Introduction
There have been a lot of changes in periodontal surgical techniques in the last few decades. One of the most important of these was the introduction of minimally invasive periodontal surgical techniques. Broadly, these techniques involve access and visualization of only those areas that require periodontal treatment using the smallest incision possible. The development of novel surgical techniques has led to the development and introduction of new instruments and materials which have been specifically designed to perform these procedures. With their multiple advantages, these techniques have become more and more popular with time. In the present chapter, we shall discuss in detail various aspects of minimally invasive periodontal surgical techniques.
Historical aspect
In medicine, the term “minimally invasive surgery (MIS)” was first coined by general surgeons Fitzpatrick and Wickham in 1990. They defined MIS as the ability to perform a traditional surgical procedure and achieve the same or better outcomes utilizing a surgical opening that was smaller than traditional surgical access. This small surgical incision results in less postoperative discomfort, more rapid healing, less morbidity, and equal or improved long-term surgical outcomes. MIS was first introduced in periodontology literature by Harrel and Rees in 1995 1. The primary aim of the proposed procedure was to minimize tissue trauma due to reflection and manipulation that resulted in better stabilization of the blood clot with reduced surgical morbidity. The procedure is usually performed by magnifying instruments, such as operating microscopes and microsurgical instruments and materials.
Cortellini and Tonetti in 2007 2 introduced a minimally invasive surgical technique (MIST) utilizing the flap design used in the modified papilla preservation technique (MPPT) or simplified papilla preservation technique (SPPT). It is a high-power magnification-assisted surgical technique that provides greater wound stability. The technique significantly reduced patient morbidity. This technique is a combination of minimally invasive surgery and papilla preservation techniques. A detailed description of the modified papilla preservation technique and simplified papilla preservation technique have been given in chapter 62 “Periodontal flap surgeries: current concepts”.
Objectives of MIST:
The primary objectives of MIST include,
- Reduction of surgical trauma.
- Increased flap/wound stability.Stable primary closure of the wound.
- Reduced surgical chair time.
- Minimized patient discomfort and side effects.
Features of minimally invasive periodontal surgery
As the name “minimally invasive” suggests, the techniques used to perform minimally invasive periodontal surgeries involve specific features. These include the following,
Incisions:
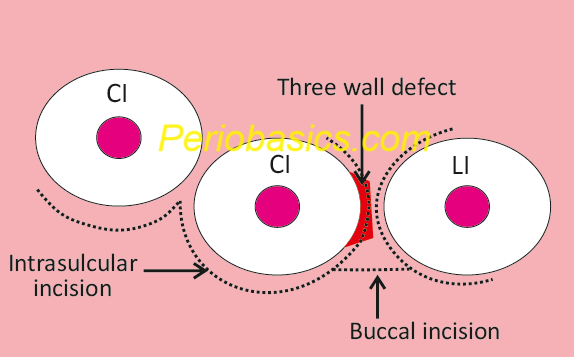
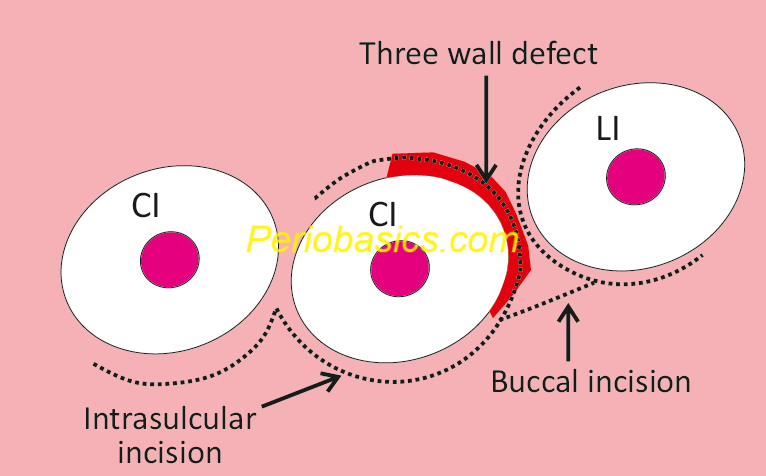
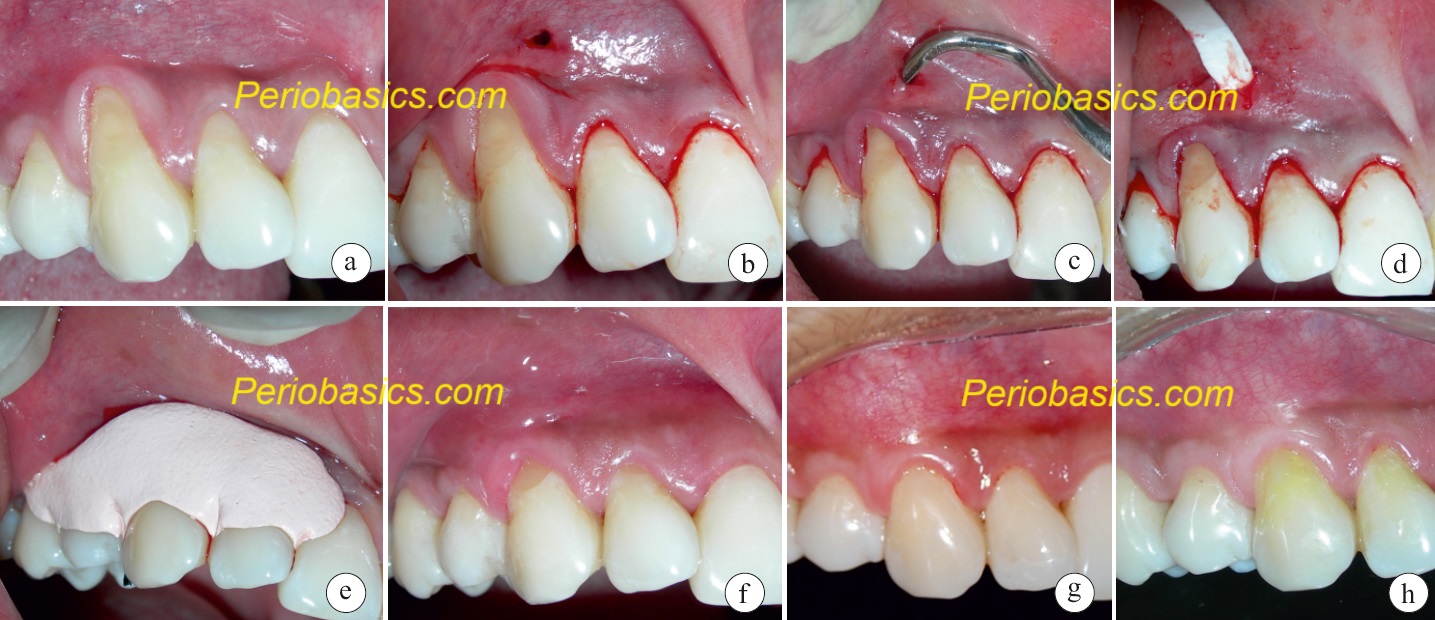
The incisions performed in these surgeries are designed to conserve as much of the soft tissue as possible. The incisions are placed as described in modified papilla preservation and simplified papilla preservation technique described by Cortellini et al. (1995, 1999) 3, 4. Let’s take an example of a localized interproximal defect on the distal root surface of the maxillary central incisor (Figure 77.1). Intrasulcular incisions are made on the teeth adjacent to the defect. As compared to most of the other surgical procedures, the incisions should be made as separate incisions and should not be continuous across the interproximal tissue. By doing so, most of the ……………Content available in book……..……Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book……… This technique allows us to preserve the shape of the papilla as well as cover the grafted site with soft tissue. Similar incision principles are used for the treatment of single gingival recession using the “Tunnel technique”. The only difference is that after placing the intrasulcular incision, instead of connecting them with a horizontal incision, a tunnel is prepared in the supra-periosteal tissue. This technique is based on the original “Envelope Technique” developed by Raetzke in 1985 5 for the treatment of single gingival recessions. After the preparation of the tunnel, a subepithelial connective tissue graft is placed and stabilized with the help of micro-sutures.
Flap elevation:
To minimize tissue damage, the flap should be elevated utilizing sharp dissection. Microsurgical blades or custom designed Orban knives can be used for this purpose. The advantage of using the Orban’s knife is that this can be inserted into previously made intrasulcular incision. During recession coverage, the tip of the knife can then be angled toward the center of the papilla, performing a thinning and placing the undermining incision. The sharp dissection preserves the blood supply to the tissue and aids in quick healing. In periodontal microsurgeries, it is always recommended that the periosteum should be left intact over the bone to prevent bone resorption. Further, it also facilitates tension-free flap closure.
Papilla preservation:
The papilla preservation techniques are a very efficient way to preserve the interdental tissue height. As already stated, both modified papilla preservation and simplified papilla preservation techniques can be utilized for this purpose. The papilla preservation technique was described by Takei et al. (1985) 6 ………….Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book………
Microsurgical instruments:
These instruments are mandatory for performing periodontal microsurgery. The microsurgical instruments are usually made slightly top-heavy and circular in cross-section to facilitate their manipulation. Shorter instruments with a rectangular cross-sectional design do not allow precise manipulation and are not ideal for microsurgery. The weight of these instruments is usually around 15-20 g to avoid the fatigue of hand and arm muscles 7. Small needles such as a spatula needle, which is 6.6 mm in length and has a curvature of 140 degrees, can be used for suturing. Designed for ophthalmic surgery, the needle track is shallow and the needle purchase point is precise.
In periodontal micro-surgical procedures, ………….Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book……… usually made from stainless steel and titanium. The titaniummade instruments are stronger, lighter, and non-magnetized in comparison to stainless steel instruments but are expensive and get readily distorted if not properly used. The most commonly used microsurgical instruments include,
- Micro raspatorium,
- Bone scraper,
- Microsurgical papilla elevator,
- Microscalpel holder,
- Needle holder,
- Micro scissors, and
- Dental microforceps.
Suturing technique:
The three primary goals to be achieved during microsurgical suturing are eliminating dead space, closing with sufficient but appropriate tension, and immobilizing the wound. As compared to conventional surgeries, the principles of suturing during microsurgery have little variations. The needle should penetrate perpendicular to the tissues and exit at equal distances; however, the suture bite size should be approximately 1.5 times the tissue thickness to achieve proper wound approximation 8. For tying the knot, the microsurgical needle holder should be held in the dominant hand, and a microsurgical tissue pickup in the nondominant hand. A very good knot strength can be achieved by placing a surgeon’s knot followed by a square knot. Adding excess ties to a knot increases its bulk rather than an increase in its strength or integrity 9.
Use of microscope:
Apotheker and Jako first introduced a commercial operating microscope to dentistry in 1981 10. As already stated in “Periodontal microsurgery” article, there are multiple magnification systems available for performing periodontal microsurgical procedures. These systems include three types of magnification loupes and the operating microscope. Both types of optical magnification have advantages and limitations. While using the loupes the defect can be visualized from various angles whereas while using the microscope, the defect can be visualized from only one angle as the microscope is fixed and cannot be moved. Hence, the type of ………….Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book………
Surgical approach in MIST
MIST in regenerative therapy:
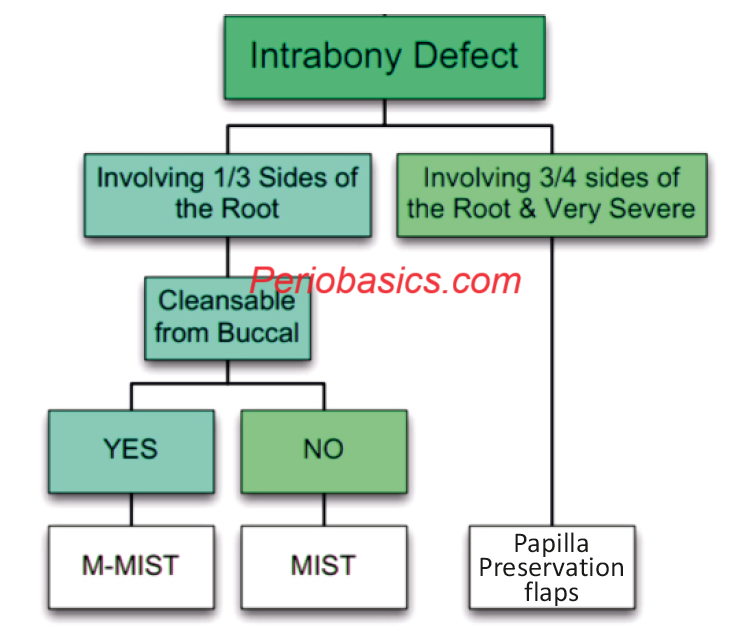
This minimally invasive surgical technique was described by Cortellini and Tonetti (2007) 2. The MIST is used in regenerative therapy in isolated defects located along single surface of the tooth. The defect is approached with modified papilla preservation technique (MPPT) or simplified papilla preservation technique (SPPT). MPPT is used when the interdental space is wider than 2 mm, while SPPF is used when the width of the interdental space is 2 mm or narrower. As described in the surgical procedures in case of MPPT and SPPT, strictly intrasulcular incisions are used to preserve all the height and width of the gingiva. Along with this, the mesiodistal dimensions of the flap are kept as minimum as possible. Full thickness flap is elevated to expose around 1-2 mm of the alveolar bone crest. When possible, only the defectassociated papilla is accessed, and vertical-releasing incisions are avoided. An isolated three-wall defect is an ideal candidate for this procedure. Sometimes, the three-wall defect may have buccal or lingual/palatal extension. In such cases, ………….Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book………
Modified minimally invasive surgical technique (M-MIST):
The modified minimally invasive surgical technique (M-MIST) was proposed by Cortellini and Tonetti (2009) 11. The three primary goals of this new technique were to minimize the interdental tissue tendency to collapse, to enhance wound/soft tissue stability, and to reduce patient morbidity. This procedure is also performed in areas with localized bone defects. The procedure involves the placement of intrasulcular incisions extended to the buccal aspect of the two teeth adjacent to the defect. The defect-associated interdental papilla is elevated following the incision design described for the simplified papilla preservation flap (when the width of the interdental space is 2 mm or narrower) or the modified papilla preservation technique (when the interdental site is wider than 2 mm). The mesiodistal extension of the incisions is kept minimal, ideally, within the mid-buccal area of the involved teeth. A triangular buccal flap then exposes the coronal edge of the buccal bone crest. The interdental papillary tissues are dissected with the help of a microblade in both b………….Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book………
Pinhole surgical technique (PST):
The pinhole surgical technique is a minimally invasive technique for the management of marginal tissue recession. The technique is indicated for the recession coverage in Cairo’s RT 1 and RT 2 types of recession. This procedure combines techniques from traditional periodontal surgical procedures, such as coronally positioned flaps and guided bone regeneration, to reverse the gingival recession. The area to be operated is first anesthetized and isolated. For maxillary teeth, a small horizontal incision of 2-3 mm is placed in the height of the mucobuccal fold located above the centermost tooth. Then, a set of instruments specifically designed for PST is used to gain access to the areas of recession. The 16-gauge sterile hypodermic needle or blade of the instrument (specifically designed to make a pinhole) is inserted in the pinhole created in the alveolar mucosa and supra-periosteal dissection is done to elevate the mucosal tissues in apicocoronal direction. In cases with multiple adjacent sites, multiple pinholes may be required. The fibrous and muscular attachments are ………….Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book………. The procedure requires significantly less chair time than conventional procedures with better patient acceptance and less postoperative pain. Along with these advantages, there are also certain limitations of this procedure. The root coverage is less predictable in areas of advanced bone loss due to a lack of bone support for the newly positioned tissue. The procedure can be performed in areas that are free of inflammation.
Review of literature
It is widely accepted that the application of minimally invasive surgical techniques significantly reduces the complications and side effects in the postoperative period. As already stated at the beginning of the chapter, Harrel and Rees (1995) 1 first introduced minimally invasive surgery (MIS) in the periodontal literature as a method of surgical access that minimizes flap reflection and tissue trauma, resulting in the maintenance of critical blood supply and stability of the blood clot within the wound site. The authors conducted multiple studies to identify the effectiveness and success of minimally invasive surgical techniques. In one study, Harrel (1998) 12 analyzed the results of 10 consecutively treated patients 25.1 months after surgery, who received MIS, bone grafting, and a surgical mesh membrane. The author observed a mean probing depth (PD) reduction of 4.10 mm and a mean gain in clinical attachment loss (CAL) of 4.20 mm. Along with this, all teeth that were initially mobile improved in mobility, and no teeth were lost. In a subsequent study, Harrel et al. (1999) 13 published ………….Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book………
In the above-stated studies, Harrel et al. used bone grafts along with a barrier membrane. However, many other investigators advocated the use of enamel matrix derivatives (EMD) instead of barrier membranes as they could provide similar results. So, Harrel et al. (2005) 14 conducted a study using EMD in conjunction with MIS. The study included 16 patients with 160 sites having 6 mm or greater probing depthafter initial nonsurgical periodontal therapy. The defects were accessed with a minimally invasive approach (as described earlier in the chapter) followed by defect debridement, root planing, and root surface modification with either citric acid or 24% ethylenediaminetetraacetic acid (EDTA). After this, EMD and DFDBA graft material was applied. Postsurgical measurements were taken at follow-up visits ranging from 11 to 24 months. The results of the study demonstrated that there was a mean PD reduction of 3.56 mm, mean CAL gains of 3.57 mm, and mean gains in gingival margin to cementoenamel junction (CEJ) measurements of 0.01 mm. The authors concluded that MIS combination EMD and DFDBA resulted in superior reductions in PD and gains in CAL with minimal to no gingival recession as compared to flap surgery, synthetic grafts, bone grafts, or traditional GTR. In a subsequent 6-year follow-up study on the same patients, the authors observed that the clinical parameters remained virtually unchanged 15.
The recent advancement in the field of minimally invasive surgical techniques is the introduction of videoscope (Micro Sight, Q-OpticsInc,www.q-optics.com). It is a high-definition digital camera placed on the end of a flexible tube 2.7 mm in diameter featuring a carbon fiber retractor that may be rotated to aid in flap reflection and a gas shield that prevents blood and contamination from obscuring the camera. It allows improved visualization of the defect once the camera is inserted into the surgical site. A 20 X to 60 X magnification of the surgical site can be obtained with a videoscope which is displayed on a surgical monitor . Harrel et al. (2016) 16 using videoscope-assisted minimally invasive surgery (VMIS),conducted a one-year clinical trial on 18 patients having sites with residual pocket probing depth (PPD) of at least 5 mm and 2 mm loss in clinical attachment level (CAL) following initial nonsurgical therapy. The results of the study demonstrated a statistically significant improvement (P < .001) in mean PPD (4.11 ± 0.98 mm) and CAL (4.58 ± 1.19 mm) in all surgical sites. In another study 17 Harrel et al. reported their observations in 30 patients with 110 qualifying sites treated with V-MIS at a minimum of 36 months follow up. The authors reported a significant improvement (P <0.001) in mean PD and CAL (PD: 3.80 ± 1.18 mm, CAL: 4.16 ± 1.18 mm) in all surgical sites compared with baseline. There was a mean improvement in soft tissue height (0.36 ± 0.64 mm, P = 0.03).
As discussed earlier in the chapter, the minimally invasive surgical technique (MIST) was described by Cortellini and Tonetti (2007) 2 that aimed to produce minimal wounds, minimal flap reflection, and gentle handling of the soft and hard tissues. The authors used enamel matrix derivative (EMD) to treat isolated intrabony defects. However, many studies have reported no additional benefit of using EMD in MIST. In a study, Ribeiro et al. (2011) 18 investigated ………….Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book…………..Content available in book………
Conclusion
Minimally invasive periodontal surgeries are quickly getting popular among clinicians because of their minimum trauma to the tissue and better results. These procedures are a choice of treatment for isolated intrabony defects. Along with these procedures, techniques like pinhole surgical technique are very effective in the management of marginal tissue recession. The primary advantage of these clinical techniques is that they are consistently associated with very limited morbidity to the patient during the surgical procedure, as well as in the postoperative period. Along with this, the chairside time required to perform these procedures is by far shorter than the chair time required for more conventional surgical approaches. In the near future, we can expect more additions to these techniques.
References
References are available in the hardcopy of the website “Periobasics: A Textbook of Periodontics and Implantology”.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:

