Introduction
Periodontitis is a chronic inflammatory disease of bacterial origin which causes progressive destruction of the periodontium that supports the teeth 1. Our present understanding of the host-bacterial interaction emphasizes multiple complex mechanisms involved in periodontal tissue breakdown. The conventional diagnostic techniques are based mainly on clinical parameters (such as probing depth, clinical attachment level) and traditional dental radiography. These are routinely used in clinical practice because of their ease of use and their cost-effectiveness. The major drawback of these techniques is their inability to detect the active disease. New diagnostic techniques which can detect the presence of active disease, predict future disease progression, and evaluate the response to periodontal therapy, thereby improving the clinical management of periodontal patients, are desirable.
In the following discussion, we shall discuss in detail the advances in various periodontal diagnostic techniques including the microbiological, immunological, molecular and radiographic diagnostic techniques
Historic developments in our understanding of periodontal disease progression
Before 1970’s the periodontitis was believed to be a slowly progressive condition which continues for a long duration of time, resulting in a periodontal bone loss. Path changing developments in this field took place in the late 1970s and early 1980s, when landmark studies by Socransky and colleagues 2, 3 changed the prevailing concept of periodontal disease from being a slow, continuously progressing disease to the one where periodontal attachment loss occurs in random bursts with periods of exacerbation and quiescence. They described active and passive periods of disease activity, where the active period showed rapid periodontal destruction accompanying all sign of clinical inflammation and the quiescent period where the disease activity was minimal.
During the active period, a significant amount (typically greater than 2 mm) of periodontal attachment was lost at a specific site over a short period of time. It was also found that …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Complexities in the diagnosis of periodontal diseases
Although microbes are the primary etiology of periodontal diseases, but they are insufficient to cause disease by themselves alone. The microbiological investigations have shown that both, the disease-causing and non-disease causing bacteria are present both in healthy individuals as well as in periodontitis patients. The presence of specific putative microorganisms in plaque cannot be considered to establish a periodontal diagnosis. The individual host response is an equally important factor in the pathogenesis of periodontal diseases. Also, individuals are variably susceptible to tissue breakdown. The presence of some systemic conditions like diabetes mellitus and environmental factors such as stress/smoking act as risk factors for the development of periodontal diseases. All these factors constitute a complex situation where establishing a diagnosis becomes difficult.
Advances in periodontal diagnosis
The advances in periodontal diagnosis can be divided into the following categories,
Advances in the assessment of gingival inflammation.
Advances in the assessment of loss of periodontal attachment.
Advances in radiographic diagnosis.
Advances in microbiological analysis,
Bacterial culturing.
Microscopic identification,
Light microscopy.
Dark-field/phase contrast microscopy.
Fluorescence microscopy.
Chromatography.
Advances in immunodiagnostic techniques,
Immunofluorescence assays.
Radio-immunoassay (RIA).
Enzyme-linked immunosorbent assay (ELISA)
Flow cytometry.
Latex agglutination assays.
Advances in assays based on molecular biology techniques,
Nucleic acid hybridization.
Nucleic acid amplification.
Nucleic acid sequencing.
Enzymatic digestion of nucleic acids.
Advances in identifying biomarkers for periodontal disease activity,
Subgingival bacteria and their products.
Inflammatory and immune products.
Proteolytic and hydrolytic enzymes released from inflammatory cells.
Enzymes released from dead cells.
Connective tissue degradation products.
Advances in genetic testing.
Advances in the assessment of gingival inflammation
The clinical signs of inflammation include calor, dolor, rubor, and tumor, which mean heat, pain, redness, and swelling, respectively. In inflamed gingiva, these signs can be seen easily. Healthy gingiva is pink with scalloped contour, firm and resilient consistency and knife-edge margins. In inflammation, the gingiva becomes edematous with the loss of knife-edge margins with clinically distinguishable redness. Bleeding on probing is one of the initial signs of gingival inflammation. In inflammation, the calor or heat has been used as a diagnostic marker to assess periodontal status. Haffajee et al. (1992) 4 used a periodontal temperature probe (Periotemp, ABIODENT, Inc, Danvers, MA, USA) to assess subgingival temperature. This probe …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Studies have demonstrated an increase in subgingival temperature in inflamed sites. Haffajee et al. (1992) 4, demonstrated that sites with a red (higher) temperature indication had more than twice the risk for future attachment loss than did those with a green indication. It was also seen that areas with increased temperature had elevated proportions of major putative pathogens, including Prevotella intermedia, Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Tannerella forsythia and Peptostreptococcus micros. However, it was not clear that whether the presence of these microorganisms was responsible for higher temperature by causing inflammation or the presence of inflammation facilitated their growth in these areas.
Advances in the assessment of loss of periodontal attachment
Periodontitis is characterized by the apical migration of junctional epithelial attachment. This loss of attachment can be clinically visible in the form of recession or in the form of true pocket formation. The periodontal attachment loss does not indicate the presence of active periodontal disease. Periodontium may be normal in the presence of significant attachment loss. A treated periodontal case may show attachment loss, but healthy periodontium.
The clinical attachment loss (CAL) is measured as the distance between the cementoenamel junction (CEJ) and the base of the sulcus/pocket. The depth of a healthy gingival sulcus ranges from 1 to 3 mm. In the case of recession, the CAL is measured by adding the sulcus/pocket depth and distance between the CEJ and gingival margin. In the case of true periodontal pocket, the CAL is measured from the CEJ and the base of the pocket. When the gingival margin is located coronal to the CEJ, CAL is measured by subtracting the distance from the free gingival margin to the CEJ from the pocket depth.
The conventional periodontal probes have been used to calculate the attachment loss, but may not give accurate results. Measurement of accurate CAL may be challenging, especially in research than in everyday clinical practice. It has been shown that while probing healthy gingival tissues, the periodontal probe generally stops coronal to the apical extent of the junctional epithelium, which is at the CEJ 5. But during gingival inflammation, there is less resistance to probe penetration and the periodontal probe generally passes apical to the level of the connective tissue attachment 6, 7. This results in an overestimation of pocket depth in the inflamed gingival sites and underestimation of pocket depth in the non-inflammed gingival sites. Also, many other factors …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
First-generation periodontal probes: The conventional or manual probes.
Second-generation periodontal probes: Pressure sensitive probes.
Third-generation periodontal probes: Pressure sensitive probes with computer capturing of data.
Fourth-generation periodontal probes: Periodontal probes utilizing 3D technology.
Fifth-generation periodontal probes: Periodontal probes utilizing 3D technology and ultrasound.
The detailed description of these generations of the probes has been given in, “Periodontal instruments”.
Advances in radiographic diagnosis
Digital radiography:
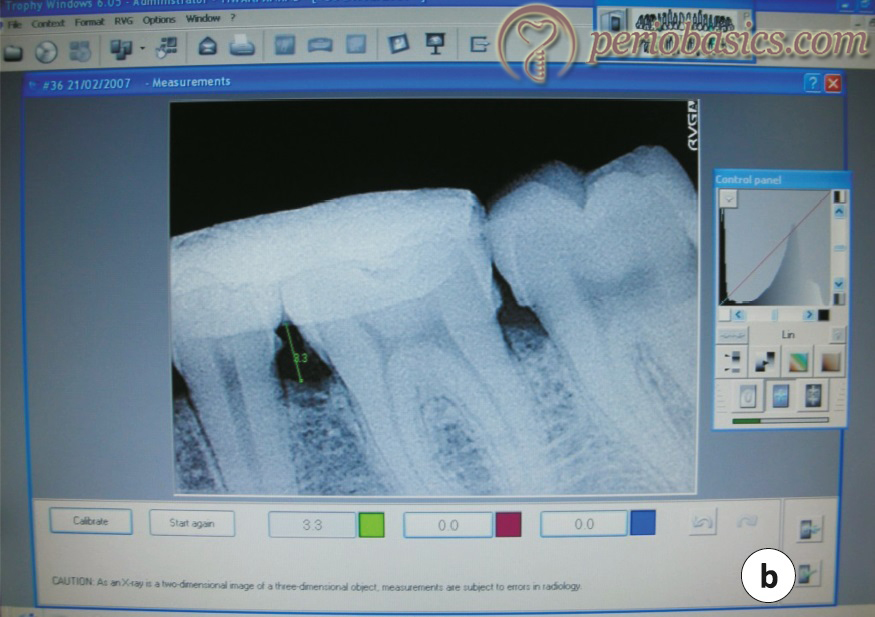
X-rays were discovered W C Rontgen in 1895 for which he was awarded the Nobel Prize in 1901. Almost a century later, the first digital dental radiographic image was produced with the introduction of RVG (Radiographic Imaging System) by Trophy in 1987. In 1991, Gendex Dental Systems introduced their new direct digital system, Visualix (VIXA in North America in 1993) in which radiation dose requirements were about 6 times less than D speed film. Today there are many companies providing digital radiography technology to practitioners. The advantage of digital images is that they can be manipulated on the computer screen to aid in the diagnosis by changing density, contrast, and magnification.
Physical principles of digital radiography:
In the conventional film-based radiography, the film serves as both detector and storage medium, whereas digital detectors are used only to generate the digital image, which is then stored on a digital medium. Digital imaging comprises four separate steps: generation, processing, archiving, and presentation of the image. Standard X-ray tube generates X-rays, which are then exposed to the sensor placed in the oral cavity. The energy absorbed by the detector is then transformed into electrical charges, which are then recorded, digitized, and quantified into a gray scale that represents the amount of X-ray energy deposited at each digitization locus in the resultant digital image.
The software then processes the information provided by the sensor and converts the raw data into a clinically meaningful image. The final digital image is stored in a digitized storage archive which contains the demographic information of the patient. While image viewing, the software provides us the freedom to manipulate the image such as panning, zooming, inverting the gray scale and in measuring distance and angle.
We have two kinds of digital radiography technologies: direct and indirect. The “Direct Digital Radiographic Technology” converts X-rays into electrical charges by means of a direct readout process. The “Indirect Digital Radiographic Technology” uses storage-phosphor image plates with a separate image readout process.
Direct digital radiography technology:
This technology uses an X-ray generator and a solid-state image receptor, more commonly referred to as a sensor. A sensor is made up of a silicon chip (with an electronic circuit on it) which is sensitive to light and has a scintillator layer that converts X-rays to light. The quality of an image produced by a solid-state detector is dependent not only on the chip pixel dimensions, but also on the type and configuration of the scintillator layer, the electronics including an analog to digital conversion, and the acquisition and display software.
There are two solid-state sensor technologies in the market today:
- CCD (charge-coupled device).
- CMOS (complementary metal-oxide semiconductor).
Following is the brief description of these solid-state sensors,
CCD (charge-coupled device):
A CCD chip is a metal oxide semiconductor (MOS) device. Its base is constructed of a material which is a good conductor under certain conditions. The base layer is topped with a layer of metal oxide. In the case of the CCD, usually silicon is used as the base material and silicon dioxide is used as the coating. The final, top layer is also made of silicon-polysilicon.
Essentially, a CCD chip consists of an array of small cells or pixels. Inside these cells are tiny photosensitive devices. These small devices are designed such that they will behave like “buckets” that will collect charge and hold it until it is drained out of the system (i.e., it is directly analogous to a capacitor). A pixel is the smallest component of an image. The individual CCD pixel size is approximately 40µ with the latest versions in the 20 µ range.
An image is derived from a CCD device in four steps …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
CMOS (complementary metal-oxide semiconductor):
Both, CMOS and CCD share common principles of physics but CMOS differs from CCD in terms of chip micro-architecture. In a CMOS chip, more of the electronic components controlling the conversion of photon energy into the electronic signal are incorporated into the chip itself. This simplifies the manufacturing process and, thus, reduces the costs of production. The quality of the image produced by CCD and CMOS systems is comparable.

Indirect digital radiography technology:
This technology uses image plates having a detective layer of photostimulable crystals that contain different halogenides such as bromide, chlorine, or iodine. The phosphor crystals are usually cast into plates and then into resin material in an unstructured way (unstructured scintillators). When X-rays are exposed on these photostimulable crystals, they absorb their energy by bringing their electrons to higher energy levels. These electrons may stay at a higher energy level for several hours depending on the specific physical properties of the phosphor crystals used.
The next step involves the scanning of the image plate with LASER beam. This converts the energy stored in the photostimulable crystals into light. An array of photomultipliers collects the light, which is converted into electrical charges by an analog-to-digital (A/D) converter. The digitally converted raw information in the form of electrical charges is now converted into a meaningful image by the software.
Advantages of digital radiography:
There are multiple advantages of digital radiography over conventional radiography. These are,
- Reduced exposure to X-radiation as compared to conventional films.
- A superior gray-scale resolution of 256 colors of gray in comparison to 16 to 25 shades of gray on a conventional film.
- Colorization and enlargement of the images can be done with digital images.
- Provides freedom of manipulation of contrast, sharpness, image orientation and pseudocolor alteration.
- Decreased processing time.
- Storage of radiographs into the small hard drive of the computer is a great space saver in comparison with an extra sheet of radiographs in each patient’s/client’s folder in the file shelves.
- Digital images can be easily transmitted to other dental offices.
- Digital radiography is environment-friendly because there are no disposal hazards of processing chemicals, silver salts in film emulsion and lead foil sheets.
- During implant placement, use of conventional films disrupt entire aseptic procedure and also time is wasted while the clinician awaits the development of the film several times during the procedure.

Subtraction radiography
Subtraction radiography was originally described by Ziedses des Plantes (1934) 9 in the 1930s. As the name indicates, subtraction radiography involves detection of areas of changes in bone density and/or volume on two serially obtained radiographs of a particular site, detected as lighter areas (bone gain) or darker areas (bone loss). Quantitative changes in comparison to baseline images can be detected using an algorithm for gray scale levels. This is accomplished by …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Limitations of subtraction radiography:
For successful subtraction radiography, reproducible exposure geometry, and also identical contrast and density of the serial radiographs, are essential prerequisites, and long experience shows that this technique is very sensitive to any physical noise occurring between the radiographs 11, 12. Such artifacts are often difficult to be distinguished from biologic changes 13; hence the projection geometry and contrast and density should be standardized. Any changes in contrast or intensity of the sequential images may provide inaccurate results. Density and contrast of radiographs are influenced by the processing time, temperature of the developer, and exhaustion of developer caused by aging and depletion. These factors have to be standardized to get accurate results.
Digital subtraction radiography (DSR)
Digital subtraction radiography (DSR) allows the detection of small changes in alveolar bone. Webber et al. (1982) 14 and Gröndahl et al. (1983) 15 introduced digital subtraction into dental radiography. The technique simply involves subtraction of pixels of one image from another with the same projection geometry where radiographs are taken at a specified time apart.
Obtaining identical images with similar projection geometry is difficult. Various published reports have used film holders connected to individual bite-blocks to obtain similar images of an area. Recently, some softwares have been developed which can reconstruct the second image according to the projection geometry of the first image. Images obtained by two different sensor systems can also be used with the help of these softwares 16.
As already stated, the baseline and sequential images should have similar exposure geometry, and also identical contrast and density of the serial radiographs. In DSR, this calibration can be accomplished by …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Computer Assisted Densitometric Image Analysis (CADIA)
Evaluation of the bone density is an important part of the treatment planning, especially during dental implant treatment. Bone quality and volume can be analyzed by various techniques such as intra-oral and panoramic radiographs, cone beam and micro-computed tomography (CBCT and CT), dual-energy X-ray absorptiometry (DEXA), magnetic resonance imaging (MRI), quantitative ultrasound and laser Doppler flowmetry. DEXA is considered as gold standard for analysis of bone density. It has been widely used for the analysis of bone density in osteoporosis. Because of the high cost of the equipment used, DEXA is usually not available in dental clinics.
The most widely used densitometric method in implantology is CADIA. CADIA is one form of subtraction radiography that allows the investigator to quantify the changes by comparing the radiographic density in a predetermined region of interest between baseline and follow-up radiographs 17. The equipment used in CADIA includes a video camera, which interfaced with an image processor, and a computer that allows the storage and mathematical manipulation of the images, measures the light transmitted through a radiograph, and converts the signals from the camera into gray-levels 10.
CADIA is capable of detecting minimal variations in the mineralized tissue density after various procedures such as after flap surgery, the healing process in the furcation area after regenerative procedures, and changes in bone density around implants over a period of time. In a study, Bragger et al. (1988) 18 compared the ability of CADIA to detect alveolar bone changes on radiographs with the interpretation of digital subtraction images and conventional radiographic interpre-tation in areas where osteoplasty or ostectomy was done. They found 72.7% negative change by digital subtraction images, 50.9% negative change by conventional interpretation, and 81.8% density change by CADIA. In another study where …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Computed tomography
The word ‘tomography’ comes from the Greek words: ‘tomos’ means slice and ‘graphein’ means ‘to write’. So, tomography literally means ‘writing slices’. It is the technique of reconstructing a cross-sectional image of the body from a ‘virtual pile of X-ray photographs’. In this scan, the patient remains stationary on the examination table while the X-ray tube rotates in a circular orbit around the patient in a plane perpendicular to the length-axis of the patient. A fan-shaped or cone-shaped X-ray beam passes through the body of the patient, which is received by the receptors on the opposite side of the X-ray source. The arrangement of the X-ray tube and the receptors have changed during the years with different technical solutions being named ‘generations’. Presently, we are using third- or fourth-generation CT-scans.
A detailed description of various forms of computed tomography scans is given in “Diagnostic imaging in implantology”.
Advances in the microbiological analysis
Bacterial etiology of periodontal diseases is well established. There is a complex microflora involved in the initiation and progression of periodontal diseases. Various types of periodontitis have been studied for the micro-organisms associated with their progression. Various organisms which have been shown to be strongly associated with periodontal destruction include Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola, and Aggregatibacter actinomycetemcomitans. The Gram-negative anaerobic rods have been shown to cause most periodontal damage. The black-pigmented, Gram-negative anaerobic rods Porphyromonas gingivalis and Tannerella forsythia have been implicated as major pathogens in the etiology of periodontal disease. These species are frequently isolated together 21, indicating an ecological relationship between them.
One investigation demonstrated a positive relationship between pocket depth and P. gingivalis and T. denticola counts and percentages. The cell numbers were significantly lower after initial periodontal treatment (which included scaling, tooth-brushing instruction, and professional mechanical tooth cleaning) as compared to that before the treatment 22. Socransky and Haffajee (1998) 23 showed that many bacterial species contribute to the development of periodontitis. They investigated over 13,000 subgingival plaque samples from 185 adult subjects and used DNA hybridization methodology and community ordination techniques to demonstrate the presence of specific microbial groups within dental plaque. Subgingival microbial complexes were made with the red complex containing most putative organisms (Bacteroides forsythus, Porphyromonas gingivalis and Treponema denticola).
The current data suggest that the presence or absence of certain bacteria cannot distinguish between chronic (Grade A/B) and aggressive (Grade C) periodontitis. In a systematic review, Mombelli et al. (2002) 24 found that the presence or absence of certain identified periodontal pathogens could not distinguish cases of chronic periodontitis from the cases of aggressive periodontitis.
So, the question remains; what is the etiology of periodontitis? The answer can be explained on the basis of host-microbial interactions. Although, the microbial etiology of …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Principles of microbial identification:
Various microorganisms can be identified based on their phenotypic or genotypic composition. The phenotypic criteria of bacterial identification are based on observable physical or metabolic characteristics of bacteria. Most of the phenotypic characterizations used in diagnostic bacteriology are based on tests that establish a bacterial isolate’s morphology and metabolic capabilities. The most commonly used phenotypic criteria include 26:
Microscopic morphology and staining characteristics.
Macroscopic (colony) morphology.
Environmental requirements for growth.
Resistance or susceptibility to antimicrobial agents.
Nutritional requirements and metabolic capabilities.
The genotypic identification methods involve characterization of some portion of a bacterium’s genome using molecular techniques for DNA or RNA analysis. The genotypic approach is highly specific and often very sensitive because it identifies the presence of a specific gene or a particular nucleic acid sequence which is specific for a particular microorganism.
Properties of an ideal diagnostic test:
An ideal diagnostic test should have the following features 27, 28,
- Highly specific,
- Highly sensitive,
- Reproducible,
- Quantitative,
- Simple to perform,
- Rapid,
- One-stage or a two-stage procedure,
- Non-invasive,
- Versatile in terms of sample handling, storage, and transport,
- Amenable to chairside use,
- Economical, and
- Dependent on simple and robust instrumentation.
Bacterial culturing
The most common bacterial identification method is conventional bacterial cultivation. It involves growing bacteria in either aerobic or anaerobic conditions on different media and performing tests to identify and quantify specific species. Bacterial culturing not only helps in bacterial identification, but also helps in determination of antibiotic susceptibility. In the identification of periodontal pathogens, there are multiple drawbacks associated with bacterial culturing. The culture methods are …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Microscopic identification
Since the introduction of the light microscope, many advances have taken place in microscopy. The light microscope has a limited capability in regards to the size of a particle that can be examined, whereas electron microscope provides additional resolution that allows for the examination of subcellular structures and even molecules.
Dark field microscopy:
Dark field microscopy works on the principle of creating a contrast between the object and the surrounding field, such that the background is dark and the object is bright. This procedure can be used to assess directly and rapidly the morphology and the motility of bacteria in a plaque sample. The main advantage of this technique is that it is an inexpensive means of smearing a microbial sample for major morphotypes.
However, there are some major drawbacks of this technique. The technique has an inability to identify certain species and to distinguish individual bacterial species. The major periodontal pathogens, including Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Tannerella forsythia, Eikenella corrodens and Eubacterium species are non-motile and therefore this technique is unable to identify these species. Other significant disadvantages of dark-field microscopy include the absence of species identification and the lack of guidance concerning the choice of an appropriate antibiotic 32. The dark-field characteristics of the subgingival microflora were systematically evaluated by Listgarten and Hellden (1978) 33. Several studies have investigated the relationship of dark-field morphotypes to the progression of periodontal diseases. Most of the studies could not establish any correlate between the presence of spirochetal and motile forms and periodontal disease progression in patients on maintenance who were entering into an active phase of disease 34, 35.
Phase-contrast microscopy:
The phase-contrast microscopy allows objects that differ slightly in refractive index or thickness to be distinguished from unstained or living cells. Differences in the thickness or refractive index of the specimen result in a differential retardation of light which shifts the phase. The main advantage of phase-contrast microscopy over dark field microscopy is that it is possible to visualize certain structures that are otherwise invisible. This includes certain cell organelles which cannot be seen well in the bright/dark field.
Fluorescence microscopy:
In fluorescence microscopy, a fluorochrome is excited by ultraviolet light, resulting in visible fluorescence. As a result, a bright image, in a dark background is seen. Fluorescence emission is always a longer wavelength (less energy) than the absorption (or excitation) which results in bright illumination of the specimen. It is used extensively to study the intracellular distribution, dynamics, and molecular mechanisms of a large variety of macromolecules and metabolites. This technique is commonly used to visualize the distribution of certain proteins in a cell or to make visible the specific organelles, filaments, and biochemically distinct membrane regions.
Chromatography
Various periodontal pathogens produce metabolites, including volatile compounds like volatile sulfur compounds. Bacteria like Treponema denticola, Porphyromonas gingivalis, Prevotella intermedia, and Tannerella forsythia are capable of reducing sulfates. They degrade serum proteins, cysteine, and methionine resulting in the production of measurable amounts of S, HS, H2S, and CH3SH. These resultant volatile sulfur compounds can be detected biochemically by chromatography 36, 37. Chromatography refers to the procedures used to separate and characterize substances based on their size, ionic charge, or their solubility in particular solvents. Chromatography involves two phases: the mobile phase and the stationary phase. The mobile phase (gas or liquid) contains and carries the sample to be analyzed through or across the stationary phase. The stationary phase maintains conditions necessary for separating various substances (i.e., the analytes) within the sample being studied. The name of the procedure specifies the mobile and the stationary phase, for example, gas-liquid chromatography refers to a chromatography method that uses gas as the mobile phase and liquid as the stationary phase.
The procedure involves mixing the sample with mobile phase, which carries the sample through a column containing the stationary phase. Depending on the nature of the solid phase, different analytes within the sample will be retained within the column based on the size, ionic charge; or analyte solubility in the mobile phase. As the mobile phase continues …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
High-performance liquid chromatography:
High-performance liquid chromatography (HPLC) is a type of liquid chromatography used to separate and quantify compounds that have been dissolved in solution. HPLC is accomplished by injection of a small amount of liquid sample into a moving stream of liquid (called the mobile phase) that passes through a column packed with particles of stationary phase. Different compounds are separated from each other as they move through the column. HPLC has multiple applications in research for the identification of various molecules and bacterial cell wall components, especially in the antibiotic-resistant bacteria.
Advances in immunodiagnostic techniques
Immunodiagnostics is a diagnostic methodology that uses an antigen-antibody reaction to detect target organisms. Various immunodiagnostic techniques including immunofluorescent (direct and indirect) assays, radioimmunoassays, enzyme-linked immunosorbent assay (ELISA), flow cytometry and latex agglutination tests, have been used widely to detect various target microorganisms. The radioimmunoassay and ELISA were the predominant techniques during the initial era of immunodiagnostics. Till date, ELISA has been the gold standard of clinical immunodiagnostics. Various immuno-diagnostic techniques employed in the field of periodontics are as follows,
Immunofluorescence assays:
This immunodiagnostic test utilizes fluorescent-labelled antibodies to detect specific target antigens. In this technique, antibodies are chemically conjugated to fluorescent dyes such as fluorescein isothiocyanate (FITC) or tetramethylrhodamine isothiocyanate (TRITC). These labeled antibodies bind (directly or indirectly) to the antigen of interest which allows for antigen detection through fluorescence techniques. The fluorescence can then be quantified using a flow cytometer, array scanner or automated imaging instrument, or visualized using fluorescence or confocal microscopy. There are two kinds of immunofluorescence assays: direct and indirect.
In the direct immunofluorescence, single antibody is used which is directed against the target of interest (known as a primary antibody). The antibody is directly conjugated to …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Radio-immunoassay (RIA):
RIA use antibodies to detect and quantitate the amount of antigen (analyte) in a sample. These assays are typically very sensitive and specific. RIA has been the first immunoassay technique developed to analyze nanomolar and picomolar concentrations of hormones in biological fluids. With this technique, any biological substance for which a specific antibody exists can be measured, even in minute concentrations. The procedure of RIA consists of adding suitable quantities of standard, unknown, radiolabelled antigen and antibodies to a buffer solution and allowing the reaction to reach equilibrium. For radiolabelling, Iodine125 labels are commonly used, although other isotopes such as C14 and H3 have also been used. Known amounts of unlabeled (“cold”) antigen are added to samples of the mixture. These compete for the binding sites of the antibodies. At the end of the incubation period, the free and bound fractions are separated using a suitable technique. The distribution of radioactivity in each sample is determined by counting either free or bound or both with the use of suitable counting equipment.
Enzyme-linked immunosorbent assay (ELISA):
ELISAs are plate-based immunoassays designed for detecting and quantifying substances such as peptides, proteins, antibodies, and hormones. In periodontology, ELISA has been primarily used to detect serum antibodies to periodontopathogens. This test is performed by first incubating a specific antigen in the wells of a plastic microtiter plate (96-well or 384-well polystyrene plate). The antigen binds to the surface of wells, the excess antigen is removed, and the sample suspected to contain antibodies against this antigen is applied to the antigen in the wells. After a wash to remove any unbound sample antibodies, a secondary antibody (an anti-antibody) specific to the antibody being investigated, is applied. This secondary antibody has been conjugated with an enzyme, such as horse-radish peroxidase, and after incubation and washing to remove any that is unbound, the enzyme’s substrate is added. The slightest amount of linked or sandwiched antibodies in the well will result in detectable amounts of color when the colorless substrate is cleaved to a colored product by the conjugated enzyme.
ELISAs can be performed with a number of modifications to the basic procedure. The key step in this test is the immobilization of the antigen, which can be achieved in different ways. It can be immobilized by direct adsorption to the assay plate or indirectly via a capture antibody that has been attached to the plate. The immobilized antigen can be identified either …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Flow cytometry:
The basic principle of flow cytometry is measuring physical and chemical characteristics of particles in a fluid stream as they pass through one or more lasers. The properties measured include particle’s relative size, relative granularity or internal complexity, and relative fluorescence intensity. The basic components of flow cytometry are fluidics, optics, and electronics. The fluidic system transports particles in a stream to the laser beam; the optical system illuminates the particles for detection of resultant light signals by optical filters and the electronics system converts the detected light signals into electronic signals that can be processed by the computer. Cells in suspension are made to react with a monoclonal cell surface constituent that is labeled with one or more fluorescent dyes such as fluorescein. After incubation, the cells are passed through a focused beam of laser. The cells scatter the light at low and wide angles, which is then measured.
Flow cytometry techniques have recently been applied for the identification of oral bacteria. However, many technical questions must be solved to determine the efficacy of this technique for the identification of specific bacteria in plaque.
Latex agglutination assays:
Latex agglutination tests are common immunological tests done in clinical laboratories. In latex agglutination procedures, an antibody (or antigen) coats the surface of latex particles (sensitized latex). When a sample containing the specific antigen (or antibody) is mixed with the milky-appearing sensitized latex, it causes visible agglutination. The degree of agglutination plotted as a function of agglutinant concentration follows a bell-shaped curve. The latex particles are used to magnify the antigen-antibody complex to make it visible. There are two types of latex agglutination assays: indirect assay and inhibition assay. The indirect assay is commonly used to detect various bacteria in plaque samples. Here, the antibody is bound to the latex particles and the suspension of the plaque sample is mixed with the sensitized latex. After gentle agitation for 3-5 minutes, agglutination or clumping is indicative of a positive result for the bacteria being tested. In an inhibition assay, a fixed quantity of antibody is mixed with a …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Immunoblotting (western blotting):
Immunoblotting is typically used to determine the amount (dot blot) and molecular weight (western blot) of an antigen present in a complex mixture. The technique uses antibodies (or other specific ligands in related techniques) to identify target proteins among a number of unrelated protein species. The process involves the separation of proteins by electrophoresis and then transferring them onto membranes (usually nitrocellulose). The membrane is overlaid with a primary antibody for a specific target and then with a secondary antibody labeled, for example, with enzymes or with radioisotopes. When the ligand is not an antibody, the reaction can be visualized using a ligand that is directly labeled. The western blot test involves three basic steps,
- Sample production by lysis or homogenization to solubilize and release cellular proteins.
- Separation of protein mixtures using gel electrophoresis.
- Transfer of separated proteins to a blotting membrane which can be manipulated more easily than a gel.
Advances in assays based on molecular biology techniques
The recent advances in microbiology are in the field of molecular analysis. Although the conventional methods are the mainstay of diagnostic bacteriology, notable limitations are associated with the use of phenotypic methods. These limitations are as follows:
Inability to grow certain fastidious pathogens.
- Inability to maintain the viability of certain pathogens in specimens during transport to the laboratory.
- Extensive delay in the cultivation and identification of slowly growing pathogens.
- Lack of reliable methods to identify certain micro-organisms grown in vitro.
- Use of considerable time and resources in the establishment.
Nucleic acid molecules like deoxyribonucleic acids (DNA), ribonucleic acids (RNA) are basic, essential and primary molecules for all molecular biology-related research. The molecular diagnostic tests can be broadly classified into following categories: hybridization, amplification, sequencing, and enzymatic digestion of nucleic acids.
Nucleic acid hybridization:
Hybridization methods are based on the ability of two nucleic acid strands that have complementary base sequences (i.e., are homologous) to a specifically make a bond with each other and form a double-stranded molecule, or duplex or hybrid. Hybridization assays require that one nucleic acid strand (the probe) originates from an organism of known identity and the other strand (the target) originates from the unknown organism to be detected or identified. Positive hybridization identifies the …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Checkerboard DNA-DNA hybridization:
Socransky et al. (1994) 45 developed this technique for the detection and levels of 40 bacterial species often found in the oral cavity. The technique is rapid, sensitive, and relatively inexpensive. The DNA Checkerboard method offers the ability to include more potential periodontal pathogens in large-scale studies with a single analysis which is usually not possible with cultural analysis. These new probe-target format permits to enumerate large numbers of species in very large numbers of samples. The method requires sophisticated laboratory equipment and expertise and is highly specific, and thus this assay has not been generalized for diagnostic purposes.
The technique includes the use of whole genomic DNA probes and allows the identification and the quantification of multiple microorganisms. Socransky et al. (1998) 23 described the presence of five, and subsequently six microbial groups within the subgingival biofilm. A group of species denominated the red complex consisted of three species: P. gingivalis, T. forsythia, and T. denticola.
Nucleic acid amplification:
Although hybridization methods are highly specific for organism detection and identification, but they may give false-negative results in case where an insufficient target nucleic acid is present in the reaction. Therefore, many hybridization methods require “amplifying” target nucleic acid by growing target organisms to greater numbers in culture. The three strategies for molecular amplification are target nucleic acid amplification, nucleic acid probe amplification, and amplification of the probe “signal”.
Target nucleic acid amplification:
For the amplification of target nucleic acid, polymerase chain reaction (PCR) technique is used which is based on the reiteration of a three-step process: denaturing double-stranded DNA into single strands, annealing primers (specific synthetic oligonucleotides) to the single-stranded DNA, and enzymatically extending the primers complementary to the single-stranded DNA templates. Taq polymerase is the enzyme commonly used for primer extension, which occurs at 72° C. This enzyme is used because of its ability to function efficiently at elevated temperatures and withstand the denaturing temperature of 94° C through several cycles. After the primers are annealed to the denatured DNA, the single-stranded DNA segment becomes the template for the extension reaction. By this method, a single copy of a nucleic acid target, often undetectable by standard hybridization methods, is multiplied to 107 or more copies within a relatively shorter period of time. The PCR amplification product containing the target nucleic acid of interest is referred to as the amplicon. Detection of the amplicon can be done by any of the basic detection methods, including radioactive, colorimetric, fluorometric, or chemiluminescent detection signaling. There are some shortcomings of the PCR. The system is susceptible to contamination with extraneous DNA fragments that could be amplified along with the sample.
Various derivatives of PCR procedure are available today. These include,
- Multiplex PCR,
- Nested PCR,
- Quantitative PCR,
- Reverse transcription PCR (RT-PCR),
- Arbitrary primed PCR, and
- Real-time PCR.
Multiplex PCR:
In this form of PCR, more than one primer pair is included in the PCR mixture. The advantage of this procedure is the establishment of an internal control in the PCR procedure. For example, in the detection of a particular bacteria, one primer pair can be directed at sequences present in all clinically relevant bacteria (i.e., the control or universal primers) and the second primer pair can be directed at a sequence specific for a particular gene of interest (i.e., the test primers). Thus, after completion of the PCR procedure, the control amplicon is always detectable. If not, the procedure was not performed accurately. Another advantage of this procedure is the simultaneous detection of multiple targets in a single PCR. The disadvantage of the multiplex-PCR procedure is that mixing different primers can cause some interference in the amplification process.
Nested PCR:
This PCR procedure involves the sequential use of two primer sets. The initial primer set is used to amplify a target sequence. The amplicon obtained is then used as the target sequence for a second amplification using primers internal to those of the first amplicon. Thus, these two step identification …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Quantitative PCR:
As the name indicates, this PCR procedure has the ability to quantitate the actual number of targets present originally in the clinical specimen. The procedure monitors the accumulation of a DNA product from a PCR reaction. The results of the procedure indicate the “infectious burden” in the original specimen which is clinically very helpful in establishing a diagnosis and identifying the prognosis of infectious conditions such as AIDS.
Reverse transcription PCR (RT-PCR):
The RT-PCR amplifies RNA targets. It is a very useful modification of the basic PCR procedure because many clinically important viruses have genomes composed of RNA rather than DNA (e.g., human immunodeficiency virus, hepatitis B virus). The unique step to this procedure is the use of the enzyme reverse transcriptase that directs the synthesis of DNA from the viral RNA template. Once the DNA has been produced, routine PCR technology is applied to obtain amplification.
Arbitrary primed PCR:
In this PCR procedure, short primers are used for amplification which is not specifically complementary to a particular sequence of a target DNA. These primers are usually composed of a short sequence (approximately 10 nucleotides) which anneal randomly to multiple sites in a chromosomal sequence. After completion of the reaction, multiple annealing sites result in the amplification of multiple fragments of different sizes. Theoretically, strains that have similar nucleotide sequences will have similar annealing sites and thus will produce amplified fragments (i.e., amplicons) of similar sizes. Therefore, by comparing fragment migration patterns following agarose gel electrophoresis, strains or isolates can be judged to be the same, similar, or unrelated.
Real-time PCR:
The real-time PCR is a recent modification to PCR. It allows precise quantification of specific nucleic acids in a complex mixture even if the starting amount of material is at a very low concentration. This is accomplished by rapid thermocycling and monitoring the amplification of a target sequence in real-time using fluorescent technology. It is capable of detecting the presence of a target within 30 to 120 minutes.
Nucleic acid sequencing:
The term DNA sequencing refers to the sequencing methods for determining the order of the nucleotide bases – adenine, guanine, cytosine, and thymine – in a molecule of DNA. Nucleotide order determines the amino acid order, and by extension of amino acid order, the protein structure and function (proteomics). By nucleotide sequencing, the exact nucleotide sequence of a …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Enzymatic digestion of nucleic acids:
Another molecular method for the identification of various microorganisms is the enzymatic digestion of nucleic acids and their subsequent electrophoresis. In this procedure, the whole genomic DNA is first purified from the bacteria. This DNA is then subjected to enzymatic degradation by using DNA endonucleases. The resultant DNA fragments are then subjected to electrophoresis. DNA fingerprinting is done by this procedure.
DNA fingerprinting:
The global population of different bacterial species consists of discrete clonal lines. There are genetic variations in between different clonal lines, but these species are not comprised of an infinite number of genetically different strains. The degree of genetic diversity is different for each bacterial species. With the help of enzyme restriction endonuclease, the bacterial chromosome can be cut in a unique set of DNA fragments. These unique DNA fragments of total genomic DNA from isolates of a selected species provides a useful method for “fingerprinting” individual stains. The procedure for DNA fingerprinting involves isolation and cultivation of a particular bacterial species in the liquid or solid medium. The bacterial cells are harvested from the culture, suspended in buffer, and lysed, usually with sodium dodecyl sulfate (SDS). Total genomic DNA is then purified by extraction. Restriction endonucleases are then used to produce the fingerprints of individual isolates because, for a specific bacterial clonal type this enzyme recognize and bind to a specific nucleotide sequence within double stranded DNA, and then cleave DNA at that point.
Advances in identifying biomarkers for periodontal disease activity
The conventional clinical and radiographical methods of periodontal diagnosis are important methods of diagnosing the periodontal diseases, but they are only capable of retrospective diagnosis of attachment and bone loss. These methods are not capable of identifying the current disease activity. A lot of research has been done to find out diagnostic tests which can detect the disease activity in periodontal diseases. The biomarkers which can be used as diagnostic markers in periodontal diseases can be either involved in some way in the disease process or released as a consequence of tissue damage during disease progression. The most important source of these biomarkers is gingival crevicular fluid (GCF).
GCF has been investigated for multiple periodontal disease biomarkers. For any GCF component to be regarded as a potential biomarker, its exact source, the precise nature and the role in disease process have to be established. The potential sources for these biomarkers can be derived from the following sources,
- Subgingival bacteria and their products.
- Inflammatory and immune products.
- Proteolytic and hydrolytic enzymes released from inflammatory cells.
- Enzymes released from dead cells.
- Connective tissue degradation products.
Subgingival bacteria and their products:
It has been well established that bacterial plaque is the primary etiology of periodontal diseases. But the subgingival flora is complex and may vary from patient to patient and site to site 46. Various periodontal pathogens have been suggested on the basis of animal and human pathogens responsible for periodontal destruction 23, 47. These include Porphyromonas gingivalis, Prevotella intermedia, Bacteroid forsythus, Aggregatibacter actinomycetemcomitans, Capnocytophaga ochracea, Eikenella corrodens, Campylobacter recta, Fusobacterium nucleatum and Treponema denticola.
As already discussed, these microorganisms can be identified by various methods, including dark field or phase contrast microscopy, culture techniques, immunological assays, DNA probe or enzyme-based assays.
Commercially available diagnostic kits for bacterial identification:
Evalusite (Kodak):
As already discussed in immunodiagnostic bacterial identification section, Evalusite is an ELISA-based diagnostic kit consisting of antibodies to detect antigens for P. gingivalis, P. intermedia, and A. actinomycetemcomitans.
Omnigene (OmniGene, Inc) and BTD (Biotechnica Diagnostics, Inc):
This is a DNA probe-based detection system for the identification of microbes. The plaque sample obtained from the patient is put in a transport medium and is sent to the company for assays. The bacterial detection DNA probes are available for A. actinomycetemcomitans, P. gingivalis, P. intermedia, E. corrodens, F. nucleatum, C. recta, T. denticola and T. pectinovorum.
Commercially available diagnostic kits for identification of bacterial products:
Certain bacterial products can be used as markers for their presence in plaque sample. Trypsin-like proteases are the bacterial products which can be used as markers for their identification. These are mainly produced by P. gingivalis but lesser amounts are also produced by B. forsythus and T. denticola. A commercially available diagnostic kit for identification of these enzymes is “Perioscan”.
Perioscan (Oral-B Laboratories):
This is a chairside diagnostic kit which uses the BANA (N-benzoyl-DL-arginine-2-naphthylamide) hydrolysis reaction for identifying bacterial trypsin-like proteases in plaque samples. In this hydrolysis reaction, BANA which is a substrate conjugated beta-naphthylamine is hydrolyzed by this trypsin-like enzyme to release free beta-naphthylamine. Free beta- naphthylamine is a chromophore which reacts with a variety of dyes (e.g. Fast-Garnet GBC) to produce colored products.
A subgingival plaque sample obtained from the patient is placed on the BANA-containing strip which is then folded to contact a second strip containing the “Fast Black” dye reagent. It is then placed in an oven for 15 min at 55°C. Identification of any blue-black color on the strip indicates the presence of trypsin-like proteases in the plaque sample. This test has advantages as well as disadvantages. In a study Loesche et al. (1992) 48 compared BANA test to other methods of microbial testing and found that …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Advantages:
- Results are available in a shorter period of time.
- The visual result can be shown to the patient related to the site from which they were obtained.
Disadvantages:
- The test may be positive at clinically healthy sites and might remain so after treatment.
- The test detects the presence of P.gingivalis, B. forsythus, and T. denticola but it has relatively poor predictive abilities for periodontal disease activity.
- It is not possible to sample all the sites in the mouth with this test (as with other chair-side diagnostic test systems) and therefore the site(s) to be tested have to be preselected.
Perio 2000:
As already discussed in chromatography section, Perio 2000 system has been designed to display the sulfide level digitally.
Toxicity Prescreening Assay (TOPAS):
is a chairside test kit for indirectly detecting bacterial toxins and bacterial proteins which are one of the markers for the presence of gingival infection. This test detects the indirect presence of bacteria by two markers of gingival infection: bacterial toxins and bacterial proteins. This test is an indirect indicator of metabolic activity within the actively dividing bacteria. This test can be used to know the difference between an active and an inactive periodontal disease as indicated by the change in the color intensity scale of the test based on the fact that metabolic activity increases as the concentrations of these toxins increases.
Inflammatory and immune products
The subgingival plaque initiates an inflammatory reaction in the gingival sulcus. This inflammation along with the direct effect of bacteria causes most of the tissue destruction 49, 50. Various inflammatory cells such as PMN’s, macrophages, monocytes etc. secrete their products which intensify the inflammatory response. The levels of inflammatory cytokines (ie, interleukin(IL)-6) and general markers of inflammation (i.e., C-reactive protein) have been shown to be elevated in the blood of patients with periodontitis 51. Most of the substances which are released from inflammatory and immune cells in periodontal connective tissues pass into the GCF. GCF is easy to sample and therefore these substances are easily available for analysis. The substances released by inflammatory and immune cells during the disease process include antibodies, complement proteins, inflammatory mediators such as prostaglandins (PG), pro-inflammatory cytokines such as various IL and tumor necrosis factor (TNF) and enzymes such as β-glucuronidase and elastase. These mediators have also been found to be elevated in the saliva of patients with periodontitis 52.
Various products of inflammatory response:
Cytokines:
Cytokines are cell to cell messengers or local hormones, which modulate the function of a wide variety of cells. They are involved in regulating the immune and inflammatory response. Although a large number of cytokines have been studied to associate them with periodontal breakdown, however; most investigated among them are IL-1β and TNF-α. These cytokines are produced by activated macrophages and other cells and have pro-inflammatory effects of relevance to periodontal pathology 53, 54. As these pro-inflammatory cytokines are present in the inflamed gingiva, their substantial levels can be found in GCF. Their concentration in healthy sites is low as compared to the diseased site which makes them a good candidate for the identification of disease activity in the periodontal pocket. The pro-inflammatory effect of IL-1β and TNF-α include stimulation of endothelial cells to express selectins that facilitate the recruitment of leukocytes, activation of macrophage IL-1 production, and induction of PGE2 by macrophages and gingival fibroblasts.
GCF levels of IL-1 β have been found to be consistently …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Prostaglandins:
PGE2, the metabolite of the cyclooxygenase pathway, is one of the most potent mediators of alveolar bone loss in periodontitis 56. It acts as one of the key mediators in the periodontal inflammation by stimulating the suppression of lymphocyte production, decreasing the collagen synthesis by fibroblasts and influencing osteoclastic bone resorption 57-59. PGE2 levels are low in health and nondetectable at many such sites. In naturally occurring gingivitis, there is a modest rise in GCF PGE2 levels to between 32 and 53 ng/ml. Whereas, untreated periodontitis patients have its significantly higher levels than gingivitis patients 60. Because PGE2 levels have been found to correlate with the periodontal status, a clinical diagnostic kit based on ELISA can be designed to estimate its level in the GCF. However, presently no commercial chairside diagnostic kit is available for PGE2 level estimation.
Proteolytic and hydrolytic enzymes released from inflammatory cells:
The inflammatory and immune cells, such as polymorphonuclear neutrophil leukocytes (PMNs), macrophages, lymphocytes and mast cells secrete various proteolytic and hydrolytic enzymes which not only degrade the phagocytosed material but are also responsible for connective tissue destruction. These can be cysteine proteinases, serine proteinases or matrix metalloproteinases (MMPs). These enzymes may be released by inflammatory cells during their function or when they degenerate or die. The main components of connective tissue are collagens and proteoglycans. Collagens have a …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book ……..
The degradation of collagen is usually followed by a breakdown of the proteoglycans. Proteoglycans consist of a glycosaminoglycan (GAG) molecule linked to a protein core 61. The principal proteoglycans present in the gingiva and periodontal ligament are hyaluronic acid, heparin sulfate, dermatan sulfate and chondroitin sulfate-4. Inflammatory cells secrete multiple proteolytic and hydrolytic enzymes which are,
- Proteolytic enzymes: Collagenase, elastase, cathepsin G, cathepsin B, cathepsin D, dipeptidyl peptidases, tryptase.
- Hydrolytic enzymes: Arylsulfatase, β-glucuronidase, alkaline phosphatase, acid phosphatase, myeloperoxidase, lysozyme, lactoferrin.
These enzymes can be easily detected in GCF which makes them suitable candidates for diagnostic kits.
Commercial chairside diagnostic kits for detection of proteolytic and hydrolytic enzymes:
Perio-Check:
This system detects the presence of neutral proteases such as collagenase in GCF. It measures neutral protease activity within GCF. GCF is obtained in a paper strip which is placed on a gel containing insoluble dye-labelled collagen fibrils (remazol brilliant blue-collagen substrate powder) and incubated at 43°C. If neutral proteases are present in GCF, they diffuse in the gel and the insoluble collagen-dye complex is digested to release soluble dye labelled fragments, which diffuse back into the strip, turning it blue. The intensity and the area of the blue color are then scored on a scale of 0 to 2 by comparing it with three standards on a color card which is provided with the test kit. The intensity of the color is proportional to the amount of enzyme present in the sample.
Prognos-Stik (Dentsply):
This kit is designed for the detection of serine proteinase, elastase in GCF samples. A GCF sample is collected on special paper strips which have been impregnated with the appropriate peptidyl derivative of 7-amino-trifluoromethyl coumarin (AFC). If elastase is present …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Enzymes released from dead cells:
During the inflammatory process, there is damage to the epithelial cells of the pocket lining and connective tissue. Also, inflammatory cells such as PMN’s densely populate the inflamed periodontal connective tissues which also degenerate with time. They live only for 7-10 days before degenerating. With degeneration, these cells pour their cytosolic enzymes in the surrounding tissue. During its passage through the inflamed tissue, GCF picks up these enzymes released during the destructive process. Two of these enzymes have been widely used in medicine for several decades as diagnostic aids to assess cell death and tissue destruction. These are aspartate aminotransferase (AST) and lactate dehydrogenase (LDH). These are soluble cytoplasmic enzymes present in the cell, but due to cell death, they are released into the surrounding tissue. Because cell death is an integral and essential component of periodontal tissue destruction, the level of these enzymes in the GCF or saliva is a good indicator of cell death in periodontal tissue. Chambers et al. (1991) 62 reported that elevated levels of AST were associated with a 9 to 16 times greater risk of experiencing active periodontal tissue destruction. The GCF/saliva levels of these enzymes can be used as a potential biomarker for the disease activity in periodontal pockets.
Commercial chairside diagnostic kits for detection of LDH and AST enzymes:
PerioGard:
This is a commercial diagnostic kit for the detection of AST levels in GCF. The test involves the collection of GCF with the filter paper strip which is then placed in tromethamine hydrochloride buffer. At the same time positive and negative control wells are prepared using strips provided. Two drops of a solution provided (260mM L-aspartic acid, 33 mM 2-oxogluteric acid, 4.3 mM disodium EDTA, 1.6% polyvinylpyrrolidone, 0.067% Triton X-100, 2.7 mM sorbic acid in 100 MM Tris-HCI, pH 6.0) are added to the wells and allowed to incubate at room temperature. After 9 minutes of incubation, the substrate/ detection solution (1 mg fast red RC diazotised salt in 1% methanol, 0.067% Triton X-100, in 230mM Tris-HCI, pH 8.0) is mixed and two drops are added at 10 minutes. After 5 minutes, test results can be read by eye by comparing the test well color to the color of the positive control. A color of greater intensity to that of the negative control is scored as positive and one of lesser or equal intensity as a negative result. The test is designed to be positive at ≥ 800 mIU, AST activity and negative at values <800 mIU.
Pocket watch:
This chairside diagnostic kit has been designed for the detection of levels of AST in GCF. The biochemical principle behind this test is that AST catalyzes the transfer of an amino group of cysteine sulfuric acid by α- keto- glutaric acid to yield β-sulfinyl pyruvate in the presence of pyridoxal phosphate. Glutamate β-sulfinyl pyruvate spontaneously and rapidly decomposes and releases inorganic sulfite. The sulfite ions, thus produced react with malachite green because of which the dye loses its color. As soon as malachite green …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Connective tissue degradation products:
During the inflammatory process in the periodontal pocket, there is degradation of both soft and hard connective tissue. Various soft connective tissue degradation products are collagens (I, II, V), proteoglycans, hyaluronan, fibronectin, collagen Type IV, laminin, and glycosaminoglycans. There are proteins which can indicate bone resorption including osteonectin, bone phosphoprotein (N-propeptide), osteocalcin, and telopeptides of collagen Type I (ICTP). The biochemical techniques used to isolate and detect these components may be difficult to modify for chairside use. Presently, we do not have any chairside diagnostic kits for the detection of these molecules which can be used to assess the connective tissue breakdown in a periodontal pocket.
Advances in genetic testing
It is very well known now that periodontal diseases have a multifactorial etiology. Genetic susceptibility is an important factor contributing to the development and progression of periodontitis. Various genetic syndromes have Grade C periodontitis as one of their components. For example, palmoplantar dyskeratosis (Papillon-Lefevre syndrome) which is due to a defective gene on chromosome 11, because of which there is defective cathepsin C activity, is associated with rapid periodontal destruction. Various polymorphisms such as IL-1β polymorphism or TNF-α polymorphism are also associated with periodontal disease progression. Presently, studies focused on IL-1 gene polymorphism have lead to the development of the periodontitis susceptibility trait test 63, 64.
The genetic basis of periodontitis has been well investigated. It has been demonstrated that single gene polymorphisms (SNPs) may significantly affect the progression of the disease. In 1997, Kornman et al. 67 found an association between the polymorphism in the genes encoding for interleukin-1α and interleukin-1β and increased severity of periodontitis.
PST® genetic susceptibility test:
The Periodontal susceptibility test (PST®) genetic risk test, originally introduced to dentistry in 1997, was the first genetic test to identify an individual’s risk for developing periodontal disease. The test analyses two interleukins (IL-1α and IL-1β) genes for variations. It should be noted here that variation IL-1 gene may not initiate or cause disease but may lead to earlier or more severe disease.
PerioPredict:
Interleukin Genetics, Inc. introduced PerioPredict™ in 2013 which is the next-generation version of the PST® genetic risk test for periodontal disease. Like the original PST® test, PerioPredict™ measures variations in the genes for Interleukin-1 (IL-1), a key mediator of inflammation, and identifies individuals who are at an increased risk for more severe periodontitis. The kit includes an improvised sample collection technique that consists of easy-to-use cheek swab. The new test also utilizes an expansion of previous genetic markers that now cover all major ethnic groups including Hispanic, African-American, and Asian, in addition to Caucasian.
Recent advances in chairside diagnostic tests
Oral fluid nanosensor test (OFNASET):
OFNASET is used for the detection of salivary biomarkers for oral cancer. The test has been developed by the University of California, Los Angeles (UCLA) Collaborative Oral Fluid Diagnostic Research Laboratory, led by Dr. David Wong 68, 69. It is a microelectro-mechanical system based on electrochemical detection platform. The test is capable of real-time, ultra-specific multiplex detection of salivary protein, and RNA biomarkers. The test is highly sensitive. It analyzes saliva for …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Electronic taste chips:
A team of scientists at the University of Texas at Austin has recently developed a new sensor technology that allows for the simultaneous identification of multiple analytes (acids, bases, electrolytes, and proteins) in solution phase. The system consists of a number of different sensor types attached to the arm, a sample table, an amplifier, and a computer for data recording. The microchip consists of microspheres which are located on the inverted pyramidal microchambers of the microchip. On the interior regions of the microspheres, the sensor array platform is placed where all the chemical and immunological reactions are performed. This system imitates what is happening when molecules with specific taste nature interact with taste buds on the human tongue. The sensors act as taste buds and they send the information obtained to the computer where they are analyzed. A Charge-Coupled Device (CCD) video chip visualizes and captures the various optical signals generated by the reactions on the microspheres. This system can differentiate between healthy and periodontally diseased individuals based on the CRP levels.
OraQuick:
It is a test developed for quick detection of HIV infection. It provides results in 20 minutes. The fluid to be diagnosed is mixed in a vial with developing solution and the results are displayed on a testing device. This test is the first FDA-approved oral swab in-home test for HIV-1 and HIV-2 detection.
Integrated microfluidic platform for oral diagnostics (IMPOD):
It is a portable microfluidic device for detection of potential biomarkers of periodontal disease in saliva. The device performs rapid microfluidic chip-based immunoassays (<3–10 min) with low sample volume requirements (10 µL) and appreciable sensitivity (nM-pM). The device facilitates hands-free saliva analysis by …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
When to use chairside diagnostic tests?
A very relevant question is, when these chairside diagnostic tests should be used? The most logical answer to this question is before starting the periodontal therapy. By doing this we can get the baseline values of destructive activity going on in the periodontal pocket, which can afterwards be compared with post-treatment values.
Advantages and disadvantages of chairside diagnostic kits
There are many advantages of chairside diagnostic kits over the conventional diagnostic procedures which make them beneficial in clinical practice, however; they have some limitations also. Following are the advantages and disadvantages of these diagnostic kits,
Advantages:
- The markers which have been selected as indicators of periodontal disease activity have been found to be increased in GCF and saliva in longitudinal studies. Hence, they can predict the disease activity in the periodontal pocket.
- Simple to use, particularly the color detection systems.
- Can be read after a short time.
- Can be used to educate the patient about the condition of the disease.
Disadvantages:
- As research has shown that the periodontal disease may be in an active or inactive state in the patient and also at different sites in a patient’s mouth. So, which site should be analyzed for the prediction of disease activity? Also, if a particular site is chosen, will it give us the exact idea about disease activity?
- The choice of the most appropriate biomarker may still be difficult at present because no biomarker has been proven to be an exact indicator of disease activity.
- If a moiety is associated with inflammation this may mask its association with destructive disease.
- No account of biological control mechanisms is taken in present tests.
- These test kits are costly as compared to the conventional diagnostic techniques.
Conclusion
An accurate diagnosis of the disease is the primary requirement for a successful treatment. With the advancements in the diagnostic procedures, our accuracy in making a diagnosis has improved. The advances in radiographic techniques have enabled us to accurately access the periodontal bone morphology and long-term changes in the bony architecture following periodontal treatment. Various chairside diagnostic kits help us in identifying various bacterial and host-derived products in the periodontal pocket, thus helping us in the determination of microbiological and immunological activity going on in the periodontal pocket. These advances in diagnostic procedures have further improved our treatment planning, helping us to achieve better results following periodontal treatment.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

