Introduction to periodontal dressing
The rationales 29, 30 for placing periodontal dressing are protection of wounds from post-operative irritation, preventing trauma, preventing salivary contamination, preventing gingival detachment from root surface, preventing coronal displacement of the flap where the flap has been apically positioned, providing additional support to free gingival grafts, splinting mobile teeth, reducing tooth hypersensitivity during the first hours after surgery, and to provide patient comfort. According to Prichard (1972) 31, the periodontal dressing is used to prevent postoperative hemorrhage and to protect the wound area from contact with food. Further, he stated that it “has no other virtue”. In spite of all fore-stated advantages, indications for periodontal dressing are limited. Studies 32, 33 using a split-mouth design have demonstrated that surgical sites with dressing resulted in more amount of plaque accumulation as compared to similar sites with no dressing. The authors concluded that dressing aids little to the healing process. In the following sections, we shall study the present status of periodontal dressings.
Ideal properties of periodontal dressing
The properties of an ideal dressing material include 34,
- It should be slow setting to allow manipulation;
- It should have a smooth, non-irritating surface;
- It should not interfere with healing;
- It should be flexible enough to withstand distortion and displacement in the mouth without fracturing;
- It should be strong and coherent without being bulky, and
- It should have good adhesive properties to the tooth surface and soft tissue, along with dimensional stability to prevent salivary leakage and accumulation of plaque and debris.
History of periodontal dressing
History of periodontal dressing dates back to 1918 when Zentler 35 reported the use of a periodontal dressing in the form of iodoform gauze. In 1923 Dr. A W Ward introduced the first commercially available periodontal dressing material called “Wonderpak”. It was made up of zinc oxide and eugenol, alcohol, pine oil, and asbestos fibers. Periodontal dressings containing eugenol had some inherent problems associated with them. These include, a persistent taste of eugenol, the rough surface of the set material, and the tendency to cause tissue necrosis. These led to the introduction of non-eugenol dressings in the late 1950’s 36. Later on, light-cured dressings were introduced which are especially useful in the anterior tooth region and particularly following mucogingival surgery because their esthetic appearance is acceptable and these can be applied over the grafted soft tissue without its dislocation. The composition of the periodontal pack has changed over a period of time and potential tissue irritants have been eliminated from its composition.

Types of periodontal dressings
There are primarily three types of periodontal dressings: zinc oxide eugenol dressings, zinc oxide non-eugenol dressings, and dressings containing neither zinc oxide nor eugenol. Zinc oxide eugenol dressing is also known as ‘hard pack’ whereas zinc oxide non-eugenol dressing is known as ‘soft pack’. Other ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Zinc oxide eugenol dressing:
The components of zinc oxide eugenol dressing consist of powder and liquid. These dressings are available in powder-liquid or paste forms.
Powder-liquid form:
The powder-liquid dressing is prepared by mixing the powder and liquid. The powder consists of zinc oxide, tannic acid, rosin, kaolin, zinc stearate, cellulose fibers and asbestos. The liquid contains eugenol, peanut oil, rosin. The specific functions of its components are,
Zinc oxide: Antiseptic and astringent.
Tannic acid: Haemostatic.
Rosin: Filler, increases strength and speeds the reaction.
Asbestos: Binder and filler.
Cellulose fibers: Improve setting.
Eugenol: Anesthetic, antiseptic, and obtundent.
Peanut oil: Regulates the setting time.
The setting reaction between zinc oxide and eugenol results in the formation of zinc eugenolate. After the completion of the reaction, some eugenol remains un-reacted, which may induce a burning sensation or allergic reaction in the mucosa. Tannic acid is added in the dressing material as a hemostatic agent, but its systemic absorption is associated with liver disease 37. Asbestos, which was added as a filler, is toxic and has been associated with the development of asbestosis, lung cancer and mesothelioma 38. Hence, it is no more added in periodontal dressing materials. On the other hand, some ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Paste form:
These are supplied in two paste system. One tube contains base zinc oxide (87%) and fixed vegetable or mineral oil (13%). It also contains lorothidol as a fungicide. The other tube contains an accelerator which is oil of clove or eugenol (12%), gum or polymerized rosin (50%), filler (silica type) (20%), lanolin (3%), non-ionizing carboxylic acids and chlorothymol (bacteriostatic agent).
Disadvantages of zinc oxide eugenol dressing material
There are some problems associated with the use of eugenol-containing dressing material,
- The taste of the material is spicy, which is unpleasant.
- In some patients, it causes a burning sensation.
- It lacks adequate smoothness.
- It is difficult to adapt.
- It has more chances of fracturing.
Zinc oxide non-eugenol dressings
These periodontal dressing materials set due to the reaction between the metallic oxide and fatty acid. These periodontal dressings do not contain materials like asbestos or eugenol, so are devoid of problems associated with these substances. The examples of these dressing materials are Coe-pak, Peripac, Vocopac, Periocare, Septopack, Perioputty, Zone periodontal pack, Nobeteca and PPC noneugenol pack.
Coe-pak:
The most common and widely used non-eugenol dressing is Coe-pak (De Trey/Denstply, Konstanz, Germany). It is supplied in two paste system where one paste contains cellulose, rosin, natural gums (for cohesiveness) and waxes, fatty acids, chlorothymol (bacteriostatic agent), zinc acetate and alcohol. It is referred to as the base paste. The second paste which is called as accelerator paste contains zinc oxide, vegetable oil (for plasticity), chlorothymol, magnesium oxide, silica, synthetic resin, coumarin lorothidol (a fungicide).

Mechanism of mixing and placement of dressing:
Coe-pack periodontal dressing is prepared by mixing equal lengths of the base and accelerator pastes to obtain a paste with a uniform color. Within 2-3 minutes the material loses its tackiness and becomes moldable. The material remains workable for 15-20 minutes during which it is placed over the operated area and is adapted. Once in workable condition, the material is then rolled into two strips which are approximately of the same length as the operated area. The end of one strip is adapted at the distal end of the last tooth of the operated area and is adapted along the whole length of the operated area. The dressing material is gently pressed along the margins and interproximal areas. The second strip is then adapted on the lingual/palatal side and both the ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
PeriPac:
PeriPac (GC America Inc., Chicago, USA) is supplied as a single paste. The paste consists of calcium sulfate, zinc sulfate, zinc oxide, ascorbic acid, polymethyl methacrylate, dimethoxy tetraethylene glycol, flavoring agent and iron-oxide pigment. The material sets as soon as it comes in contact with water. The material sets in approximately 20 minutes. The material is taken out from the jar and with a dry sterile spatula and deposited on a paper napkin. The material is then rolled to make two strips of the approximate length of the operated area and is adapted in the same manner as described for Coe-pack. While applying the dressing, figures should be moistened with water to prevent the material sticking to them. The dressing should not be overextended to cover mobile alveolar mucosa. The material ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……….

Vocopac:
Another periodontal dressing material is Vocopac (Voco, Cuxhaven, Germany). It is supplied in a two paste system: accelerator and base pastes. The main constituents of vocopac are purified colophonium, zinc oxide, zinc acetate, magnesium oxide, fatty acids, natural resin and natural oils and colorant e127. In patients who are allergic to the colorant, this dressing is contraindicated.
PerioCare®:
PerioCare® (Pulpdent®Corp., Watertown, MA, USA) is a two tube system (paste and gel) which sets resiliently hard in the oral cavity. After mixing the paste and gel for 45-60 seconds, the dressing material can be picked up with wet fingers. It has a working time of 4-5 minutes and sets in 15 minutes.

SeptoPack:
SeptoPack (Septodont, Saint-Maur-Des-fosses, France) is supplied as a self-hardening paste in 60 gm packaging. The main components of the material are amyl acetate, dibutyl phthalate (10-25%), methyl polymethacrylate, zinc oxide (20-50%) and zinc sulfate (2.5-10%). Medicaments such as antimicrobials can also be combined with the paste before placement of the dressing. The material sets by chemical reaction when it comes in contact with water. The working time for this material is 2-3 minute and it completely sets in 20-30 minutes.

Perio Putty:
Perio Putty (Cadco Dental Products Inc., Los Angeles, CA, USA) is another non-eugenol periodontal dressing which in addition to the basic components contains methylparabens and propylparabens (fungicidal) and benzocaine (topical anesthetic).
PeriogenixTM:
PeriogenixTM (OroScience (New Line Medical Inc., Lafayette, LA, USA) contains perfluorodecalin, purified water, glycerine hydrogenated phosphatidylcholine, cetearyl alcohol, polysorbate 60, tocopheryl acetate, benzyl alcohol, methylparaben, propylparaben, and oxygen. The dressing has been shown to aid in the healing process by multiple mechanisms 40.
Periodontal dressings containing neither zinc oxide nor eugenol
Light cure periodontal dressings:
These include single component light-activated dressing material which is placed over the tissue surface followed by curing with the visible light application. It is cured in increments and after curing it maintains its elastic properties. The dressing has a tinted pink translucent color and is preferred in the anterior tooth segment and for mucogingival surgical procedures. Bucrylate® (Ethicon Inc., Somerville, NJ, USA) and Barricaid (Dentsply International Inc., Milford, DE, US) are the examples for light cure periodontal dressings.
Collagen containing periodontal dressings:
Collagen is a physiological component of connective tissue. It forms a physiologic interface when placed over healing tissue and thus enhances healing by deposition and organization of the fibers in granulation tissues formed during the healing process. It is an excellent hemostatic, promoting hemostasis by facilitating the aggregation of platelets during coagulation cascade. Other advantages of using collagen as a dressing material are: it is non-immunogenic, nonpyrogenic and has minimal allergic potential. Commercially, the collagen materials are available in three forms: tape (CollaTape; Zimmer Dental, Carlsbad, CA, USA), cote (CollaCote, Zimmer Dental, Carlsbad, CA, USA) and plug (CollaPlug; Zimmer Dental, Carlsbad, CA, USA). The collagen in these dressing materials has been derived from bovine Achilles tendon consisting of collagen Type I. It is a completely resorbable dressing that is used to ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Reso-Pac®:
Reso-Pac® (Hager & Werken GmbH & Co. KG, Duisburg, Germany) is easy to mix periodontal dressing. It does not require removal because it dissolves in the mouth. The material is squeezed out of the tube and is taken on a moist glove or moist spatula. It is hydrophilic in nature and when put in the oral cavity, it takes a gel-like consistency due to the presence of saliva. This dressing remains in place for up to 30 hours.
Cyanoacrylates:
Cyanoacrylate alkyls were first isolated by A E Ardis in 1949 42. Coover et al. (1959) 43 who suggested their use as tissue adhesive material. Cyanoacrylates have a chemical formula, H2C = C(CN)COOR, where R- can be substituted for any alkyl group, ranging from methyl to decyl. This material was introduced to dentistry by Dr. S N Bhaskar (1996) 44, who advocated its use as a dressing as well as suture replacement material. It is a liquid which can be applied directly or sprayed over the wound surface. The material sets when it comes in contact with the moisture. Cyanoacrylate is a good hemostatic and stops post-operative bleeding quickly. Another important advantage of this material is ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
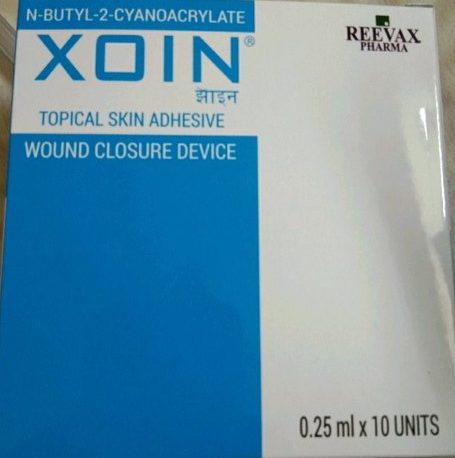
XOIN® (Reevax Pharma Private Limited, Hyderabad, India) periodontal dressing material consists of N-butyl cyanoacrylate which is an effective tissue adhesive, hemostatic and bacteriostatic. Other commercially available cyanoacrylate periodontal dressing material are PeriAcryl®, which is a blend of N-butyl and 2-octyl cyanoacrylate and Histoacryl® (B. Braun Biosurgicals, Germany).
Controversy regarding the use of periodontal dressings
Whether to use or not to use a periodontal dressing after periodontal flap surgery has been a topic of discussion for years. As already stated, it was Ward (1923) 45 who advocated the use of periodontal dressing following periodontal surgery to avoid pain, infection, root sensitivity and to prevent the formation of caseous deposits upon the root surfaces. Orban (1941) 46 demonstrated that better healing occurred if the periodontal dressing is changed every 2 to 4 days for 10 to 14 days post-operatively. Similar findings were reported by Bernier and Kaplan (1947) 47 who reported that the use of a dressing facilitates the healing process. Linghorne (1949) 48 reported that zinc oxide eugenol periodontal dressing has bacteriostatic properties and also has local anesthetic action. Greensmith and Wade (1976) 49 in split-mouth study evaluated the effect of applying a surgical dressing versus without applying a dressing after reverse bevel flap procedures. They reported that application of periodontal dressing resulted in a statistically slightly better healing.
On the other hand, other researchers did not support the placement of periodontal dressing following periodontal surgery. It was Waerhaug (1955) 50 who first reported that application of a surgical dressing did not influence the final result of healing. Similar findings were reported by Löe and Silness (1961) 51 who stated that exposed tissues will heal irrespective of the application of a dressing material. Baer et al. (1969) 37, in experimental studies, observed that periodontal dressings following periodontal surgery did not exert any perceptible influence on the final healing. Jones et al. (1979) 33 in a split-mouth study where internal beveled full-thickness, apically positioned flaps with osseous recontouring were performed in 20 quadrants, evaluated ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Presently, most of the clinicians believe that in cases where adequate primary closure of the flap margins has been achieved, there is no requirement for the placement of periodontal dressing. In cases where the primary closure of flaps is not adequate or cases where the protection of the operated area is required (e.g. mucogingival surgeries), placement of periodontal dressing has been recommended.
Post-operative instructions to the patient
The post-operative instructions should be given to the patient verbally and in written, so that any complication related to the surgical procedure can be avoided. Following instructions are given to the patient before he/she is discharged,
- The patient should take analgesics and antibiotics as prescribed by the clinician. Ibuprofen 600 to 800 mg can be started preoperatively and should be continued 1 tablet every 8 hours for 24 to 48 hours is quite effective in controlling post-operative pain. Amoxicillin 500 mg every 8 hours for one week can be prescribed to provide antibiotic cover during initial healing.
- The patient should be asked to apply ice intermittently for alternating 20 minutes on and 20 minutes off, on the face over the operated area on the first day after surgery.
- If surgery has been done on one quadrant, the patient should be asked to chew on the non-operated side.
- The patient is asked to take only semi-solid food to avoid any injury to the operated area.
- The patient should be advised not to take carbonated drinks after the surgery, as it may hamper the healing process by interfering with clot formation.
- Teeth which have not been involved in the surgery should be brushed and flossed as previously instructed. Teeth in the operated area should be gently brushed and flossed only after 24 hours. A small amount of bleeding is expected, but the removal of bacterial plaque is essential because it enhances healing.
- A small amount of bleeding or oozing may occur after the surgery, which may continue for one or two days. However, if the bleeding is excessive or continuous, the patient should be asked to place a moistened gauze pad or clean cloth against the bleeding area and put a constant pressure on the bleeding area for 10-15 minutes. The procedure may be repeated, if necessary. If bleeding does not stop, a visit to the dental office is required.
- In the case where resorbable membrane has been used for GTR or Emdogain® has been used to achieve regeneration, the patient should not brush or floss in the operated area(s) for 4-6 weeks after surgery.
- To enhance plaque control, the patient may be advised to use mouth rinses as follows,
- Warm salt water (¼ tsp. salt per cup of warm water) can be used 24 hours after the surgery with a frequency of rinsing 2-3 times a day.
Chlorhexidine mouthwash can be used 24 hours (the next day) after the surgery. The mouthwash should be used by swishing with ½ oz. of the solution for 30 seconds after breakfast and before bedtime. As the ingredients of toothpaste interfere with the activity of chlorhexidine, a gap of 30 minutes should be maintained between toothbrushing and mouth rinsing. - In case periodontal dressing has been placed, the patient should be told about its protective function and should be asked to protect it from breaking off. If a small piece of dressing breaks off, there is no need to be concerned. However, if a large piece of the dressing breaks off, then dental office should be consulted.
- The patient should visit the dental office after one week or 10 days whenever he/she has been given an appointment for dressing and/or suture removal.
Conclusion
The use of periodontal dressing after periodontal surgical procedures is a routine procedure. However, presently it is recommended that periodontal dressing should be used only in those cases where healing with secondary intention is anticipated. The type of periodontal dressing should be selected according to the indications for a particular case. In the upcoming articles, we shall read about various periodontal surgical procedures.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

