Introduction
Achieving complete periodontal health is the ultimate goal of the periodontal therapy. A thorough understanding of the etiopathogenesis of the periodontal diseases is essential to effectively treat them and to achieve complete periodontal health. The clinician should be able to judge the periodontal condition of the patient and establish a treatment plan that effectively treats the periodontal problems of the patient. In the following paragraphs, we shall discuss why periodontal treatment is important and what outcomes are expected after this treatment. The rationale of periodontal treatment can be best explained by longitudinal studies that have compared the surgical and non-surgical periodontal therapies in periodontitis patients.
Longitudinal studies comparing outcomes of surgical and non-surgical periodontal therapies
There are several treatment modalities in periodontics which can be broadly divided into non-surgical and surgical periodontal therapies. The non-surgical periodontal therapies include plaque control, supra, and subgingival scaling and root planing and use of chemotherapeutic and host modulation agents. The surgical periodontal therapy includes resective or regenerative procedures (discussed in detail in the “History of surgical periodontal pocket therapy and osseous resective surgeries”). In the late 60’s and continuing into the 70’s and 80’s, series of longitudinal studies were done to evaluate the outcome of periodontal therapy, particularly in the long duration of time. These longitudinal studies compared the non-surgical and surgical periodontal therapy and have provided a strong evidence for the improvement in periodontal health following these treatments.
The primary aim of these studies was to compare the long-term outcome of various non-surgical and surgical periodontal therapies. Irrespective of the type of periodontal treatment done, all the studies have reported an improvement in the periodontal status of the patients. The studies are often identified by their geographic location, such as Michigan study I, II, and III done by Ramfjord et al. 1-7, Swedish study I, II, III, IV, and V by Lindhe and co-workers 8-14, Minnesota study by Pihlstrom et al. 15-17, Denmark study by Isidor and Karring 18, 19, Loma Linda study by Badersten et al. 20-28, Arizona study by Becker et al. 28-31, Nebraska study by Kaldahl et al. 32-34, and others. A review 35 has discussed theses studies in detail. Thus, based on the results of these studies, the aim and objectives of periodontal treatment can be explained.
Objectives of periodontal therapy
The main objective of periodontal therapy is to achieve complete periodontal health. The first and foremost step in periodontal treatment is the elimination of inflammation. Local therapy accomplishes the removal of local factors like plaque and calculus, which leads to the resolution of inflammation. Identifying occlusal problems and occlusal harmonization is important to eliminate undue forces on the periodontium. If the patient has moderate or advanced periodontal destruction, surgical therapy is required to reduce/ eliminate the pockets. Along with reduction/elimination of pockets, it is ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Non-surgical periodontal therapy:
Elimination of primary etiology, which is plaque and calculus is the first step in the periodontal treatment of the patient. The resolution of inflammation requires thorough scaling and root planing. A biologically acceptable root surface is achieved through this process which is required during periodontal healing. Other factors which favor plaque accumulation such as overhanging restoration margins are also corrected during the treatment. Analysis of the occlusion is very important because abnormal occlusal forces may adversely affect the periodontal tissue. Occlusal harmonization is required to eliminate abnormal occlusal forces which also aid in periodontal healing.
After the resolution of inflammation, the primary signs of inflammation such as bleeding on probing and swelling subside. In the case of moderate to advanced periodontitis where deep periodontal pockets are present, the gingiva may become fibrotic due to repeated healing in the inflamed tissue. Surgical therapy is then executed to achieve pocket depth reduction and physiological periodontal architecture of the tissues. In conditions like localized and generalized Grade C periodontitis, putative periodontal pathogens have been isolated from the connective tissue supporting the periodontal pocket. So, systemic antimicrobial therapy is employed to eliminate these pathogens from the connective tissue. Furthermore, diseases such as diabetes mellitus may alter the rate of periodontal destruction and also negatively affect periodontal healing. So, it becomes necessary to control these systemic conditions to achieve the best results of the treatment.
Host modulation therapy (HMT) is relatively a new concept and is being investigated. Some drugs have been shown to modulate the host response and prevent destruction caused by the host immune response. Tetracycline group of drugs has been widely investigated for their host response modulation. In addition, non-steroidal anti-inflammatory drugs such as flurbiprofen, ibuprofen, etc., have been shown to decrease periodontal bone loss. Although, HMT is still under investigation, but certainly it has got great potential in the future.
Systemic therapy may also be provided from a preventive point of view. It is well established that various periodontal treatments cause bacteremia. The bacteremia caused due to ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……
Surgical periodontal therapy:
The surgical periodontal therapy can be broadly divided into resective and regenerative periodontal therapy. The resective periodontal therapy involves the removal of the alveolar bone in order to achieve a periodontal architecture that is best suited for the maintenance of periodontal health. The regenerative periodontal therapy aims at the regeneration of the lost periodontal tissues as a result of periodontal disease progression. The choice of the treatment depends on various factors including the rate and extent of disease progression, type of bone defects, and status of the soft tissue (presence of gingival recession, the thickness of gingiva etc.), occlusal considerations, systemic condition of the patient, patient motivation and economic status of the patient. The ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……
What does periodontal therapy accomplish?
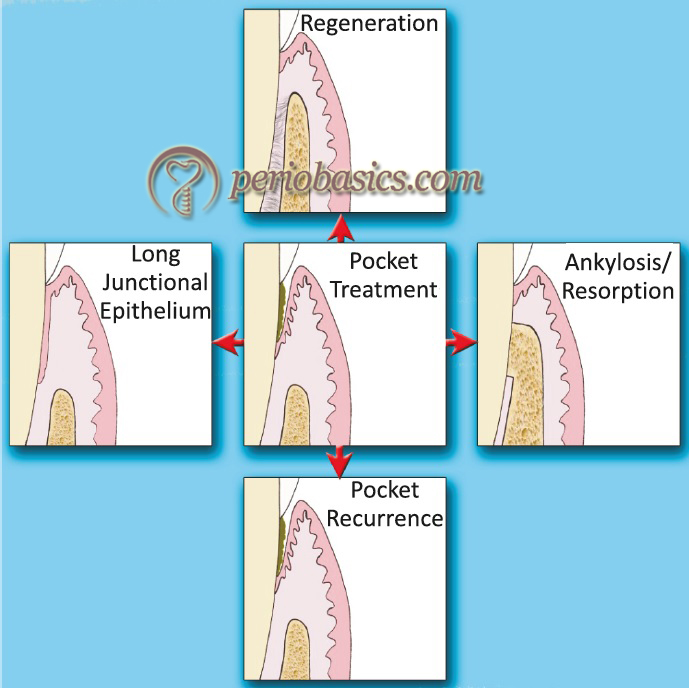
Like other parts of the body, the basic steps in healing in periodontal tissues are the same. Clinically, after periodontal treatment, a periodontium free of inflammation is achieved. But, as far as healing at the microscopic level is concerned, patterns of healing may result in different outcomes. Dentogingival unit is a dynamic structure that attaches the periodontal soft tissue to the tooth. Its integrity is first to be lost during inflammation, so its re-establishment is the first sign of healing. A lot of research has been done to understand the basic mechanism of healing in periodontal tissue. Our present understanding suggests following patterns of healing in the periodontal tissues,
New Attachment:
New attachment is the embedding of new periodontal ligament fibers into new cementum and the attachment of the gingival epithelium to a tooth surface, previously denuded by disease 36. It employs the reunion of connective tissue with a root surface that has been deprived of its periodontal ligament. This occurs with the formation of new cementum with inserting collagen fibers which can be verified by histological examination 37.
Regeneration:
Regeneration is defined as the reproduction or reconstruction of a lost or injured part in such a way that the architecture and function of the lost or injured tissues are completely restored 36. Periodontally, this definition implies to ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……
Repair:
It is the biological process by which continuity of disrupted tissue is restored by new tissues which do not replicate the structure and function of the lost tissue 38. In other words, tissue formed, does not allow the original morphological or functional restoration of the tissue being considered and is considered as non-functional scarring. Thus, the long epithelial attachment is interpreted as repair, since there is no restoration of the periodontal structural architecture and it only acts as a cover to the underlying structures.
Reattachment:
Reattachment refers to repair in areas of the root not previously exposed to the pocket, such as after surgical detachment of the tissues or following traumatic tears in the cementum, tooth fractures, or the treatment of periapical lesions. In the past, term reattachment was used to describe the ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……
Epithelial adaptation:
It is the close apposition of gingival epithelium to the tooth without the complete obliteration of pocket and no gain in the attachment of gingival fiber attachment. As already stated, epithelial adaptation is the result of repair because it just covers the underlying connective tissue.
Factors affecting the outcome of periodontal therapy
The factors that affect the outcome of the periodontal therapy can be broadly divided into local and systemic factors.
Local factors:
The local factors that affect the outcome of the periodontal therapy include the anatomical position of the tooth/teeth in the arch, local plaque retentive factors such as restoration overhangs, extent of tissue manipulation during the surgical procedure and post-operative maintenance of the surgical area by the patient. An adequate vascular supply is essential to ensure adequate healing of the operated area. The operator should strictly follow the principles of periodontal surgery (read “Principles of periodontal surgery”), so that an uneventful healing can be ensured. The presence of plaque adversely affects the healing process, so the patient should be well motivated to maintain plaque control well before the surgical periodontal therapy is initiated. Another factor that affects wound healing is adequate immobilization of the healing area.
Systemic factors:
The overall systemic condition of the patient is directly related to the healing process in his/her body. With aging, the healing capacity of the body reduces, probably because of the atherosclerotic changes in the vasculature resulting in decreased oxygen supply to the healing area 39, 40. The systemic diseases such as diabetes mellitus adversely affect the outcome of the periodontal treatment and post-operative healing. The unmodifiable factors like age of the patient cannot be controlled, but the modifiable factors such as diabetes mellitus should be controlled prior to the periodontal surgical procedures to achieve the appropriate outcome of the treatment.
The immunocompromised patients, either due to disease or systemic administration of immunosuppressants, also are more likely to have impaired healing than the normal patients. The environmental factors like stress and smoking also have an adverse effect on wound healing. The stress management is recommended for ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……
Long- term results of periodontal therapy
The long term evaluations (both retrospective and prospective) of different conventional modalities of periodontal therapy have demonstrated its effectiveness in maintaining the dentition in comfort and function, providing regular maintenance is instituted 41, 42. At present, we have many treatment modalities to treat periodontitis. However, successful periodontal therapy requires the cooperation and commitment of the patient. They not only need to perform routine oral hygiene as effectively as possible, but they should also commit to a regimen of periodic professional maintenance. Without it, successful long-term results are less likely to occur. The long-term success of periodontal treatment is primarily based on patient cooperation and motivation.
Conclusion
With the above background, now we can systematically go ahead with the discussion on different clinical aspects of periodontal treatment, starting with the non-surgical periodontal therapy followed by the surgical periodontal therapy. We have come a long way in our journey to understand the etiopathogenesis of periodontal diseases and our scientific knowledge regarding periodontal diseases has been enriched quite a bit. In the upcoming chapters, we shall read in detail, various non-surgical and surgical periodontal treatments.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

