Introduction
With the introduction and advancements in the surgical periodontal pocket therapy, our understanding regarding the type of bone defects and healing following flap surgeries improved dramatically. 1970’s and 80’s may be regarded as two decades when our basic understanding regarding surgical periodontal therapy improved and it was demonstrated that lost periodontal tissue can be regenerated. Many researchers working on the outcomes of non-surgical and surgical periodontal therapy, published their research work during this period.
The future of periodontal treatment resides in the regeneration of lost periodontal structures. So, it is essential to understand the historical aspect of periodontal regenerative therapy. In the following discussion, we shall study in detail, how regenerative periodontal therapy came into the picture, advancements that took place in this field over the years and where we stand now.
Important terminologies
It is important to clearly understand the following terms before we go ahead with our main discussion,
Regeneration:
Regeneration is defined as the reproduction or reconstruction of the lost or injured part in such a way that the architecture and function of the lost or injured tissues are completely restored 1. From the periodontal point of view, it means, formation and …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
New attachment:
It describes new cementum formation with inserting collagen fibers on the root previously denuded of its periodontal ligament. Periodontal regeneration is differentiated from new attachment in that the former must include new bone formation 2.
Reattachment:
It refers to repair in areas of the root not previously exposed to the pocket, such as after surgical detachment of the tissues or following traumatic tears in the cementum, tooth fractures, or the treatment of periapical lesions 3. In 1948, Orban 4 in his classical article “Pocket Elimination or Reattachment” defines reattachment as the establishment of an organic connection between connective tissue and cementum in the area of gingival or periodontal pocket.
Repair:
It is the biological process by which continuity of disrupted tissue is restored by new tissues which do not replicate the structure and function of the lost tissue 3. In simple words, repair can be described as healing by the formation of scar tissue. Repair can be mediated by the formation of long junctional epithelium and bone fill. Root resorption, ankylosis, and fibrous adhesion can also be seen.
Bone fill:
It is defined as the clinical restoration of the bone tissue in a previously treated periodontal defect. The presence of bone fill does not mean that new attachment has taken place (which can only be demonstrated by histological evaluation). It just indicates the presence of new bone in the surgically treated periodontal bony defect.
Epithelial adaptation:
It is the close apposition of gingival epithelium to the tooth without complete obliteration of pocket.
Historical aspect of periodontal regenerative therapy
How it started?
The initial research work clearly demonstrated the bacterial etiology of periodontitis. It was also clear that periodontitis leads to the destruction of supporting bone and creates periodontal bone defects. The detailed description of periodontal bone destruction in periodontitis is available in “Patterns of bone destruction in periodontal diseases”. So, based on these factors, periodontal treatment was focused on achieving two objectives: the primary objective was to eliminate bacterial plaque and secondary objective was to eliminate the anatomical defects produced by periodontitis. There are two ways to eliminate these bony defects, both of which are surgical:
Resective osseous surgery: Wherein the bony architecture is modified by removal or reshaping of supporting bone. Details are available in “Osseous resective surgeries”.
Regenerative surgical procedures: Wherein there is an attempt to regenerate new bone and periodontal ligament, thereby coronally displacing the attachment apparatus and thus the gingival margin.
To evaluate the outcome of surgical therapy various procedures were employed which included pre and post-surgical probing measurements, examination of radiographs, re-entry procedures and histological examination 5. The periodontal probing procedure is widely used for the assessment of pre- and post-operative pocket depth. This procedure can give us pocket depth measurements, but cannot accurately determine the level of connective tissue attachment on the tooth surface which is required to determine whether regeneration has taken place or not. Similarly, radiographs can demonstrate the changes in pre and post-operative bone levels but cannot determine whether there is any periodontal ligament present between the bone and tooth surface which is indicative of the new attachment. Surgical re-entry in the operated area has been used to determine the increase in bone level as compared to its original level during the surgery. It can also demonstrate an increase in bone volume but cannot determine whether …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Where the progenitor cell population resides?
For periodontal regeneration, we need to regenerate new periodontal ligament, alveolar bone, and cementum and more importantly, this re-formation of the tissue is expected on previously diseased root surface. But, can regeneration occur on previously diseased root surface? Where does the progenitor cell population reside, which is expected to do regeneration? Is the progenitor cell population derived from alveolar bone, gingival connective tissue or periodontal ligament? These were the basic questions in the mind of researchers at that point in time which needed to be answered to initiate basic research on periodontal regeneration.
Let us try to find out the answers to these questions by discussing some studies which were designed to address these questions,
Whether new attachment depends on normal/diseased root surface or normal/reduced periodontium?
Polson and Caton (1982) 9 designed an experimental study on rhesus monkeys. Experimental periodontitis was induced around single maxillary central incisor. Then, both the maxillary central incisors were extracted and autotrans-planted. Tooth with normal root surface was transplanted in the reduced periodontium and tooth with the diseased root surface (involved with periodontitis) was transplanted in the normal periodontium. The teeth were splinted and left in place for 40 days. After 40 days, radiographic evaluation showed a crestal bone loss around periodontitis affect tooth. Histological evaluation of teeth demonstrated that normal teeth, which were transplanted in reduced periodontium demonstrated a …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
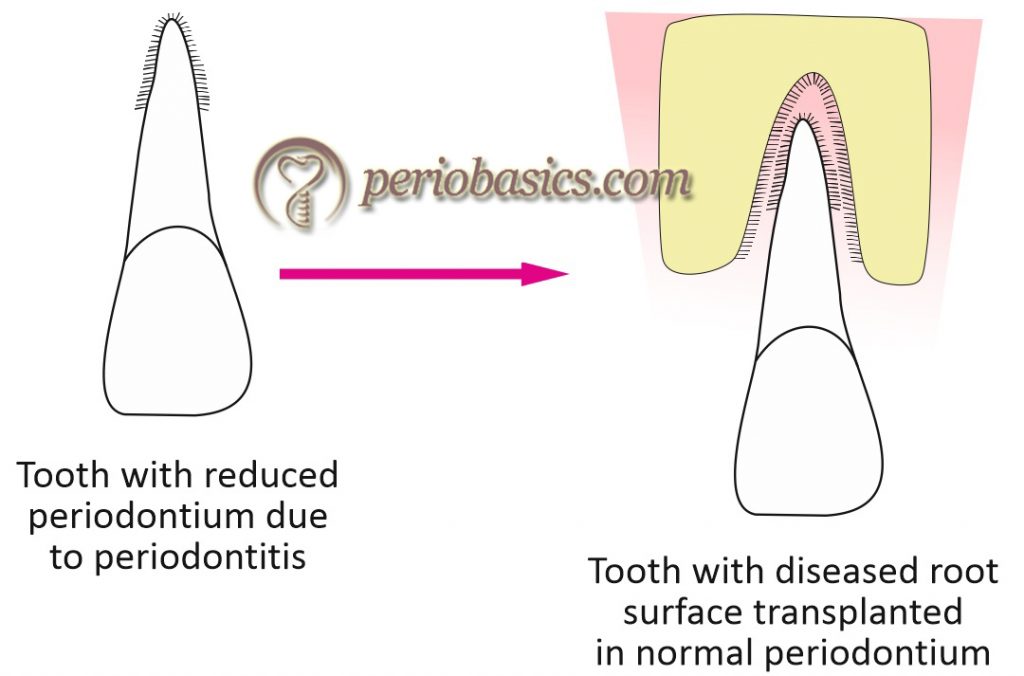

So, the results of this study demonstrated that it is the exposed root surface and not lack of periodontium which inhibits a new connective tissue attachment.
Whether the presence of alveolar bone has any influence on new attachment?
Lindhe et al. (1982) 10 addressed the same question in an experimental study done on monkeys. In this study, maxillary and mandibular central incisors were extracted and placed in their own socket in four situations which included: non-root planed teeth placed in sockets with normal bone height, non-root planed teeth placed in sockets with reduced bone height, root planed teeth placed in sockets with normal bone height and root planed teeth placed in sockets with reduced bone height. After 6 months, when the histological examination was done, it was found that …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
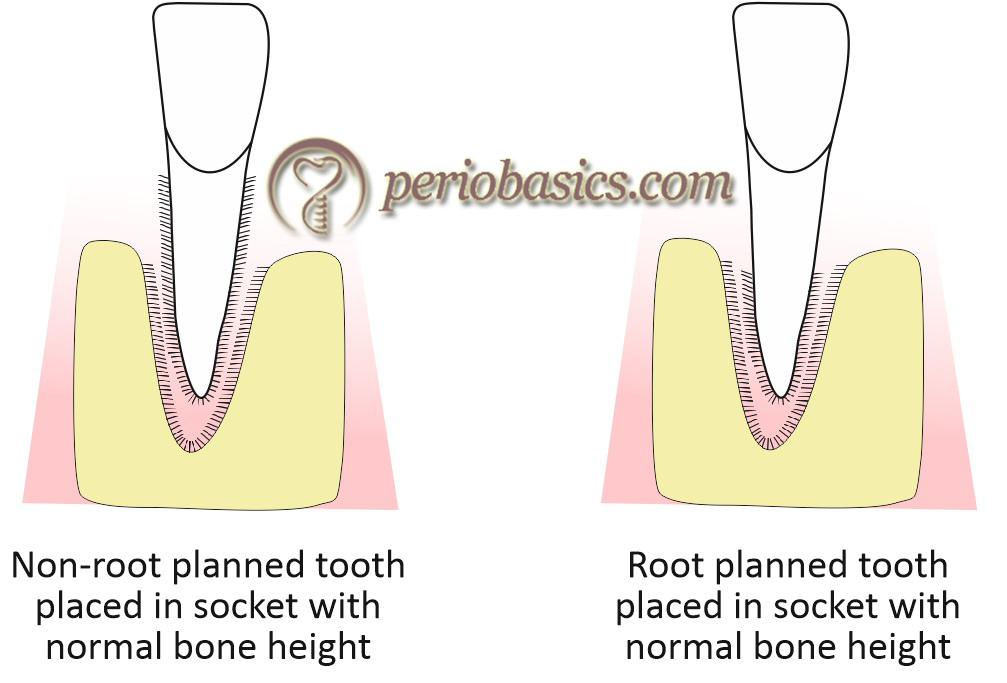
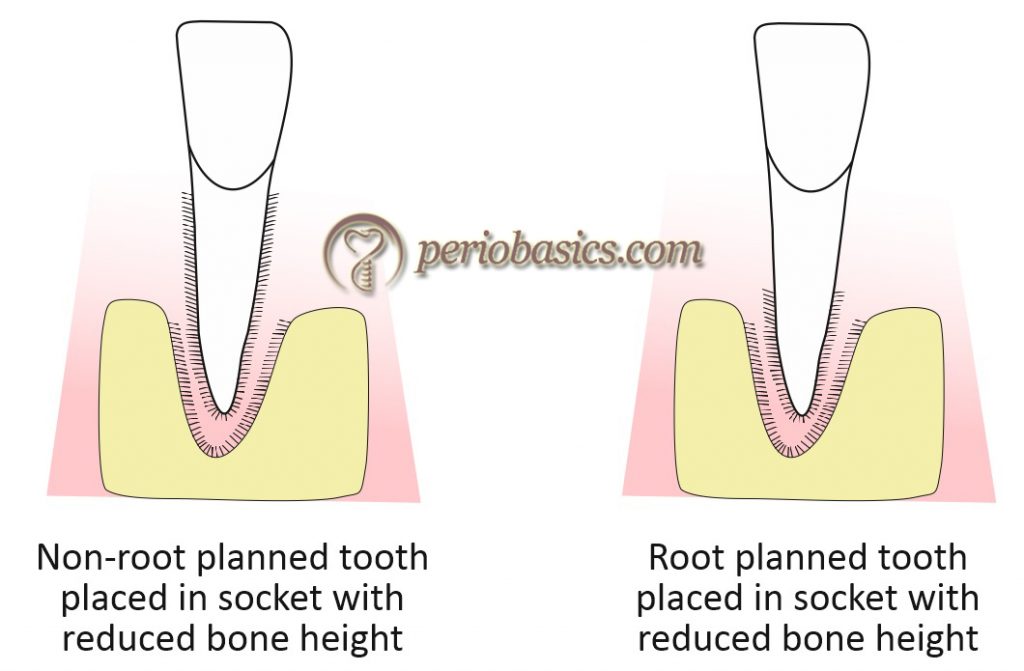
So, it was concluded that the establishment of connective tissue attachment was not related to the presence of bone.
During the same time period, Melcher (1976) 11 in a review described that for periodontal regeneration the progenitor cell population can be derived from four sources,
Epithelial cells.
Cells derived from gingival connective tissue.
Cells derived from alveolar bone.
Cells derived from periodontal ligament.
This observation focused the research work on these four sources of cells. Various methodologies were adopted to find out the cells responsible for periodontal regeneration.
Whether the progenitor cell population is derived from the alveolar bone?
Karring et al. (1980) 12 carried out an experimental study on dogs where they extracted the roots of periodontitis-affected teeth and placed them in surgically created sockets in edentulous areas of the dog. These sockets were prepared in such a way that they prevented migration of epithelium and bacterial infection during wound healing. After a healing interval of 3 months, histological examination was done. It was found that in apical areas where periodontal ligament was retained during implantation, it was again re-established. In coronal areas of root which were affected by periodontitis and were scaled and root planed ankylosis or root resorption resulted.
So, the results of the study revealed that the cells derived from bone lack potential to produce new attachment.
Whether the progenitor cell population is derived from gingival connective tissue?
Nyman et al. (1980) 13 in this study followed the same study design as above, but the bone cavities were prepared on the buccal surface of the jaw and root specimens were placed which were subsequently covered by the flap. In this way half of the root surface was in contact with connective tissue and half the surface was in contact with the bone. After a healing period of 3 months, histological examination was done. It was found that in apical areas of the root where …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
So, the results of the study revealed that connective tissue lacks the cells, which have a potential to produce new attachment.
Whether the progenitor cell population is derived from periodontal ligament?
Karring et al. (1985) 14 in an animal experiment, examined whether a new connective tissue attachment forms on previously periodontitis-involved roots when reduced but healthy periodontal ligament tissue persists following periodontal treatment. The migration of epithelial cells was prevented into the healing site. After producing experimental periodontitis, when 50% of the bone support of teeth was lost, the periodontal treatment was done to remove pocket epithelium and granulation tissue. The crowns were resected and roots were covered with a mucosal flap. The animals were sacrificed after 3 months of healing and histological examination was done. It was found that new cementum with inserting collagen fibers had formed in the apical portion of the previously exposed root surfaces. It was in continuity with the original cementum layer apical …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
So, the results of the study demonstrated that new attachment was formed by the coronal migration of the cells originating from the periodontal ligament and proliferation of epithelial cells should not be allowed on the root surface to achieve new connective tissue attachment.
Nyman et al. (1982) 15, in an experiment on non-human primates, created fenestration defects on the buccal aspect of maxillary lateral incisors and mandibular canines. A millipore filter was placed to cover the fenestration defects with the aim of preventing gingival connective tissue from contacting the root surface. New cementum with a …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
The results of the study clearly showed new connective tissue attachment from cells originating from periodontal ligament.
Warrer et al. (1993) 17 did a study on dental implants, where the implants were placed in contact with the retained root tips of the teeth. The periodontal ligament around these retained roots served as a source of cells during healing around implants. The results of the study demonstrated the formation of a distinct layer of cementum on the implant surface with inserting collagen fibers which were most of the times oriented perpendicularly to the surface, embedded in the opposite bone.
The results of the study clarified that cells originating from periodontal ligament have the potential to make the new connective tissue attachment.
Later on, many studies confirmed that it is the cells from the periodontal ligament that are responsible for the re-establishment of periodontal attachment 18, 19. In addition, it was also shown that the exclusion of the junctional epithelial cells from the treated root surface in the early stages of periodontal wound healing …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Concept of guided tissue regeneration
From the above studies and many other studies, it became clear that cells from periodontal ligament should be allowed to proliferate in order to achieve new connective tissue attachment. When healing takes place, every tissue is given equal opportunity to proliferate and among all epithelium grows at the fastest rate. Migration of the junctional epithelium into periodontal defects and the formation of sub-gingival plaque are thought to be the primary impediments to the re-establishment of normal connective tissue attachment 21. So, there should be some kind of barrier which should prevent epithelial and other cells from gingival connective tissue to enter the site of healing to facilitate regeneration by periodontal ligament cells.
Keeping all these factors in mind concept of guided tissue regeneration was given. The procedure involves placement of a barrier membrane which separates the exposed root surface and supporting alveolar bone from the gingival tissue. This barrier prevents the migration of junctional epithelial cells and gingival connective tissue cells from colonizing on the root surfaces and provides space for the selective re-population …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
The initial membranes used such as ePTFE were non-resorbable, so they had to be removed later on. With due course of time, resorbable membranes such as those made of glycolide and lactide polymers, collagen, etc. were introduced which did not require additional surgery for their removal. The detailed description of these is available in “Guided tissue regeneration”.
Root surface biomodification
The concept of root surface bio-modification is based on the fact that root surface plays an important role in the formation of new connective tissue attachment and modifications can be done on the root surface to further enhance new attachment. This technique has the ability to modify the root surface by “detoxifying the surface” 26.
The history of root surface biomodification can be traced back to Marshall (1833) 27, who presented a case of pocket eradication with “presumable clinical reattachment” after the use of aromatic sulphuric acid. Later, Stewart 28 in 1890’s recommended mechanical removal of calculus and cementum along with acid application. Work done by Urist brought acid demineralization of root surfaces under the limelight. In 1965, Urist 29 suggested that f …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
In 1973, Register 31 performed a systematically designed controlled study where the potential of demineralization to induce cementogenesis, osteogenesis, and new attachment was assessed. The results of the study showed that optimum cementogenesis and new connective tissue attachment occurred when roots were demineralized with citric acid at pH 1 for 2-3 minutes. Presently, various agents are used for root surface demineralization including citric acid, polyacrylic acid, fibronectin, laminin, tetracycline, doxycycline, ethylenediaminetetraacetic acid (EDTA) etc. A detailed description on this topic is available in chapter 69 “Root surface biomodification”.
Bone grafts
Another way of enhancing periodontal regeneration was putting a bone graft in osseous defects. The use of bone grafts in periodontal therapy can be traced back to the work of Hegedus (1923) 32. Beube and Silvers 33 in 1934 used boiled cow bone powder to successfully repair intrabony defects in humans. Anorganic bone (bovine bone from which the organic material is extracted by means of ethylenediamine) was used by Melcher 34 in 1962 in 187 bone defects which were …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Autogenous grafts have osteoinductive properties. Their application for periodontal bone defects can be traced back to Nabers and O’Leary (1965) 35, who used cortical bone chips as grafting material. Later on, Robinson 36 in 1969, and Jacobs and Rosenberg 37 in 1984 introduced the application of osseous coagulum and bone blend (Intra-oral bone obtained with high or low-speed round burs and mixed with blood). Intraoral cancellous bone and marrow grafts were used as autogenous grafts by various authors, including Hiatt and Schallhorn (1973) 38, Ross and Cohen (1968) 39, Soehren and Von Swol (1979) 40, Halliday (1969) 41 and Rosenberg (1971) 42. Extra-oral sites for autogenous graft harvesting have been suggested by many authors. Schallhorn (1968) 43 suggested either the anterior or the posterior iliac crest for graft harvesting.
The problems associated with autogenous bone graft harvesting, namely, morbidity accompanying a second surgical site and the need for a sufficient quantity of material to fill multiple defects, led to the development of allograft materials. Presently, three types of bone allografts are used clinically: fresh-frozen allograft, freeze-dried bone allograft (FDBA), demineralized freeze-dried bone allograft (DFDBA).
Initially, various researchers had their reservations regarding bone graft usage in periodontal defects. According to some, bone grafting materials will enhance regeneration of a new attachment apparatus 44. While others disapproved the usage of bone grafts in periodontal defects, saying that there was no evidence in human trials that clearly demonstrated new attachment 45.
The first field test study was initiated in 1972 in the United States in which 89 clinicians participated. FDBA was placed alone or in combination with autograft in bony defects. They were given the option of flap design, fill or overfill the defect, use of periodontal dressing, antibiotic regimen and whether to do perforations in the bone lining the defect. Surgical re-entry was …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Presently, we have a large database regarding applications of different types of bone grafts, their success rate and long-term results. A detailed description regarding bone grafts is available in “Bone grafts in periodontics”.
Application of growth factors in periodontal regeneration
Presently, we have sufficient scientific evidence which supports the important role of growth factors and other molecules in periodontal regeneration. Growth factors are proteins that may act locally or systemically to affect the growth and function of cells in several ways. The concept behind this therapy is to create an environment which is close to that present during embryonic and post-natal development. The signaling molecules that have been most intensively investigated in periodontal regeneration include bone morphogenetic proteins (BMPs, e.g. BMP-2, BMP-7, & BMP-12) 49-58, transforming growth factor (TGF)-β1 59, 60, platelet-derived growth factors (PDGFs, such as PDGF-BB) 61-64, insulin-like growth factor (IGF)-1 61, 65, 66, and basic fibroblast growth factor (b-FGF) 67-70. Detailed description on this topic is available in “Application of growth factors in periodontal regeneration”.
Conclusion
The aim of the above discussion was to give a brief idea to the readers, regarding where we started in the field of periodontal regeneration and where do we stand presently. With a clear understanding of the historical aspect of periodontal regeneration, now we can go ahead with the discussion of recent techniques, materials and other advances in this field. In the upcoming chapters, we shall study in detail various regenerative periodontal procedures.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

