Introduction to trauma from occlusion
Do abnormal occlusal forces play a significant role in the initiation and progression of periodontal diseases? This question has been our focus of attention for many years. It is generally accepted that trauma from occlusion (TFO) or occlusal traumatism is a separate entity, not related to periodontitis. But, when both the conditions are present simultaneously, it becomes a matter of discussion to designate them as entirely non-associated, partially associated or completely associated conditions. Although many studies have been done to evaluate any relation between progressions of gingival inflammation and trauma from occlusion, conflicting results have been encountered. In the following discussion, we shall try to analyze our current understanding of TFO and its association with inflammatory periodontal diseases.
Definition
Following definitions are commonly used to describe trauma from occlusion,
- When occlusal forces exceed the adaptive capacity of tissues, tissue injury results. The resultant injury is termed as trauma from occlusion 1.
- According to world health organization (WHO), 1978, trauma from occlusion is “damage in the periodontium caused by stress on the teeth produced directly or indirectly by the teeth of the opposing jaw.”
- Injury resulting in tissue changes within the attachment apparatus as a result of occlusal force(s) 2.
- Trauma from occlusion can be defined as structural and functional changes in the periodontal tissues caused by excessive occlusal forces 3.
Etiology of trauma from occlusion
There are many factors involved in the etiology of TFO. Broadly, they can be divided into two categories: precipitating factors and predisposing factors. In TFO, the precipitating factors are the destructive occlusal forces. The predisposing factors are those which contribute to the development of TFO indirectly. They include intrinsic and extrinsic factors.
Precipitating factors:
As already stated, destructive occlusal forces are the precipitating or the primary etiology of TFO. The occlusal forces when within the normal range can be well adapted by tooth-supporting soft tissues. But, when these forces …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Magnitude: When the magnitude of occlusal forces exceeds the normal range of forces for a tooth, due to natural adaptive response, some changes can be appreciated in the periodontal ligament (PDL). There is widening of the periodontal ligament space, an increase in the number of PDL fibers, an increase in the width of PDL fibers and an increase in the density of alveolar bone.
Direction: The principal fibers of the periodontal ligament play an important role in withstanding the occlusal forces and transferring them to the alveolar bone. Normally, they are oriented in such way that they are best capable of withstanding the occlusal forces. But, if the direction of occlusal forces is changed, these fibers are not able to efficiently bear the occlusal forces, hence injury results.
Duration of force application: If the abnormal occlusal forces are subjected to a tooth for a longer duration of time, they cause injury to the periodontal tooth-supporting structures, which can be seen histologically.
Frequency of force application: Frequent application of abnormal occlusal forces results in more damage to the periodontal tooth supporting structures than less frequent application.
Predisposing factors:
These can be divided into intrinsic and extrinsic factors,
Intrinsic factors:
- The orientation of the long axis of the teeth in relation to the forces to which they are exposed.
- The morphological characteristics of the roots. The size, shape and number of the roots determine how occlusal forces are dissipated. In general, short, conical, slender or fused roots are more vulnerable to TFO.
- The morphology of the alveolar process, i.e. the quality and the quantity of the alveolar bone play an important role in absorbing the occlusal forces.
Extrinsic factors:
- Local factors such as plaque which predisposes to the alveolar bone loss.
- Fabrication of long span bridges on few teeth, thus overloading them.
- Injudicious bone resection during surgical periodontal therapy or oral surgical procedures.
- Parafunctional habits as a result of neurosis.
- Other factors include food impaction, overhanging fillings, poorly contoured crowns and bridges and ill-fitting partial dentures.
Historical perspective
The association of excessive occlusal forces and their deleterious effects on tooth and tooth-supporting structures has been established for over 100 years now. Karolyi (1901) 4 implied a cause and effect relationship between traumatic occlusion and periodontal disease progression. Since then a lot of research has been done using autopsy studies, animal studies, and human studies. Two studies supported Karolyi’s hypothesis 5, 6.
In Box’s study (1935) 5, a gold crown was placed on lower incisor of sheep in supra-occlusion thereby increasing the crown-root ratio and buccolingual dimensions of the tooth. After more than three months, the crowned tooth showed increased mobility, slightly increased pocket depth and greater calculus accumulation as compared to other three incisors. Along with this, the pulpal tissue of the crowned tooth showed sub-acute inflammation and the surrounding tissues were inflamed. This study has been criticized by many researchers. Regardless of the results of the study, Box himself did not claim any definite relationship between occlusal trauma and periodontal diseases. In Stone’s study (1938) 6, high …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
There have been fundamental differences between various research groups working to establish the etiological significance of TFO. Some groups say that specific occlusal forces and specific occlusal contacts are responsible for periodontal disease progression, whereas others assert that occlusal forces are not associated with progression of periodontal diseases. Bhaskar and Orban (1955) 7 have contended that the apical migration of epithelial attachment observed by Stone in his study was physiological and not pathological and cannot be considered to be related to occlusal trauma.
Regardless of the results of various studies, most authorities believed that occlusal trauma did not initiate gingivitis or periodontitis and that the microbial plaque was responsible for initiation of gingivitis, which in turn is essential for the development of periodontitis.
Terminologies which have been used to describe occlusal trauma
Various researchers who have studied the effects of traumatic occlusal forces on periodontium have used different terms to denote these abnormal forces and associated occlusion. Following is the description of some initial researchers, who used different terminologies to describe abnormal occlusal forces,
Stillman (1917) 8 used the term “Traumatic occlusion” to describe abnormal stresses capable of producing injury to the dental or periodontal tissues.
Box (1930) 9 used the term “traumatogenic occlusion” to describe these abnormal occlusal stresses and used another term “traumatic occlusion” to describe the functional contact relationship of occlusal surfaces which results in this trauma.
The term “traumatic occlusion” was also used by Ramfjord and Ash (1972) 10.
Muhlemann (1956) 11 used the term “Traumatogenic occlusal situation” to address the factors initiating the abnormal occlusal stresses and “Occlusal trauma” to describe the resulting microscopic lesion.
Orban (1958) 12 and Prichard (1965) 13 gave the term “Periodontal traumatism” to address the tissue injury caused by abnormal occlusal forces and not for the occlusal forces themselves.
Glickman (1974) 14 used the term “Trauma from occlusion” (TFO) to describe these abnormal occlusal forces. In the present discussion, this term has been used to discuss trauma from abnormal occlusal forces.
Review of literature of studies done on the association of TFO and spread of inflammation
Stillman (1917) 8, initially started the discussion over the role of occlusion in the progression of periodontal disease by stating that TFO was the primary cause of periodontal disease and, as such, occlusal treatment was mandatory for the successful treatment and control of periodontal disease. According to him, all other …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Autopsy studies:
These observations made by Stillman set a stage for controversies regarding the association of TFO and spread of inflammation in the inflammatory periodontal diseases. These findings were opposed by Weinman et al. 15-17. In their autopsy studies, Weinman et al. observed that the spread of inflammation into the underlying bone followed the course of blood vessels. They found no correlation between the type of occlusal contact and progression of periodontal inflammation. Later on, various researchers published their findings, which were both in favor and against the association of TFO and spread of inflammation in inflammatory periodontal diseases. To understand this controversy, we must know about “Glickman’s concept” and “Waerhaug’s concept”.
Glickman’s concept
Glickman and Smulow (1962, 1969) 18, 19 in autopsy studies, investigated if TFO could alter the progression of inflammation in the underlying soft tissue and bone. According to their investigation, occlusal trauma could alter the progression of periodontal destruction. Glickman stated that the pathway of spread of a plaque-associated gingival lesion can be changed if forces of an abnormal magnitude are acting on teeth harboring subgingival plaque. Therefore, the periodontium of non-traumatized teeth would present an even destruction (horizontal bone loss), while traumatized teeth would present angular bony defects.
Glickman (1963, 1965) 20, 21 then proposed the “Theory of Co-destruction” to explain the relationship between occlusion and periodontal disease. This theory suggested that occlusal trauma in the presence of plaque-induced inflammation may result in alteration of the normal pathway of inflammation, and development of angular bony defects with intrabony pockets, but that occlusal trauma, in and of itself, did not cause gingivitis and periodontitis 20, 22-24. This theory suggested the presence of a “zone of irritation” (marginal/interdental gingiva; gingival fibers) and “zone of co-destruction” (transseptal/alveolar crest fibers, periodontal ligament, cementum, bone).
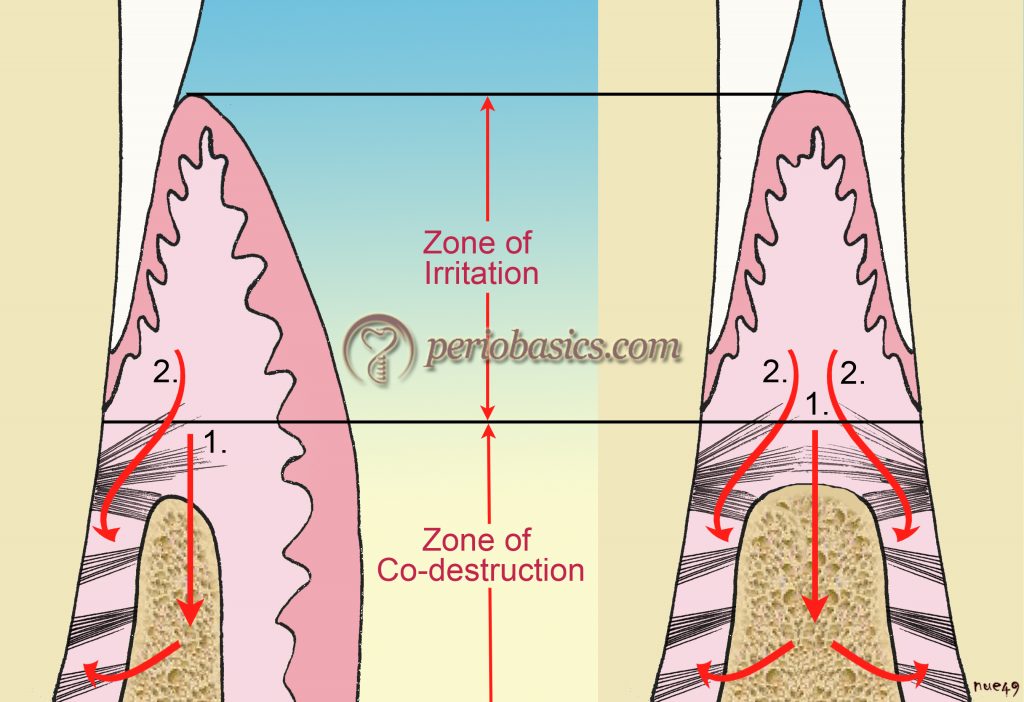
Zone of irritation:
This zone consists of marginal and interdental gingiva. This tissue is bordered by hard tissue only on one side (tooth) and is unaffected by the occlusal forces. In other words, we can say that the gingival inflammation cannot be induced by TFO, but is the result of irritation produced by microbial plaque. Inflammation in the “zone of irritation” causes horizontal bone loss.
Zone of co-destruction:
The zone of co-destruction includes trans-septal/alveolar crest fibers, periodontal ligament, cementum and alveolar bone. It is coronally demarcated by trans-septal and dentoalveolar fibers. The fiber bundles which separate the zone of irritation from the zone of co-destruction are affected by both inflammatory lesion produced by plaque and trauma-induced changes in the zone of co-destruction. As a result of both of these factors, the fiber bundles may get dissolved or may get oriented parallel to the root surface. This may facilitate the direct spread of inflammation from the zone of irritation …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
According to Glickman, TFO is an etiological factor, particularly in situations where angular bony defects combined with infrabony pockets are found around single or multiple teeth.
Waerhaug’s concept:
In his classical study, Waerhaug disputed Glickman’s concept. Waerhaug measured distance between the subgingival plaque and, perimeter of the associated inflammatory infiltrate and the surface of the adjacent alveolar bone. Based on a large number of human autopsy specimens, he concluded that angular defects and infrabony pockets occurred in teeth with TFO and in teeth without TFO, with equal frequency. The reduction in alveolar crestal height was related to the presence of subgingival plaque, ranging from 0.5 to 2.7 mm (mean 1.63 mm) from the alveolar crest. He postulated that loss of attachment and bone are the result of inflammation induced by subgingival plaque and not occlusal trauma. Teeth with narrow interproximal bone develop horizontal defects while teeth with wide interproximal bone were more likely to develop angular or vertical defects.
Animal studies:
Rochester Group (Polson and co-workers) 25-31 and the Gothenburg group (Lindhe and co-workers) 32-38 used primate model and dog model, respectively for investigating the effect of occlusal trauma on periodontal disease progression. These groups differed in some of their findings which may be attributed to the differences in study design and the animal model utilized.
The conclusions of these studies are as follows:
- TFO alone could not cause attachment loss.
- Gingival inflammation is not initiated by occlusal trauma.
- In the absence of inflammation, a traumatogenic occlusion will result in increased mobility, widened PDL, loss of crestal bone height and bone volume, but no attachment loss.
- The excessive jiggling forces in the presence of inflammation did not cause accelerated attachment loss in squirrel monkeys (Rochester Group studies) but accelerated attachment loss in beagle dogs (Gothenburg Group studies).
- Treating the gingival inflammation in the presence of continuing mobility or jiggling trauma will result in decreased mobility and increased bone density, but no change in attachment level or alveolar bone level.
- When excessive occlusal forces were removed, loss of bone density was reversible, except in the presence of periodontitis.
The majority of the animal studies concluded that the application of excessive forces on the teeth creates areas of pressure and tension around involved tooth/teeth. The early changes seen on the tension side include widening of the periodontal ligament space, stretching or tearing of fibers and thrombosis. On the pressure side, necrosis or disorientation of the periodontal ligament fibers, thrombosis, hemorrhages, and undermining bone resorption can be seen. TFO tends to change the shape of the alveolar crest, causing the widening of the marginal periodontal ligament space, narrowing of the interproximal alveolar bone, and shelf-like thickening of the alveolar margin.
In the absence of inflammation, tooth/teeth adapt to the increased occlusal forces (explained later), but in the presence of inflammation the changes in the shape of the alveolar crest may be conducive to angular bone loss, and existing pockets may become intrabony. The control of plaque and gingival inflammation would stop the periodontal disease progression in the presence or absence of excessive occlusal forces. If the excessive occlusal forces continue, the tooth tries to move away from the forces. When the tooth is out of ab-normal occlusal forces, the repair begins. This period is characterized by the formation of new bone and connective tissue. With continued remodeling, the damaged periodontal ligament, cementum, and alveolar bone are completely restored.
The major objection raised regarding the design of animal studies was the quality of the forces. It was said that the occlusal overloading did not replicate the same jiggling type of forces that are observed in humans. To overcome this objection, studies were designed by placing lingual locks on the crowns which forced the tooth buccally with every occlusal closure. An orthodontic appliance then pulled the tooth back lingually with disocclusion. This arrangement prevented …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Human trials:
Gold standards for experimental studies are the blinded, randomized controlled clinical trials. To study the association between TFO and inflammatory periodontal diseases, the study should include identified cases of TFO with periodontal diseases which need to be followed over a long duration of time, which raises serious ethical issues. Therefore, all human studies on TFO have been designed considering the ethical issues which make them less ideal than an ideal clinical controlled trial.
Burgett et al. (1992) 41 in a randomized clinical trial evaluated the effects of occlusal treatment on the outcome of periodontal therapy. Half of the patients selected randomly received occlusal treatment as a part of their periodontal therapy, whereas remaining did not receive any occlusal treatment. All the patients were treated with identical non-surgical and surgical periodontal treatment. The patients were then followed for over two years and then were re-evaluated. The results of the study showed that the group of patients who received occlusal therapy along with periodontal treatment showed a significant improvement in pocket depth in comparison to the group which did not receive occlusal treatment. This study emphasized that occlusal treatment yields a beneficial effect on the outcome of periodontal treatment.
In other investigations 42, 43, the association of occlusal trauma and periodontitis was studied. The results of these studies demonstrated that teeth in patients with occlusal disharmonies (centric relation-centric occlusion, balancing; or protrusive contacts) did not demonstrate any greater severity of periodontitis when compared to teeth without such contacts.
In a study series 44, 45 the effect of parafunctional habits on the long-term prognosis of teeth was investigated. Authors reviewed the change in prognosis and in the number of teeth lost by patients with periodontal disease who had para-functional habits. The study concluded that …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Occlusal forces during jaw movements
The forces exerted on the teeth during jaw movements such as chewing, swallowing and performance of parafunctional habits, including bruxism and clenching, are well tolerated by the tooth-supporting structures. During speech, the tooth contact is minimal, so there are hardly any forces exerted on the teeth. During mastication in normal healthy adults, the mandible typically follows a wide lateral path during closure. The tooth contacts occur on the lateral guiding cusps, typically the cusps of the canines and premolars. The forces exerted on teeth during these contacts are of low magnitude, averaging 81 N lasting for a small-time period (20-50 ms). At final closure in intercuspal position, the forces are much higher, averaging 262 N for a relatively longer duration of time (115 ms). The occlusal forces during swallowing in the intercuspal position are averaging around 296 N for a duration of about 700 ms 46.
Classification of trauma from occlusion
The TFO can be classified as,
- Acute / chronic trauma from occlusion.
- Primary / secondary trauma from occlusion.
Acute trauma from occlusion:
This type of trauma is caused due to abrupt occlusal impact, such as due to biting on a hard object (e.g. biting on an olive pit, a piece of stone in falafel). Another cause of acute TFO is high restorations or prosthetic appliances. The clinical signs and symptoms of the condition include tooth pain and sensitivity to percussion, increased tooth mobility and when the cause is removed, symptoms subside and complete healing takes place. If the cause …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Chronic trauma from occlusion:
It results from the abnormal occlusal forces exerted on the tooth-supporting structures for a longer duration of time. It is more common and is of greater significance than the acute condition because it results in gradual changes in occlusion clinically seen as tooth wear, tooth migration and extrusion of teeth. This condition is usually associated with parafunctional habits such as bruxism and clenching. With the duration of time, pathological changes are seen in the tooth-supporting structures which are discussed in detail later.
Primary trauma from occlusion:
It refers to the injury resulting from excessive occlusal forces applied to a tooth or teeth with normal support 47. Examples include high restorations, drifting or extrusion into edentulous spaces, and orthodontic movement. Once the abnormal forces are removed, the tooth returns to complete health. It must be noted that in the case of primary TFO, there is no alteration in the connective tissue attachment level and it does not initiate the pocket formation. It may be because; the supra-crestal fibers remain unaffected, preventing the apical migration of connective tissue attachment 27.
Secondary trauma from occlusion:
It refers to the injury resulting from normal occlusal forces applied to a tooth or teeth with inadequate support 47. In other words, we can say that even the normal occlusal forces become deleterious to the tooth-supporting structures because the periodontal support is reduced and is not able to withstand the occlusal forces. Due to the loss of tooth-supporting structures, the fulcrum of the tooth …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Stages of tissue response to excessive occlusal forces
Carranza (1967, 1970) 48, 49 has described three stages of tissue response to excessive occlusal forces. These are injury, repair and adaptive remodeling of the periodontium. Following is the description of these stages,
Stage I, Injury:
The immediate result of excessive occlusal forces is the soft tissue injury. The occlusal forces may vary in their magnitude, being slightly excessive, greater than slightly excessive or severely high. The center of rotation of single rooted teeth is located at the junction of middle third and apical third of the tooth, whereas the center of rotation of multi-rooted teeth lies near the furcation area. When excessive occlusal forces are subjected to teeth, they rotate around the fulcrum of rotation, thereby moving away from the deleterious forces. Due to this rotation in the tooth socket, areas of pressure and tension are created on the opposite sides of the fulcrum. If the force is unidirectional, these areas are created on the opposite surfaces, whereas in the case of jiggling forces, these areas may coexist on the same surface.

Slightly excessive forces:
The slightly excessive forces stimulate bone resorption in the areas of pressure, causing the widening of periodontal ligament space. In the areas of tension, elongation of periodontal ligament fibers takes place. The blood vessels on the pressure side are compressed whereas on the tension side they are enlarged 50. In the due course of time, slow remodeling of the alveolar socket takes place.
Greater than slightly excessive forces:
Marked changes in the tooth-supporting structures are seen in the case of greater occlusal forces. The excessive compression of periodontal ligament produces areas of hyalinization 51-53. Areas of necrosis can be seen in periodontal ligament due to excessive trauma to the periodontal ligament fibers and connective tissue cells including fibroblasts. Within 30 minutes of application of such traumatic forces on the tooth, vascular changes can be …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Severely high forces:
Severely high occlusal forces result in thrombosis, hemorrhage, tearing of the periodontal ligament, widening of periodontal ligament space and alveolar bone resorption. Under severely high forces, on the pressure side, there is a disturbance of blood flow in the compressed PDL and cell death in the compressed area of the PDL (hyalinization). The first sign of hyalinization is the presence of pyknotic nuclei in the cells, followed by areas of acellularity, or cell-free zones. The resolution of this hyalinized area starts when cellular elements such as macrophages, foreign body giant cells, and osteoclasts from the adjacent undamaged areas invade the necrotic tissue. These cells also resorb the underside of the bone immediately adjacent to the necrotic PDL area and remove it together with the necrotic tissue. This process is known as undermining resorption 55, 56.
Due to injury caused by occlusal trauma, there is a temporary reduction of mitotic activity of the cells, including fibroblasts (reducing their rate of proliferation) 57 and osteoblasts (reducing the rate of bone formation) 57, 58. In the presence of these excessive occlusal forces, all the above-stated changes take place, but if the forces are removed or tooth moves away from the forces, the periodontium is completely restored.
Stage II, Repair:
Repair is a well-regulated mechanism in which the damaged tissues are replaced by new connective tissue and cells. The extracellular matrix and certain inflammatory mediators play critical regulatory functions, directly or indirectly, facilitating the healing process. Although the reparative activity is always going on in normal periodontium, it is increased during TFO.
To withstand the heavy occlusal forces, the body tries to reinforce the trabeculae within the new bone. This process is known as “buttressing bone formation” 21. When this process occurs within the bone, it is known as ‘central buttressing’ and when it occurs on the facial or lingual surface of the alveolar bone, it is known as ‘peripheral buttressing’. In central buttressing, the endosteal cells deposit bone on the trabecular walls, thereby reducing the marrow space and strengthening the bone to bear increased occlusal load. In peripheral buttressing, shelflike thickening of the bone can be seen on the lingual or the buccal surface of the alveolar bone which is sometimes referred to as “lipping” 18.
Stage III, adaptive remodeling of the periodontium:
If the repair process cannot keep pace with the destruction caused by excessive occlusal forces, adaptive remodeling of the periodontium occurs. In this process of remodeling, a structural relationship is established in such a way that the occlusal forces are no longer harmful to the periodontium. It includes …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Examination and diagnosis of trauma from occlusion
Clinical history of the patient and clinical examination are the cornerstones of correct diagnosis of TFO.
Signs of trauma from occlusion:
Tooth mobility:
It is one of the earliest signs of TFO. As already discussed, the widening of periodontal ligament space and angular bone loss during the adaptive response are the main causes of increased tooth mobility. Although increased tooth mobility is one of the most widely used indicators of occlusal trauma, it may result from bone loss independent of occlusal forces. It may also represent as a self-limiting adaptive response of the host periodontium to the sustained application of occlusal forces 39, 60. Progressive mobility may be suggestive of on-going occlusal trauma, but assessments and monitoring at differing points in time are necessary to make this determination 61.


It is important to differentiate pathologic tooth mobility from physiologic tooth mobility. Normal physiological movement is thought to vary between 10 µm and 150 µm and would not be detectable on clinical examination. One common index used to classify tooth mobility is Miller’s Index (1938) 62:
Class 0
Normal (physiologic) movement when force is applied.
Class I
Mobility greater than physiologic.
Class II
The tooth can be moved up to 1mm or more in a lateral direction (buccolingual or mesiodistal). Inability to depress the tooth in a vertical direction (apicocoronal).
Class III
The tooth can be moved 1mm or more in a lateral direction (buccolingual or mesiodistal). Ability to depress the tooth in a vertical direction (apicocoronal).
Tooth migration:
To avoid excessive occlusal forces, tooth tries to move away from them. Loss of interproximal contacts and migration of tooth from its stable position is one of the signs of TFO.
Wear patterns:
Wear surfaces in the area of interference can be seen. A common reason for the formation of wear facets is bruxism. Bruxism causes the formation of wear facets on the occlusal/incisal surfaces of teeth which can be identified as shiny and irregular areas.
Abfraction, especially in premolars:
Abfraction is caused by lateral deflection. The deflection in the tooth, on deviating from the long axis, can create traction on one side and compression of mineralized structures on the other side. As we know that the tooth structure is composed of enamel, dentin, and cementum, which have a different mineral composition, the effects of lateral forces are different in these tissues. Dentine is comprised on average of 60% inorganic component, and 40% organic component, predominantly proteins and water. On the other hand, 50% of the cementum structure consists of organic matter, and 50% inorganic. Together, dentin and cementum form a structure with relative flexibility. Enamel is highly mineralized (96%) and has a negligible deflection capacity. Thus, cementum and dentin are deformable, but enamel is not. Upon application of lateral forces, the enamel resists the compression forces during deflection, but on the traction side, enamel cannot resist and presents with early fractures and/or cracks in its delicate cervical portion.
On repetition of these lateral forces, enamel is lost in these areas which is known as abfraction. Abfraction can be seen especially in premolars. The wear facets and abfraction appear before the gingival recession (v-shaped recession). So, when these are present, the clinician may conduct a …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
V-shaped or angled gingival recessions:
TFO may promote gingival recession, particularly V-shaped or angled gingival recession. This has been a matter of controversy as many researchers are in favor of this finding 63, 64 and many others are not 65, 66. Researchers who are not in favor of the association of TFO with recession claim that recession results from marginal inflammation due to the presence of plaque, whereas researchers in favor of association of recession with TFO claim that V-shaped or angled gingival recessions with a small fissure in their most apical extremity is directly associated with occlusal trauma 64 and is commonly associated with abfraction 63, 67, 68.
Buccal bone dehiscence:
Buccal cortical bone is thin, especially in the canine and premolar areas. As already stated, due to occlusal trauma, there is a widening of periodontal ligament space at the expense of bone resorption. In these areas, a very little resorption on the periodontal face may result in loss of cervical height and V-shaped bone dehiscence over the buccal face of the root that is affected. The detection of these areas is quite difficult and newer diagnostic techniques such as CT scan or CBCT scans can be used to diagnose these bone defects. With the loss of bone in the marginal area, the periosteum covering the bone persists for an indefinite period. Later on, the periosteum due to lack of bone and blood vessels to nourish it, gets restricted to the bone margins, leaving the root surface exposed to gingival and periodontal connective tissues.
Fremitus test:
This test is used to clinically detect TFO. It measures the vibratory pattern or movement of the teeth when the teeth are placed in the contacting positions and during protrusive and lateral movements. In this test, dampened index finger is placed along the buccal and labial surfaces of the maxillary teeth and the patient is asked to tap the teeth together in the maximum intercuspal position and then grind systematically in the protrusive and lateral movements. The vibratory movement of tooth/teeth is then identified and graded. In the posterior teeth, TFO can be detected with the help of occlusion registration strips/articulating paper. High-pressure points can be detected by the pattern of impressions made by registration strips/articulating paper.
The following classification system is used 69:
Class I fremitus : Mild vibration or movements detected.
Class II fremitus : Easily palpable vibration, but no visible movements.
Class III fremitus : Movements visible with naked eye.
Symptoms of trauma from occlusion
Persistent discomfort on eating:
The patient complains of persistent discomfort during eating. Due to excessive occlusal forces on a tooth or a group of teeth, the patient is not able to satisfactorily chew the food and the teeth under high occlusion cause discomfort.
Thermal sensitivity:
Although, the exact effect of occlusal trauma on dental pulp is still not clear, but studies have demonstrated that there are changes in the vascular supply of the pulp due to excessive occlusal forces 70. It causes increased blood pressure in the pulp and hence tooth becomes sensitive to thermal changes.
Muscle hypertonicity:
The patient complains of tired jaws, especially after rising in the morning and at the end of the day. It is because of the occlusal interferences causing muscle spasm and discomfort.
Radiographic signs of trauma from occlusion
The radiographic signs that can be seen in tooth/teeth with TFO are,
- Thickening of the lamina dura.
- Irregular widening of the periodontal ligament space.
- Vertical bone loss.
- Bone sclerosis in the periapical area or in the interdental bone crest.
- Inflammatory root resorption, more common in advanced stages of occlusal trauma.
- Sclerosing osteitis type of increase in the periapical bone density around a vital tooth on radiograph and positive clinical signs of TFO can guide us to a correct diagnosis and treatment plan.
Is traumatic occlusion reversible?
Although the injury caused by TFO is reversible, there may or may not be a complete restoration of the tooth-supporting structures. If the excessive occlusal forces are neutralized, healing takes place and there is an attempt to restore the normal periodontal structures. The presence of plaque which results in inflammation may impair healing, so the resolution of inflammation should be done.
Trauma from occlusion around implants
An osseointegrated implant is in direct contact with the surrounding bone. There is no periodontal ligament around dental implants. It has been suggested that functional load on dental implants may enhance osseointegration and does not result in the marginal bone loss when the occlusal load is adequately distributed 71. But, occlusal overload adversely affects the implant stability. It has been suggested by …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
One of the key factors controlling bone remodeling at the molecular level is the strain in the surrounding environment. The strain is defined as the change in length divided by the original length. The strain is created when any object is subjected to external stress. In the oral environment, this stress is the occlusal load. The occlusal stresses on the implant prosthesis are transmitted at implant-bone interface 80. The mechanoreceptors present in the bone respond to these stresses and initiate bone remodeling. These mechano-receptors are very sensitive and the microstrain levels 100 times less than the ultimate strength of bone may trigger bone remodeling 81. If the implant is subjected to TFO, high levels of stress are imposed at the implant-bone interface, initiating bone resorption leading to implant failure.
Another important mechanical factor is the modulus of elasticity (stiffness of a material). The modulus conveys the amount of dimensional change in a material for a given stress level. The modulus of elasticity of a tooth is similar to that of cortical bone, but the modulus of elasticity of titanium is 5 to 10 times greater than that of cortical bone 82. There is an engineering principle known as “the composite beam analysis”. According to this principle, when two materials of different elastic moduli are placed together with no intervening material and one is loaded, a stress contour increase will be observed where the two materials first come into contact 83. In osseointegrated implants, these stresses are concentrated at crestal bone level. This observation has been authenticated by photoelastic and 3-dimensional finite element analysis studies where implants were loaded within a bone stimulant 84, 85. This is the reason why the crestal bone loss is often observed around implants.
The density of the bone is directly related to …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Our present understanding of trauma from occlusion
As we know that normal occlusal forces are required to keep periodontal tissue healthy. When the functional demand of the tooth increases, the periodontium accommodates this increased functional demand, which is evidenced by thickened lamina dura and reinforcement of bony trabeculae. If the functional demand of the tooth cannot be met by the periodontium, tissue injury results. If the noxious stimulus is chronic, there is a widening of the periodontal ligament space at the expense of bone resorption. Widening of the periodontal ligament space has a cushioning effect which enables the tooth to bear the excessive occlusal forces. The type of periodontal pocket that develops in response to …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Although, many concepts in trauma from occlusion still need to be clarified, with the analysis of the present data, the following conclusions can be drawn,
- There is presently no evidence that trauma from occlusion can cause gingivitis or periodontitis or may accelerate the progression of gingivitis to periodontitis.
- Periodontal ligament is a dynamic tissue and it has a capability to adapt to the increased occlusal forces which occurs by widening of the periodontal ligament. Increased occlusal forces cause alveolar crest bone resorption. Tooth mobility increases due to excessive occlusal forces. However, this injury is reversible and if the excessive occlusal forces are eliminated, the tooth and periodontium come back to their normal state of function.
- Occlusal trauma may be a cofactor which can increase the rate of progression of an existing periodontal disease.
- Correction of occlusal abnormalities is not a substitution of the conventional methods of resolving plaque-induced inflammation. Thus, as a rule, the first step in the treatment of the patient should be to resolve inflammation by the elimination of local factors by scaling and root planing.
- Occlusal therapy is an important component of the overall periodontal treatment of the patient to ensure smooth occlusal functions and patient comfort.
Treatment of trauma from occlusion
The treatment of TFO involves removal of the excessive occlusal forces and bringing the tooth/teeth in a comfortable position. Many treatment modalities have been advised to treat TFO 88. These include,
- Occlusal adjustments.
- Management of parafunctional habits.
- Splinting of teeth.
- Orthodontic tooth movement.
- Occlusal reconstruction.
- Extraction of selected teeth.
Occlusal adjustment
The reshaping of the occlusal/incisal surfaces of the tooth/teeth or coronoplasty involves selective grinding of the teeth to achieve a harmonious relationship of teeth in the opposite arches. There are many controversies regarding the grinding of occlusal surfaces of teeth. These are regarding the extent of selective grinding of teeth and its long-term effectiveness. The 1989 World Workshop in Periodontics listed the following indications and contraindications for occlusal adjustment 89:
Indications for occlusal adjustment:
1. To reduce traumatic forces to teeth that exhibit:
a. Increasing mobility or fremitus to encourage repair within the periodontal attachment apparatus.
b. Discomfort during occlusal contact or function.
2. To achieve functional relationships and masticatory efficiency in conjunction with restorative treatment, orthodontic treatment, orthognathic surgery or jaw trauma when indicated.
3. As adjunctive therapy, that may reduce the damage from parafunctional habits.
4. To reshape the teeth, which are contributing to soft tissue injury.
5. To adjust marginal ridge relationships and cusps that are contributing to food impaction.
Contraindications for occlusal adjustment:
1. Occlusal adjustment without careful pre-treatment study, documentation, and patient education.
2. Prophylactic adjustment without evidence of the signs and symptoms of occlusal trauma.
3. As the primary treatment of microbial-induced inflammatory periodontal disease.
4. Treatment of bruxism based on patient’s history without evidence of damage, pathosis, or pain.
5. When the emotional state of the patient precludes a satisfactory result.
6. Instances of severe extrusion, mobility or malpositioning of teeth that would not respond to occlusal adjustment alone.
Management of parafunctional habits
Parafunctional habits like bruxism cause excessive forces on the periodontium resulting in injury to the periodontium. The correct diagnosis of bruxism should be made by taking the history of the patient and associated clinical findings. A night guard is used to prevent night grinding of the teeth. It also helps in relaxation of the masticatory muscles.
Splinting of teeth
Splinting is the mechanism of joining adjacent teeth, thereby reducing their mobility and converting them into a single unit which is expected to withstand the occlusal forces better than the individual tooth. However, it must be understood that the removal of abnormal occlusal forces should be our primary target. Glickman et al. (1961) 90 in a study, clearly showed that although fixed splints provide some beneficial distribution of occlusal forces, the ideal way to alleviate excessive occlusal forces that cause tooth/teeth mobility is to remove the destructive occlusal contacts. Following are indications and contraindications of splinting as listed in the 1989 World Workshop in Periodontics 89.

Indications of splinting:
1. Stabilize teeth with increasing mobility that have not responded to occlusal adjustment and periodontal treatment.
2. Stabilize teeth with advanced mobility that have not responded to occlusal adjustment and treatment when there is interference with normal function and patient comfort.
3. Facilitate treatment of extremely mobile teeth by splinting them prior to periodontal instrumentation and occlusal adjustment procedures.
4. Prevent tipping or drifting of teeth and extrusion of unopposed teeth.
5. Stabilize teeth, when indicated, following orthodontic movement.
6. Create adequate occlusal stability when replacing missing teeth.
7. Splint teeth so that a root can be removed and the crown retained in its place.
8. Stabilize teeth following acute trauma.

Contraindications for Splinting:
1. When the treatment of inflammatory periodontal disease has not been addressed.
2. When an occlusal adjustment to reduce trauma and /or interferences has not been previously addressed.
3. When the sole objective of splinting is to reduce tooth mobility following the removal of the splint.

Orthodontic tooth movement
Moving tooth/teeth through orthodontic forces is one of the ideal treatments for TFO. But, applications of orthodontic forces also have their own indications and contraindications. A periodontally compromised tooth with little bone support is not a good candidate for orthodontic tooth movement. Moving the tooth in a position which will further compromise its stability and long-term prognosis is also not desirable. Tooth movement which shall eliminate abnormal occlusal forces as well as improve its long-term prognosis should be our primary goal during application of orthodontic forces on the tooth.
Orthodontic treatment itself may induce some occlusal interferences, but these are temporary and generally do not last long enough to significantly injure the periodontal support structures. The causes of occlusal trauma following orthodontic treatment are usually related to premature contacts arising from the position of teeth, inappropriate occlusal morphology between antagonist teeth and overload on lateral incisors when these teeth are laterally involved in canine guidances. Usually, after completion of orthodontic treatment, it is not widespread conduct to perform a thorough occlusal analysis. The interferences, if present, are allowed to settle down on their own over a duration of time by natural “accommodation”. However, in many cases, the patient …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Occlusal reconstruction
Complete occlusal reconstruction involves redesigning complete occlusal scheme. It is done in cases, whereby no other means occlusal equilibration can be achieved. It involves re-designing the occlusal contacts by giving crowns, bridges or implant-supported prosthesis. This kind of procedure requires a thorough knowledge of occlusion. It must be remembered that this procedure completely changes the occlusal scheme, so the changed occlusion should be thoroughly studied first on articulated casts and then it should be replicated into the patient’s mouth.
Extraction of selected teeth
Rarely, a tooth is extracted to correct TFO. In certain situations extraction of selected tooth/teeth may be done to correct TFO, such as a tooth with extensive periodontal involvement with poor prognosis, the extraction of which may improve the prognosis of the remaining teeth. During orthodontic treatment also extraction of certain teeth may be indicated for proper final positioning and alignment of remaining teeth.
Conclusion
Teeth and their surrounding supporting structures can well withstand the normal occlusal forces. However, abnormal occlusal forces adversely affect periodontal health and hence, the long term prognosis of teeth. Abnormal occlusal forces and their role in the progression of periodontal diseases have been studied for over last hundred years. From the above discussion, it is clear that trauma from occlusion does not cause gingival inflammation, but can modify the spread of inflammation into the underlying connective tissue. Elimination of the abnormal occlusal forces along with stabilization of the involved tooth/teeth is the primary treatments for TFO. Thus, it can be concluded that elimination of periodontal inflammation as well as TFO is essential to achieve complete periodontal health and to improve the prognosis of teeth.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

