inflammation starts interproximally and then involves the marginal gingiva and alveolar bone. It is a four-grade index based on both the extent of bleeding and the time it takes for bleeding to occur after stimulation with a periodontal probe. This index can be used for patient motivation to improve their gingival health. The scores are obtained by moving a probe with a blunt tip in the gingival sulcus. The probe is inserted into the gingival sulcus at the base of the papilla on the mesial aspect, and then moved coronally to the papilla tip. This is repeated on the distal aspect of the papilla. Scoring criteria are as follows,
| Score | Bleeding on gentle probing |
|---|---|
| 0 | No bleeding. |
| 1 | Only one bleeding point appearing. |
| 2 | Several isolated bleeding points or a small blood area appearing. |
| 3 | Interdental triangle filled with blood soon after probing. |
| 4 | Profuse bleeding when probing, blood spreads towards the marginal gingiva. |
Modified papillary bleeding index (MPBI)
The papillary bleeding index was modified by Barnett et al. (1980) 48, proposing modified papillary bleeding index. The rationale behind proposing this index was that the severity of inflammation is directly proportional to the spontaneity of bleeding upon gentle probing. A blunt probe is gently placed in the gingival sulcus at the mesial line angle of the tooth surface to be examined and is then carefully moved forward into the mesial papilla. The scoring is done on the basis of the appearance of bleeding following probing.
0 = no bleeding within 30 seconds of probing;
1 = bleeding between 3-30 seconds of probing;
2 = bleeding within 2 seconds of probing;
3 = bleeding immediately upon probe placement.
Scoring:
The scoring is done by calculating scores of mesial papillae, starting from the second molar to the lateral incisor. The values are obtained from maxillary left and mandibular right buccal segments, and the maxillary right and mandibular left lingual segments. These segments were selected because each mesial papilla could only be tested once, i.e. from either the buccal or lingual side.
Gingival bleeding index (GBI)
This index was proposed by Carter and Barnes in 1974 49. The index was designed for easy estimation of gingivitis in patients. Unwaxed floss is passed into the interproximal sulci of the teeth and the presence or absence of bleeding is checked. Dental floss is an easily available oral hygiene aid and can be instructed easily to the patient for self-evaluation.
Teeth examined:
The oral cavity is divided into six segments: upper right, upper anterior, upper left, lower left, lower anterior and lower right. Flossing is done in the same sequence, starting from upper right quadrant and ending at lower right quadrant.
GBI Scoring:
If the gingival inflammation is present, bleeding is immediately evident after the introduction of floss. However, thirty seconds are allowed for re-inspection of each segment. Bleeding is recorded as present or absent. If copious bleeding is present, the patient can be asked to rinse the mouth after each quadrant is examined. GBI score is obtained by noting the total units of bleeding and the total susceptible areas at risk for each patient.
Periodontal indices
Clinical attachment loss is the cardinal sign of periodontitis. It is caused by apical migration of junctional epithelium from the cementoenamel junction due to bone loss. The severity of bone loss can be determined by clinical and radiographic assessment. Gingival recession and tooth mobility also indicate the bone loss associated with the tooth.
Russell’s periodontal index (PI)
The first index assessing the prevalence and epidemiological characteristics of periodontal diseases was given by Russell in 1956. The index can be recorded solely on the basis of the clinical examination or it can make use of X-rays, if available. The scoring criteria (0, 1, 2, 6 and 8) in this index are based on the sequence of appearance of inflammation, pocket formation, and loss of function. It is a popular index used for assessing periodontal disease status in a population.
Russell’s periodontal index scores
| Score | Criteria | Additional radiographic features |
|---|---|---|
| 0 | Negative (neither overt inflammation in investing tissues nor loss of function due to the destruction of supporting tissue). | Radiographic features normal |
| 1 | Mild gingivitis (overt area of inflammation in free gingiva but this area does not circumscribe the tooth). | |
| 2 | Gingivitis (inflammation completely circumscribes the tooth but no apparent break in epithelial attachment). | |
| 4 | Used only when radiographs are available | |
| 6 | Gingivitis with pocket formation (the epithelial attachment is broken and there is a pocket. There is no interference with normal masticatory function, the tooth is firm in its socket and has not drifted). | Horizontal bone loss involving alveolar crest up to half length of the root. |
| 8 | Advanced destruction with loss of masticatory function (tooth may be loose, tooth may have drifted, tooth may sound dull on percussion with metallic instrument, tooth may be depressible in the socket). | Advanced bone loss |
Scoring criteria:
Each tooth is scored according to the condition of surrounding tissues. The scoring criteria is used is given in, The scores of each tooth are added and the total is divided by the number of teeth examined. Interpretation of the scores is as follows,
0-0.2 = clinically normal supportive tissues
0.3-0.9 = Simple gingivitis
0.7-1.9 = Beginning destructive periodontal disease
1.6-5.0 = Established destructive periodontal disease
3.8-8.0 = Terminal disease
Periodontal disease index (PDI)
PDI was introduced by Sigurd P Ramfjord in 1959 50, 51. It is the clinician’s modification of Russell’s periodontal index for epidemiological surveys of periodontal diseases. The primary objective of this index is to accurately assess the periodontal status of an individual by identifying the periodontal tissue attachment to the tooth surface in relation to the cementoenamel junction (CEJ). These measurements are useful in longitudinal studies where the effectiveness of a therapy is to be assessed in a long duration of time.
Teeth examined:
All the teeth or selected teeth can be examined in this index. If selected teeth are examined, following teeth are included in the index,
- Maxillary right first molar
- Maxillary left central incisor
- Maxillary left first premolar
- Mandibular left first molar
- Mandibular right central incisor
- Mandibular right first premolar

Scoring criteria:
There are two components of periodontium which are checked in this index: gingival inflammation and attachment loss. The gingival status is assessed by ………….Content available in the book…………. Content available in the book…………… Content available in the book…………… Content available in the book………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Dental plaque component of PDI:
For the selected teeth, 4 surfaces (facial, lingual, mesial and distal) are scored from 0-3. The disclosing agent is used to disclose the plaque on the tooth surface. Specific surfaces with disclosed plaque are observed and scored as follows,
| Score | Criteria |
|---|---|
| 0 | No plaque present |
| 1 | Plaque present on some but not all interproximal, buccal and lingual surfaces of the tooth |
| 2 | Plaque present on all interproximal, buccal and lingual surfaces but covering less than half of these surfaces |
| 3 | Plaque extends over all interproximal, buccal and lingual surfaces and covers more than half of these surfaces |
The plaque component of PDI is estimated by totalling all individual tooth scores and dividing it by the number of teeth examined.
Dental calculus component of PDI:
The calculus present on the tooth surfaces is examined by a subgingival explorer or a periodontal probe. For all the selected teeth four surfaces (facial, lingual, mesial and distal) are scored from 0-3 as follows,
| Score | Criteria |
|---|---|
| 0 | Absence of calculus |
| 1 | Supragingival calculus extending only slightly below the free gingival margin (not more than 1 mm) |
| 2 | Moderate amount of supragingival or subgingival calculus or subgingival calculus alone |
| 3 | An abundance of supra and subgingival calculus |
The calculus component of PDI is estimated by totalling all individual tooth scores and dividing it by the number of teeth examined.
Miscellaneous indices
Community periodontal index of treatment needs (CPITN)
Till late 1970’s many indices were available for the assessment of the dental and periodontal status of an individual or population groups. But, researchers had a lot of dissatisfaction with the available indices to estimate periodontal treatment needs. Considering this problem, WHO in 1977 summoned a group of experts from 14 FDI member countries to conduct a comprehensive review of the literature and suggest an index which addressed treatment needs for an individual or population groups. In this way CPITN was designed which incorporated sextant approach by O’Leary et al. (1963) 52, periodontal treatment needs system proposed by Johansen et al. (1973) 53 and principle of using dichotomous criteria for periodontal disease indicators by Ainamo et al. (1975) 54. CPITN facilitates a rapid analysis of both prevalence and treatment needs for periodontal disease. Although this index has been given name ‘community’ periodontal index of treatment needs, it can be very well adaptable to the individual patient. The final recommendation of the scoring system used in CPITN was published in 1982 by six members of joint FDIWHO group 55.
Methodology:
The dental arches are divided into six sextants as follows,
Sextant 1: segment distal to right upper cuspid
Sextant 2: upper right canine to left canine
Sextant 3: segment distal to left upper cuspid
Sextant 4: segment distal to left lower cuspid
Sextant 5: lower left canine to right canine
Sextant 6: segment distal to right lower cuspid
All the teeth can be examined for an individual. The worst score for each sextant is noted. In case of epidemiological surveys, the assessment of two teeth in the posterior sextants and one tooth in the anterior sextants is done. These index teeth examined are as follows,
………….Content available in the book…………. Content available in the book…………… Content available in the book…………… Content available in the book………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Although 10 index teeth are examined, but only 6 recordings are made one from each sextant.
CPITN probe:
A specially designed lightweight periodontal probe with 0.5 mm ball tip is used, with a black band between 3.5 and 5.5 mm and rings at 8.5 and 11.5 mm from the ball tip. The probe is made up of metal with knurled handle of diameter 3.5 mm and a maximum weight of 4.5 gm. There are two variants of this probe: CPITN-E and CPITN-C.
CPITN-E: This probe is used for epidemiological surveys and has 3.5 and 5.5 mm markings.
CPITN-C: This is a clinical probe with additional markings at 8.5 and 11.5 mm.
The tooth is probed to determine the periodontal pocket depth with a light force, not more than 25 gms. This light force can be determined by gently inserting the probe tip under finger nail and press until blanching occurs without causing pain or discomfort. The ball end of this probe has been designed to ‘sense’ the root surface. The probe tip should be gently inserted into the periodontal pocket and is moved around the root surface to assess calculus on the root surface and to reach the pocket depth. If the patient feels pain during probing, it is indicative of excessive force application during probing. The pocket depth should be examined at least at six points: mesiobuccal, midbuccal, distobuccal, mesiolingual, midlingual and distolingual.
Scoring criteria:
Upon examination with periodontal probe, following codes are listed according to the complexity of the treatment,
Code X: When only one tooth or no teeth are present in a sextant (third molars are excluded unless they function in place of second molars).
Code 0: Healthy periodontal tissues
Code 1: Bleeding elicited during or after gentle probing without calculus or pocket being present.
Code 2: The whole of the colored band of the probe is visible, but supragingival or subgingival calculus or other plaque retentive factors such as ill-fitting crowns or defective margin of a filling are either seen or felt during probing shallow pockets only. If no pockets which involve or exceed the colored area of the CPITN probe and supra or subgingival calculus or other plaque retentive factor are detected, and code 2 is given, it is not necessary to examine for gingival bleeding.
Code 3: Pathological pocket of 5 mm or less, that is, only a part of the colored band is visible. If the deepest pocket is between 3.5 mm and 5.5 mm found in a designated tooth/tooth and code 3 is given, there is no need for recording calculus or bleeding.
Code 4: Pathological pocket of 6 mm or more, that is, the black area of the CPITN probe is not visible. If the designated tooth / teeth are found to have 6 mm or deeper pockets in the sextant examined, and code 4 is given to the sextant, there is no need to record the presence or absence of pathological pockets of 4 mm or 5 mm, calculus or bleeding.
Treatment needs:
According to the scoring codes designated, the treatment needs are planned as follows,
TN 0: A recording of code 0 (health) or X (missing) for all six sextants indicates that there is no need for treatment.
TN 1: A code of 1 or higher indicates that there is a need for improving the personal oral hygiene of that individual.
TN 2:
a: Code of 2 or higher indicates the need for professional cleaning of the teeth and removal of plaque retentive factors. The patient requires oral hygiene instructions.
b: Shallow to moderate pocketing (4 or 5 mm, code 3). Oral hygiene and scaling will reduce inflammation and bring 4 or 5 mm pockets to values of or below 3 mm. Thus, sextants of these pockets are placed in the same treatment category as scaling and root planning, i.e. TN2.
TN 3:
A sextant scoring code 4 (6 mm or deeper pockets) may or may not be treated successfully by means of deep scaling and efficient personal oral hygiene measures. Code 4 is therefore assigned as a complex treatment which can involve deep scaling, root planning, and more complex procedures.
Scoring criteria for community periodontal index of treatment needs (CPITN)
| CPITN Score | Periodontal status | Treatment need |
|---|---|---|
| 0 | Healthy periodontium | No treatment |
| 1 | Bleeding observed by probing/spontaneous | Improvement of Oral hygiene |
| 2 | Calculus felt by probe; entire black area is visible | 1+ professional scaling |
| 3 | Pocket depth 4-5mm; Gingival margin on the black band | 1+ professional scaling |
| 4 | Pocket depth >6 mm; Entire black band is invisible | 1+2+ complex surgery |
Periodontal screening and recording (PSR) index
CPITN Index has been used extensively as a screening tool in clinical settings. In the year 1992, PSR index was introduced which was actually derived from the Basic Periodontal Examination (BPE). On October 6, 1993, the American Dental Association (ADA), with the endorsement of the American Academy of Periodontology (AAP) and sponsorship by the Procter & Gamble Company (P&G), officially introduced Periodontal Screening and Recording™ (PSR) as the recommended system for the early detection of periodontal disease.
The index is similar to the CPITN index, except, a new addition was done that was denoted by an asterisk (*) code. A periodontal probe similar to the CPITN probe was used in PSR index which included a 0.5 mm diameter ball tip and a colored band extending from 3.5 mm to 5.5 mm from the tip. The description of PSR codes is as follows 56:
………….Content available in the book…………. Content available in the book…………… Content available in the book…………… Content available in the book………..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
The code definitions and recommended treatment plans in PSR index
| Clinical Signs | Treatment Plan | |
|---|---|---|
| Code 0 | Absence of clinical signs | No treatment required |
| Code 1 | Bleeding on probing | Oral hygiene instructions |
| Code 2 | Supra and/or subgingival calculus and/or defective margins | Removal of calculus Correction of plaque retentive margins |
| Code 3 | Periodontal pocket 4mm to 5.5 mm deep (colored band on probe partially visible) | Removal of calculus Root planing Detailed periodontal examination of sextant or entire mouth if more than 2 sextants receive a Code 3 score |
| Code 4 | Periodontal pocket 6mm deep (colored band no longer visible) | Detailed periodontal examination of entire mouth Complex treatment |
| Code * | Periodontal abnormalities present | Detailed periodontal examination of affected sextant |
| Code X | Sextant absent or fewer than 2 teeth |
Conclusion
Periodontal diseases are multi-factorial diseases. There are many risk factors which have been shown to be associated with the progression of periodontal disease. However, epidemiological studies have shown that the association of these risk factors with periodontal disease progression varies with race, age group, socioeconomic status, etc. The exact magnitude to which these factors may affect the periodontal disease progression still needs to be investigated. However, the evidence available so far has provided us a lot of information regarding the steps required for the prevention of periodontal diseases.
References
References are available in the hard copy of the website.
Suggested reading

