Introduction
Periodontium consists of gingiva, periodontal ligament, cementum and alveolar bone. These structures surround and support the teeth and function as a unit to keep the teeth in position. The components of periodontium are supported and surrounded by various anatomical structures. Periodontitis and other pathologies associated with tooth and its supporting structures are commonly treated by surgical intervention. That is why, a sophisticated knowledge of the anatomy of the periodontium and related structures is mandatory to perform any surgical intervention in this region. In the following discussion, we shall discuss in detail the anatomy of various structures associated with teeth and periodontium.
Maxilla
The two maxillae on each side of the face, house the maxillary teeth, contain maxillary sinus and makes the floor of the orbit. Each maxillary bone consists of a body and four processes. The body of maxilla makes the largest part of the bone and is pyramidal in shape. The interior part of the body is hollowed out by the maxillary paranasal air sinuses. The superior surface of the bone forms the floor of the orbit, anterior surface forms the curved external surface of the upper jaw, posterior surface makes the anterior wall of the infratemporal fossa and the medial surface forms a structural component of the nose. The four processes are ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
Maxillary teeth are supplied by the maxillary division of the trigeminal (5th cranial) nerve, which arises as the sensory root from the pons, enters the trigeminal ganglion and divides into three branches viz. ophthalmic, maxillary and mandibular. The mandibular nerve leaves the cranial cavity foramen ovale, maxillary nerve leaves the cranial cavity via foramen rotundum and passes into the pterygopalatine fossa. In this fossa, the maxillary nerve is associated with the pterygopalatine ganglion (secretomotor) from which several other branches are given off before the nerve enters the orbit. These branches include posterior superior alveolar nerves (which enter maxilla via post alveolar foramina), greater palatine nerve, lesser palatine nerve, nasal nerves, lateral and medial posterior superior nasal and nasopalatine nerves. Then it enters the orbit via the inferior orbital fissure becoming the infraorbital nerve. Before the nerve comes out from infraorbital foramen, it gives off a number of branches collectively known as anterior superior alveolar nerve and middle superior alveolar nerve.
The palatine process of maxilla makes the anterior two-thirds of the palate (hard palate). The posterior one-third (soft palate) is a muscular structure with a fibrous foundation. The palatine processes of both the maxillae meet at midline forming a ridge, named raphe palati. In the posterior part of the hard palate, is the greater palatine foramen, the exit from the greater palatine canal and further posterior to it, on the inferior surface of the pyramidal process, are the openings of the lesser palatine canals. The greater palatine neurovascular bundle comes on the palatal surface through this foramen. The greater palatine nerve innervates the palatal gingiva and the hard palate. Most of the nerve fibers of palatine nerves are derived from the sphenopalatine branch of the maxillary nerve.
The descending palatine artery descends through the greater palatine canal with the greater and lesser palatine branches of the pterygopalatine ganglion. It comes out on the palate, from the greater palatine foramen and runs forwards in a groove on the medial side of the alveolar border of the hard palate to the incisive canal. The terminal branches of the artery pass upwards in the incisive canal, where they anastomose with the sphenopalatine artery.
The free gingival graft and connective tissue graft are commonly done periodontal surgical procedures for root coverage and for increasing the width of attached gingiva. The palate is most commonly used site for harvesting the graft. While harvesting the graft, if the incision is made too palatal, the greater palatine neurovascular bundle may get damaged. If the greater palatine artery is cut, excessive bleeding results, which should be immediately controlled by placing a suture noose.
Maxillary sinus (Antrum of Highmore):
Maxillary sinuses are the largest of all the paranasal sinuses. These open in the middle nasal meatus of the nasal cavity. Each sinus is pyramidal in shape and contains three cavities. These are smaller in size (8 x 4 mm) at birth, but gradually enlarge variably and greatly by pneumatization until they reach the adult size by the eruption of the permanent teeth. The process of pneumatization occurs by resorption of the internal walls (except the medial wall) at a rate that slightly exceeds the growth of the maxilla. In younger age, the rate of pneumatization is proportional to the growth of the maxilla but with advancing age, the rate of pneumatization exceeds the rate of growth of the maxilla. The extension of the maxillary sinus in the alveolar process is not only between the roots of adjacent teeth but also between the roots of the individual tooth. The blood supply of ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Clinically, the floor of the maxillary sinus is a limiting factor for implant placement. If there is an insufficient bone for implant placement, direct or indirect sinus lift procedure is done, so that implant with sufficient length can be placed. The membranous lining of the maxillary sinus cavity is known as a Schneiderian membrane. The perforation of this membrane is the most common complication during sinus lift procedures. The sinus lift procedure was first conceived by Tatum in 1976 for implant installation on the atrophic posterior maxilla. Later on, a new procedure where a lateral approach was utilized to reach maxillary sinus was reported by Boyne and James in 1980 6. Maxillary sinus may also possess maxillary sinus septa or Underwood’s septa which are fin-shaped projections of bone. These were first described in 1910 by Arthur S. Underwood. These ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
Mandible
The mandible is the only mobile bone of the facial skeleton. It has a horizontal horseshoe-like body with a flat ramus, projecting upward at each end. The rami are divided into two processes: posterior condylar process and anterior coronoid process. It is formed by intramembranous ossification. The complete structure of the mandible is formed by two hemi-mandibles joined at the midline by a vertical symphysis. Initially developed separately, these hemi-mandibles fuse to form a single bone by the age of 2 years. A lot of changes occur in the mandible with increasing age due to bone remodeling.
Body of the mandible:
The anterior inferior aspect of the lateral surface of the mandible body affords attachment to quadratus labii inferioris and triangularis oris; the platysma is attached below it. Buccinator muscle attachment is present at the superior portion of the mandible. The medial surface of the bone has 2 paired protuberances termed, the superior and inferior mental spines, just lateral to the symphysis. The superior mental spines give attachment to genioglossus whereas inferior mental spines give attachment to geniohyoid muscle. At the inferior border of the mandible, on the lateral aspect of inferior mental ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
The lateral surface of the body of the mandible has mental foramen located below the apices of premolars. It is the opening of the mandibular canal on the external surface of the mandible. A smooth ridge that extends from the anterior border of the ramus downward and forward with diminishing prominence is present on the body of the mandible which is termed as an external oblique ridge. This ridge provides attachment to the buccinator muscle.
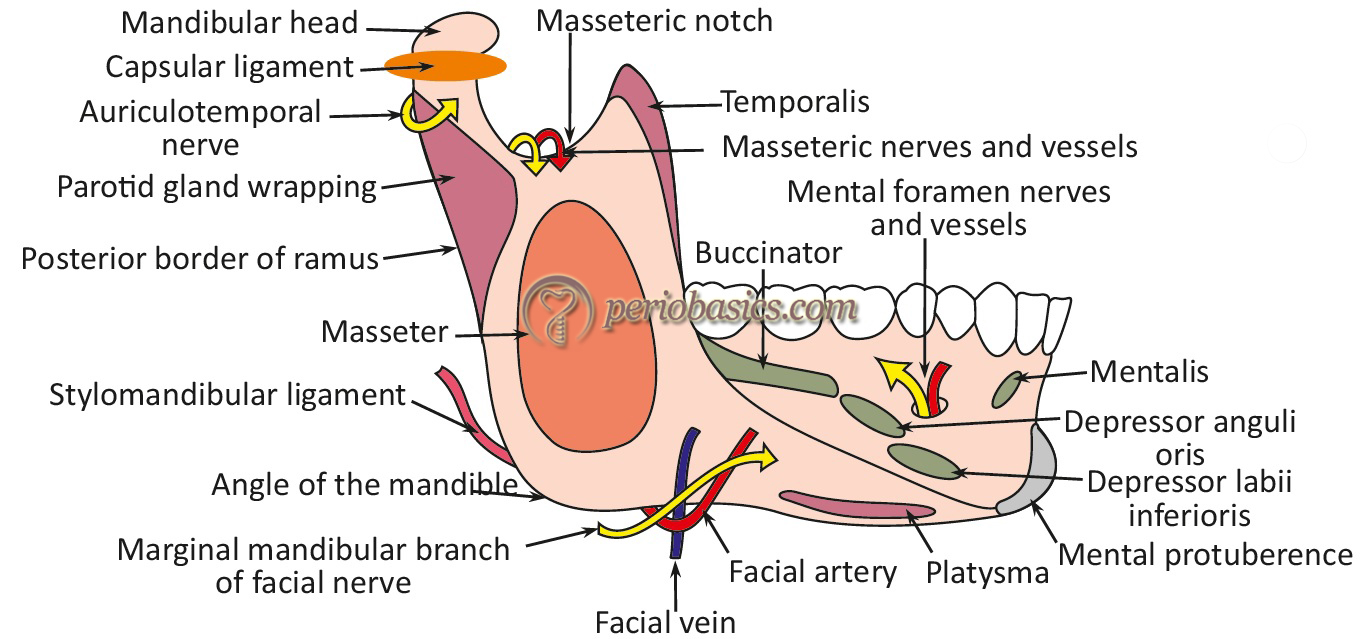
Ramus of the mandible:
The ramus of the mandible extends in the posterosuperior direction from the body of each hemi-mandible. The angle of the mandible is the intersection point formed by the inferior rim of the body and the posterior rim of the ascending ramus. As already stated, the ramus divides into two processes superiorly: anterior coronoid ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
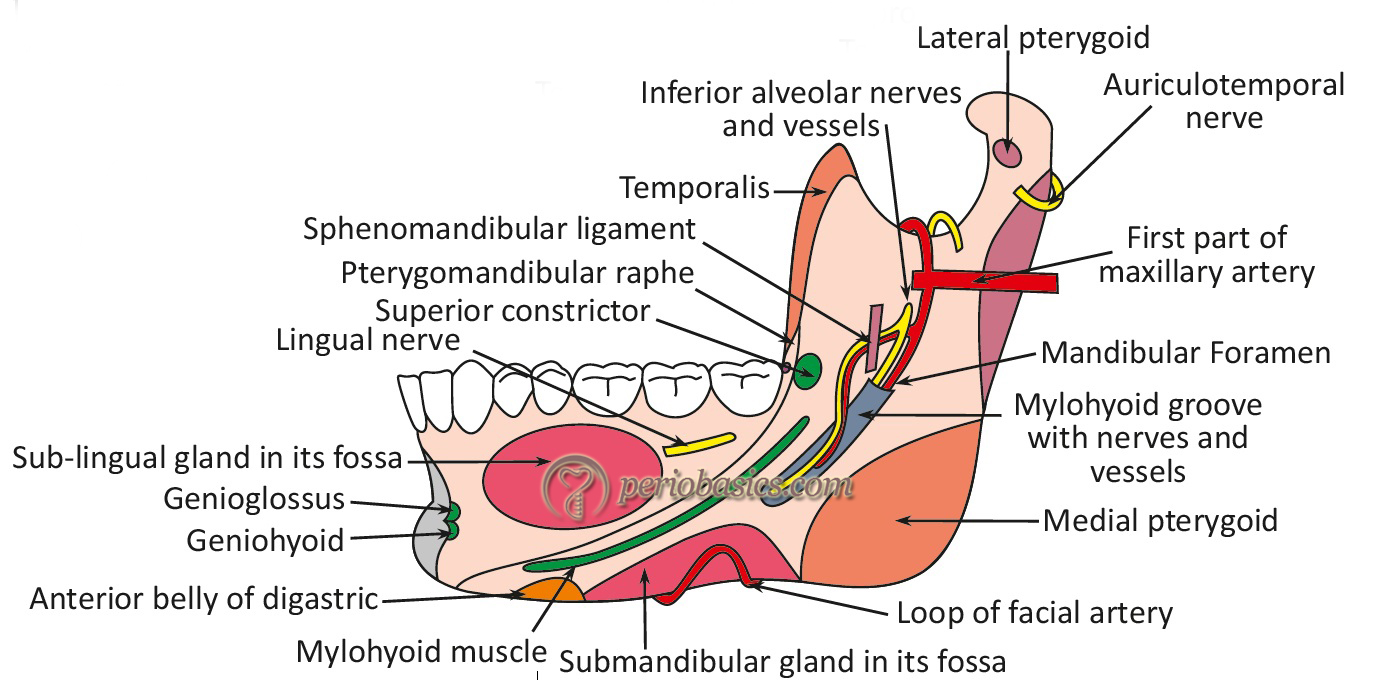
The medial surface of the mandible has mandibular foramen (foramen mandibulae) which leads into the mandibular canal. The mandibular canal runs in the body of the mandible and opens at the mental foramen on the lateral surface of the body of the mandible, in the space between the first and second premolars. The inferior alveolar nerve and blood vessels run through the mandibular canal. The nerve emerging out of the mental foramen is termed as mental nerve, which divides into three branches. One nerve runs forwards and downwards to supply the skin of the chin. Other two nerves run forwards and upwards to supply the mucous membrane and skin of the lower lip and mucous membrane of the labial alveolar surface.
It should be remembered that when inferior alveolar nerve comes out of the mental canal, it runs outward, upward and backward to make a loop known as the anterior loop of mental nerve. It is important to consider while placing dental implant near the opening of mental foramen. CT or CBCT scan can be used to identify the exact location of the mental nerve loop; however, if its position is not clear with CT or CBCT scan, the distal aspect of the dental implant should be placed 6 mm ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
The neurovascular bundle traversing the mandibular canal is an important anatomical limiting factor during dental implant placement. There should be a safety margin of around 2 mm from the implant and inferior alveolar canal. However, in cases with deficient alveolar bone; a surgical procedure such as nerve lateralization is done to place implant below the level of the mandibular canal. Injury to the inferior alveolar nerve results in partial or complete paresthesia of the lip and area of the mouth which is supplied by the nerve. Nortje et al. (1977) 10 on the basis of panoramic radiographs have demonstrated that the vertical mandibular canal position can be divided into four categories,
1. High mandibular canal (within 2 mm of the apices of the first and second molars),
2. Intermediate mandibular canal,
3. Low mandibular canal, and
4. Other variations – these include duplication or division of the canal, apparent partial or complete absence of the canal or lack of symmetry.
The medial edge of the foramen has a projection named lingula of the mandible (lingula mandibulae) which is the attachment site for sphenomandibular ligament. Posterior to lingula, is present a mylohyoid groove which runs downwards and forwards. It lodges the mylohyoid nerve and vessels. Lingual nerve, which is the branch of the posterior division of the mandibular nerve, descends along the ramus of the mandible medial to and in front of inferior alveolar nerve. The nerve lies close to the mucosa in the third molar region. The lingual nerve provides senses to the front two-thirds of the tongue, as well as to the underside that surrounds it. It can easily get damaged during the delivery of local anesthesia and oral surgery procedures.
Maxillary and mandibular tori
The torus is a localized bony protuberance that originates from the cortical plate. When present in maxilla it is called as torus palatines and when present in mandible it is called as torus mandibularis. It is a non-pathological benign growth. Various etiologies have been proposed for their growth including masticatory hyperfunction, genetic factors (common in females), environmental factors and multifactorial etiology. Tori are usually reduced when planning ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
Lymphatic drainage areas of the face and neck
The spread of infection and inflammation most commonly follows the route of lymphatic drainage. Infection in various different parts of the oral cavity may involve different spaces according to their lymphatic drainage. Following table describes lymphatic drainage of various parts of the oral cavity.
| Lymphatic drainage of various head and neck areas. | |
|---|---|
| Lymph nodes | Drainage areas |
| Submental | Mandibular incisors, tip of the tongue, a part of the floor of the mouth in the midline, related gingiva, middle alveolar process, basal bone of the mandible and midportion of the lower lip and chin. |
| Submandibular | All maxillary teeth, mandibular teeth except incisors, inferior nasal cavity, palate, body of tongue, upper lip, lateral portion of the lower lip, angle of mouth, medial angle of eye, and submental lymph nodes. |
| Mandibular | The skin over the mandible, mucous membrane of lips and cheeks. |
| Buccal | Skin of anterior face, mucous membrane of lips and cheeks. |
| Preauricular | Skin inferior to the temple, external auditory meatus, lateral part of the forehead, lateral part of the eyelids, posterior part of cheeks, a portion of outer ear, parotid gland. |
| Postauricular | Scalp above and behind the ear and external ear. |
| Occipital | Scalp posterior to ear, occipital region. |
| Superficial cervical | Pinna and adjoining skin, pre and post auricular lymph nodes. |
| Deep cervical | Submental, submandibular, inferior auricular and tonsillar lymph nodes. |
Potential anatomical spaces around oral cavity
There are several potential anatomical spaces present around the oral cavity which can be easily distended by inflammatory fluid and infection. Although fascias, muscle attachments and bones separate the orofacial region into different compartments, the infection may still spread beyond the dentoalveolar tissue to involve distant spaces 11, 12. To understand various potential spaces in the head and neck region, knowledge of fascia which covers and invests various structures is important.
Fascia is a layer of fibrous tissue that surrounds muscles, vessels, and nerves. In head and neck region, deep cervical fascia has three divisions which separate various structures into three compartments; the investing (superficial), middle and deep layers. The investing or superficial layer is present just below the subcutaneous tissue and platysma. Superiorly it is attached to the lower border of the mandible and inferiorly to the sternum and clavicle 13. The middle layer of fascia encircles central organs which include the larynx, trachea, pharynx and strap muscles. It forms the anterior part of the carotid sheath. Inferiorly, this layer extends into the mediastinum to attach to the pericardium 13. The deep fascia divides into two layers: alar ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
Classification of potential spaces in orofacial region
The potential spaces in the orofacial region can be classified depending on the site/space involved:
Spaces related to the mandible
Submandibular space.
Sublingual space.
Submental space.
Submasseteric space.
Masticator space.
Pterygomandibular space.
Buccal space.
Spaces related to the maxilla
Canine fossa abscess.
Infratemporal spaces.
Buccal space.
Deep fascial spaces of the neck
Lateral pharyngeal space.
Retropharyngeal space.
Danger space.
Prevertebral space.
Description of the individual spaces
Spaces related to the mandible
Submandibular space:
The submandibular space is located superficially on the surface of the mylohyoid muscle between the anterior and posterior bellies of the digastric muscle. Mylohyoid muscle separates the submandibular space from the sublingual space. This muscle also determines the direction of the spread of dental infections. The apex of the first molar is above the mylohyoid line and apices of second and third molars below and the mylohyoid line. So, infection in 2nd and 3rd molars spread into submandibular space, whereas infection in 1st molar spreads into sublingual space. The infection further spreads to lateral pharyngeal space from submandibular space.
Sublingual space:
This is a potential space contained between soft tissue beneath the tongue and above the origin of the mylohyoid muscle. This space contains sublingual gland, its excretory duct and is traversed by lingual nerve and vessels and hypoglossal nerve. Clinically, most important identifying feature for this space involvement is swelling in the floor of mouth, which may deflect the tongue medially and superiorly. In severe involvement, the swelling may affect speech, swallowing, and airway. Infection from this space may spread to involve the submandibular space or across the midline to involve the contralateral sublingual space.
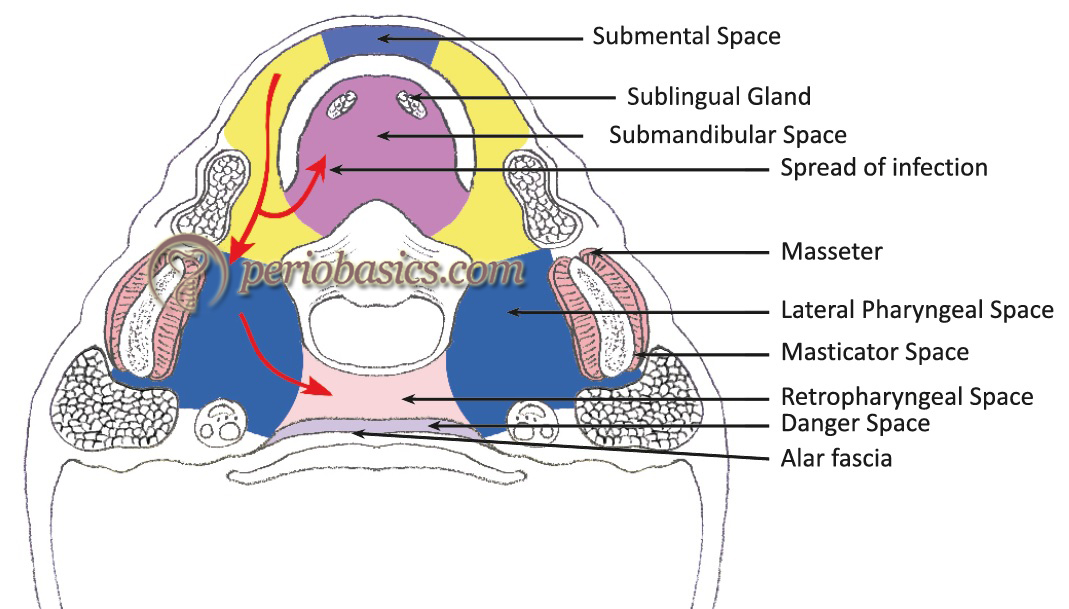
Submental space:
This potential space is present between mylohyoid muscle superiorly and the investing layer of deep cervical fascia covered by platysma inferiorly. Laterally, the area is bounded by the anterior bellies of the digastric muscle. This space also contains submental lymph nodes. Clinically, submental space abscess appears as a firm swelling beneath the chin. This space gets involved due to the infection in lower anterior teeth.
Submasseteric space:
Masseter muscle is divided into three parts, namely superficial, middle and deep. The superficial part is inserted at the lower third of the ramus; the middle part being the smallest part is inserted at the thin line curving posteriorly and superiorly over the middle third of the ramus and the deep part is inserted at the lateral aspect of the coronoid process and the upper third of the ramus of the mandible. The submasseteric space is present beneath the masseter muscle on the ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
Masticator space:
This is a potential deep facial space which is bounded superficially by the superficial layer of the deep cervical fascia. This space contains four muscles of mastication (medial and lateral pterygoid muscles, temporal muscle and masseter muscle) and the ramus and posterior body of the mandible. This space contains important nerves, including all branches of the mandibular division of the trigeminal nerve (masticator nerve, buccal nerve, lingual nerve, and inferior alveolar nerves). It is distinguished from other spaces by the superficial layer of deep cervical fascia. A masticator abscess is usually caused by the advancement of a submandibular abscess. The clinical features of this space involvement include swelling of the face, severe trismus and pain. In cases where only the deep parts of the space are involved, the patient may not have significant facial swelling but usually, has pain and trismus.
Pterygomandibular space:
This potential space is present between the medial surface of the mandible and the medial pterygoid muscle. The medial pterygoid muscle originates from the medial surface of the lateral pterygoid plate, the pyramidal process of the palatine bone and maxillary tuberosity. The muscle is inserted into the medial surface of ramus and angle of the mandible. The important nerves and vessels that traverse this space are lingual nerve, mandibular nerve, and the inferior alveolar artery. This space communicates ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..

Ludwig’s angina:
The bilateral involvement of submandibular, sublingual and submental spaces results in a condition known as Ludwig’s angina. It occurs due to rapidly spreading cellulitis. The bilateral space involvement is associated with elevation and edema of the tongue, drooling of saliva, and airway obstruction.
Spaces related to the maxilla
Canine fossa abscess:
It is a potential bilateral space present between the levator anguli oris muscle inferiorly and the levator labii superioris muscle superiorly on either side of the face in relation to the maxilla. The involvement of this space occurs due to odontogenic infection derived from canine. This space communicates with buccal space posteriorly. The components of this potential space are the angular artery, angular vein and infra-orbital nerve.
Infratemporal space:
The infratemporal space lies superior to the pterygomandibular space. It is located posterior to the maxilla, between the lateral pterygoid plate of the sphenoid bone medially and the base of skull superiorly. It is in continuity with the deep temporal space laterally. The most common reason for the involvement of this space is odontogenic infection derived from maxillary third molars. The infratemporal space contains pterygoid plexus and infection of this space may be ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
Buccal space infections:
The space is anteriomedially bounded by the buccinator muscle and posteriomedially by the masseter, pterygo-mandibular raphe and anterior border of the ramus of the mandible. The superior boundary of the space is zygomatic arch and the inferior boundary is the lower border of the mandible. The lateral covering of the space is provided by superficial cervical fascia and skin. This space contains buccal fat pad, Stenson’s duct, terminal branches of the facial nerve, and the facial artery and veins. The odontogenic infection derived from maxillary bicuspid and molar teeth and even the mandibular equivalents may result in the involvement of this space. The infection is easily diagnosed as there is often marked cheek swelling, but trismus is not severe. The infection from buccal space may extend to involve temporal space or submandibular space with which this space communicates.

Deep fascial spaces of the neck
Lateral pharyngeal space:
The lateral pharyngeal space occupies a critical area in the neck. The space is like an inverted cone with the base of the cone formed by the base of the skull and apex formed by the hyoid bone. Its medial wall is formed by superior constrictor muscle along with styloglossus and stylopharyngeus. The lateral wall is formed by fascia covering the medial pterygoid, angle of the mandible and submandibular salivary gland. Posteriorly, this space is limited by the parotid gland, prevertebral fascia and upper part of the carotid sheath. This space communicates with all other fascial spaces. The space is divided into anterior and posterior compartments by the styloid process. Clinically, most of the times, this space is involved via the spread of infection from ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
Retropharyngeal space:
The retropharyngeal space lies between the visceral division of the middle layer of the deep cervical fascia around the pharyngeal constrictors and the alar division of the deep layer of deep cervical fascia posteriorly. It is located anterior to the danger space and prevertebral space and laterally adjacent to carotid space.
Danger space:
Danger space lies posterior to the retropharyngeal space. This potential space exists between the alar layer and prevertebral layer of the deep fascia. It is named so because it contains loose areolar tissue and offers little resistance to the spread of infection. It is extended superiorly from the base of the skull inferiorly till the diaphragm.
Prevertebral space:
Prevertebral space is a deep space in the neck region defined by the anterior part of the cervical spine and the deep layer of the deep cervical fascia running between the transverse processes of the spine. It extends from the base of the skull till the level of 4th thoracic vertebra. In contrast to all the spaces discussed so far, infection of the prevertebral space usually does not occur due to contiguous extension of other space of the neck. It is most commonly caused by the hematogenous spread of infection and osteomyelitis. In Pott’s disease Mycobacterium tuberculosis may spread to the prevertebral space. The symptoms of the infection of this space vary ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……. Contents available in thr book ……..
Conclusion
A thorough knowledge of the anatomy of the orofacial region is absolutely essential to perform any surgical intervention in this area. Both maxilla and mandible have in proximity, various vital structures which must be handled carefully during surgical procedures. This region is one of the highly vascularized regions of the body, so excessive bleeding may be encountered if any blood vessel is severed. Hence, while performing any surgical intervention, important nerves and vessels should be preserved. However, if any emergency is encountered, one should be well equipped for its management.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

