Introduction
Peri-implantitis is a significant and increasingly recognized complication in the field of implant dentistry. As the global prevalence of dental implants rises, so does the occurrence of peri-implant diseases, with peri-implantitis being the most severe form. Characterized by inflammation in the peri-implant tissues and progressive bone loss around the implant, peri-implantitis poses a serious threat to the longevity of dental implants. Understanding its etiology, risk factors, pathogenesis, diagnosis, and treatment options is critical for clinicians to effectively prevent and manage this condition
Etiology of Peri-Implantitis
Peri-implantitis is a multifactorial disease, and its etiology involves a complex interplay of bacterial infection, host immune response, and mechanical factors.
Bacterial etiology of peri-implantitis
The pathogenesis of peri-implantitis is closely associated with the formation of a biofilm on the implant surface, which is composed of various microorganisms. Understanding the bacterial etiology of peri-implantitis is critical in developing effective prevention and treatment strategies. As stated earlier, formation of a biofilm is the initial step in the development of peri-implantitis. A biofilm is a structured community of bacteria embedded in a self-produced extracellular matrix that adheres to the surface of the implant. The biofilm protects the bacteria from the host’s immune response and antimicrobial agents, making the infection difficult to eradicate. Once established, the biofilm can trigger an inflammatory response in the peri-implant tissues, leading to tissue destruction. The bacterial communities associated with peri-implantitis are similar to those found in periodontitis, albeit with some differences in the microbial profile. The peri-implant environment, characterized by the presence of a titanium surface and a distinct micro-architecture, can influence the types of bacteria that colonize the area. Most common bacterial species associated with peri-implantitis include Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola, Aggregatibacter actinomycetemcomitans and Fusobacterium nucleatum. The interaction between the bacterial biofilm and the host immune response is a key factor in the progression of peri-implantitis. The host immune system responds to the presence of the biofilm by recruiting neutrophils, macrophages, and other immune cells to the site of infection. These cells release pro-inflammatory cytokines, such as interleukin-1β (IL-1β), tumor necrosis factor-alpha (TNF-α), and prostaglandin E2 (PGE2), which contribute to the inflammatory process and the activation of osteoclasts. Osteoclasts, the cells responsible for bone resorption, are activated in response to the inflammatory mediators produced during peri-implantitis. This leads to the destruction of the alveolar bone supporting the implant, which is a hallmark of peri-implantitis.
Differences between peri-implantitis and periodontitis microbiomes
While the microbiomes of peri-implantitis and periodontitis share similarities, there are distinct differences due to the unique environment around dental implants. For example,
Titanium Surface: The titanium surface of implants may select for specific bacterial species that can adhere more effectively to metal surfaces compared to natural tooth surfaces.
Peri-Implant Pocket Environment: The peri-implant pocket is typically deeper and less vascularized than the periodontal pocket, which may influence the types of bacteria that can thrive in this environment.
Differences in Host Response: The inflammatory response in peri-implantitis may differ from that in periodontitis, potentially affecting the composition of the microbial community.
Review of literature on microbial etiology of peri-implantitis
Numerous studies have explored the microbial etiology of peri-implantitis to better understand the bacterial species involved, their virulence factors, and how they contribute to the disease’s progression. Mombelli et al. (1987) in their landmark study were first to characterize the microbial flora associated with dental implants. The authors found that failing implants had a significantly higher proportion of anaerobic bacteria, particularly black-pigmented Bacteroides, which include P. gingivalis and Prevotella intermedia. These findings suggested that the microbial shift towards a more pathogenic flora is associated with implant failure. In another study, Lang et al. (1992) investigated the microbial flora around failing implants with those around healthy implants. The study found that failing implants had a higher prevalence of periodontal pathogens, such as Porphyromonas gingivalis and Prevotella intermedia, indicating that these bacteria play a role in peri-implantitis similar to their role in periodontitis. Leonhardt and colleagues (1999) analyzed the microbial profiles of implants with peri-implantitis and found that anaerobic Gram-negative bacteria were predominant. The study identified Porphyromonas gingivalis, Tannerella forsythia, and Fusobacterium nucleatum as key pathogens associated with peri-implantitis. This study reinforced the idea that peri-implantitis shares a similar microbial profile with chronic periodontitis.
Shibli et al. (2008) in their study titled, “Microbiologic and immunologic aspects of peri-implant health and disease” compared the microbial profiles of healthy implants, implants with peri-implant mucositis, and those with peri-implantitis. The authors found that peri-implantitis sites had a higher prevalence of pathogenic bacteria, including P. gingivalis, T. forsythia, and Treponema denticola. The study also highlighted the importance of the host immune response in modulating the progression of peri-implantitis. Dabdoub et al. (2013), using high-throughput sequencing, provided a comprehensive analysis of the bacterial microbiome in peri-implantitis. The authors found that peri-implantitis lesions harbored a more diverse and complex bacterial community compared to healthy implants. Key pathogens included P. gingivalis, F. nucleatum, and A. actinomycetemcomitans. This study emphasized the role of microbial diversity and dysbiosis in the development of peri-implantitis. In the same year, Koyanagi et al. (2013) compared the microbial profiles of peri-implantitis and periodontitis using advanced molecular techniques. The authors found significant similarities between the two conditions, particularly in the presence of red complex bacteria (P. gingivalis, T. forsythia, T. denticola). However, certain species were more prevalent in peri-implantitis, such as Staphylococcus aureus, suggesting that implants may harbor a unique microbial environment.
In a consensus report, Heitz-Mayfield et al. (2014) summarized the current understanding of the microbial etiology of peri-implantitis, based on the findings of numerous studies. The report emphasized the role of bacterial biofilms in the pathogenesis of peri-implantitis and identified key pathogens, including P. gingivalis, T. forsythia, and A. actinomycetemcomitans. The report also called for more research into the role of emerging pathogens and the influence of implant surface characteristics on microbial colonization. In another study, Maruyama et al. (2014) used pyrosequencing to analyze the subgingival bacterial communities in peri-implantitis and periodontitis. The findings revealed that peri-implantitis sites had a distinct bacterial community compared to periodontitis, with a higher prevalence of opportunistic pathogens, such as Staphylococcus spp. and Pseudomonas spp. The study suggested that the unique environment around implants may select for different bacterial species, contributing to the pathogenesis of peri-implantitis. In a systematic review, Ramanauskaite et al. (2016) synthesized the findings from various studies on the microbial etiology of peri-implantitis. The review confirmed that peri-implantitis is primarily associated with anaerobic Gram-negative bacteria, with P. gingivalis, T. forsythia, and F. nucleatum being the most consistently implicated species. The review also highlighted the role of systemic factors, such as diabetes and smoking, in influencing the microbial composition and the risk of peri-implantitis.
In a randomized clinical trial, Renvert et al. (2017) investigated the effects of different treatment modalities on the microbiota of peri-implantitis sites. The study found that while non-surgical treatments could reduce the bacterial load, certain pathogens, such as P. gingivalis and T. forsythia, persisted even after treatment. Surgical intervention was more effective in reducing these pathogens, but complete eradication was still challenging. Berglundh et al. (2018) compared the microbial composition of peri-implantitis and periodontitis lesions using high-throughput sequencing. The authors found that while both conditions shared many bacterial species, peri-implantitis lesions were characterized by a higher prevalence of Staphylococcus spp. and Enterococcus spp., which are not typically associated with periodontitis. The study suggested that the implant surface and peri-implant environment might select for different microbial communities, contributing to the distinct pathogenesis of peri-implantitis. In a cross-sectional study, Bramanti et al. (2019) used quantitative PCR to analyze the microbial profiles of patients with and without peri-implantitis. The results showed a higher concentration of red complex bacteria (P. gingivalis, T. forsythia, and T. denticola) in peri-implantitis sites. Additionally, the study identified Candida spp. as a significant co-pathogen in peri-implantitis, highlighting the potential role of fungal infections in the disease’s etiology. Monje et al. (2019) in a case-control study, compared the submucosal biofilm of peri-implantitis lesions with periodontitis lesions. The authors found that peri-implantitis lesions had a more diverse microbial community, with higher levels of opportunistic pathogens, such as Escherichia coli and Klebsiella pneumoniae. The study emphasized the need for targeted antimicrobial therapies that consider the unique microbial profile of peri-implantitis. Sanz-Martín et al. (2019) in a systematic review and meta-analysis synthesized data from various studies on the peri-implant microbiome. The review confirmed that peri-implantitis is associated with a dysbiotic microbial community dominated by anaerobic bacteria, including P. gingivalis, T. forsythia, and F. nucleatum. The study also highlighted the emerging role of Staphylococcus spp. and other opportunistic pathogens in the etiology of peri-implantitis, suggesting that these bacteria may be potential targets for new treatment strategies.
Koyanagi et al. (2020) used 16S rRNA gene sequencing to profile the bacterial communities associated with peri-implantitis. The authors identified a complex microbiome with a high diversity of bacterial species, including Porphyromonas gingivalis, Fusobacterium nucleatum, and Treponema denticola. Interestingly, the study also found a significant presence of non-traditional periodontal pathogens, such as Staphylococcus spp. and Pseudomonas spp., suggesting that peri-implantitis may involve a broader range of microbial species than previously thought. Tsigarida et al. (2020) explored the effect of different implant loading protocols on the microbial colonization of peri-implant tissues. The authors found that early loading implants were more prone to colonization by pathogenic bacteria, such as P. gingivalis and F. nucleatum, compared to delayed loading implants. The study suggested that the timing of implant loading could influence the microbial etiology of peri-implantitis and recommended careful monitoring of patients with early loaded implants. Heitz-Mayfield et al. (2020) in a systematic review focused on the antibiotic resistance profiles of bacteria isolated from peri-implantitis lesions. The authors found that many peri-implantitis-associated bacteria, particularly P. gingivalis and A. actinomycetemcomitans, exhibited resistance to commonly used antibiotics, such as metronidazole and amoxicillin. The study underscored the importance of microbiological testing and the judicious use of antibiotics in the management of peri-implantitis. Renvert et al. (2021) in a longitudinal study followed patients with peri-implantitis over several years to track the changes in the microbial community associated with disease progression. The authors observed that peri-implantitis progression was marked by an increase in the abundance of specific pathogens, such as P. gingivalis, T. forsythia, and Prevotella nigrescens. The study highlighted the dynamic nature of the peri-implant microbiome and the potential for certain bacteria to act as biomarkers for disease progression.
Qiu et al. (2022) used 16S rRNA gene sequencing to compare the microbial profiles of peri-implantitis and periodontitis. The findings indicated that while both conditions share common pathogens, such as P. gingivalis and T. forsythia, peri-implantitis lesions exhibited a unique microbial signature with a higher abundance of Staphylococcus aureus and Enterococcus faecalis. The study suggested that these differences could be linked to the distinct tissue environment around implants. Zhang et al. (2022) in a systematic review and meta-analysis focused on the impact of implant surface characteristics on the microbial profile associated with peri-implantitis. The study found that rough surface implants were more prone to colonization by pathogenic bacteria, such as P. gingivalis and T. denticola, compared to smooth surface implants. The findings suggested that implant surface properties could influence the development and progression of peri-implantitis by affecting microbial adhesion and biofilm formation. Costa et al. (2023) in a recent study used next-generation sequencing to explore the microbial diversity in peri-implantitis lesions. The authors found a highly diverse microbiome, with the presence of both traditional periodontal pathogens and non-oral bacteria, including Pseudomonas aeruginosa and Escherichia coli. The study highlighted the complexity of the peri-implant microbiome and its potential implications for disease management and treatment strategies. Teng et al. (2023) in their study explored the role of fungal species in the microbiome of peri-implantitis lesions using metagenomic analysis. The authors found that fungi, particularly Candida albicans, were prevalent in peri-implantitis sites and often co-existed with bacterial pathogens like P. gingivalis and F. nucleatum. The study highlighted the potential role of fungal-bacterial interactions in the pathogenesis of peri-implantitis and the need for antifungal treatments in certain cases. (References are available in the book)
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Outcome of research on microbial etiology of peri-implantitis
The studies on the microbial etiology of peri-implantitis have provided significant insights into the complex and diverse microbial communities associated with the condition. The key findings may be summarized as follows,
Microbial diversity and complexity
Studies using advanced sequencing techniques like shotgun metagenomics and next-generation sequencing have revealed a highly diverse microbiome in peri-implantitis lesions. Traditional periodontal pathogens, such as Porphyromonas gingivalis, Treponema denticola, and Fusobacterium nucleatum, are consistently identified as major contributors to peri-implantitis. However, the presence of non-oral and opportunistic pathogens, such as Staphylococcus aureus, Pseudomonas aeruginosa, and Escherichia coli, has also been noted, suggesting that peri-implantitis involves a broader range of microbial species than previously understood.
Impact of implant surface characteristics
The surface characteristics of dental implants appear to influence the microbial composition associated with peri-implantitis. Rough surface implants are more prone to colonization by pathogenic bacteria compared to smooth surface implants. This finding suggests that the physical properties of implants can play a critical role in the development and progression of peri-implantitis by affecting microbial adhesion and biofilm formation.
Microbial changes post-treatment
Longitudinal studies have shown that while non-surgical treatments can reduce the overall bacterial load in peri-implantitis lesions, key pathogens such as P. gingivalis and T. forsythia often persist. This persistence of pathogens highlights the challenges of completely eradicating the microbial biofilm and suggests that adjunctive therapies may be necessary for effective treatment.
Influence of systemic conditions
Research on diabetic patients with peri-implantitis has shown that diabetes may exacerbate microbial dysbiosis, leading to a more pathogenic microbial community. This finding underscores the importance of considering systemic health conditions when assessing and treating peri-implantitis.
Role of fungal species
Emerging research has highlighted the potential role of fungal species, particularly Candida albicans, in the pathogenesis of peri-implantitis. Fungal-bacterial interactions in the biofilm could contribute to the disease’s progression, suggesting the need for antifungal treatments in certain cases.
Antibiotic resistance and treatment challenges
Studies have raised concerns about the impact of systemic antibiotic use on the peri-implant microbiome. While antibiotics can temporarily reduce the abundance of key pathogens, they may also lead to a decrease in beneficial commensal bacteria, potentially resulting in microbial imbalances and recurrence of the disease. These findings call for more selective and targeted antibiotic use and the exploration of alternative therapeutic approaches.
Peri-implant pocket depth
Deeper peri-implant pockets have been associated with a more pathogenic microbial community. This relationship suggests that pocket depth is a critical factor in determining the severity of peri-implantitis and the associated microbial load, with deeper pockets harboring higher levels of harmful bacteria.
Host immune response and peri-implantitis
The host immune response plays a crucial role in the development and progression of peri-implantitis, which is an inflammatory condition affecting the tissues surrounding dental implants. While microbial infection is a primary trigger, the host’s immune response significantly influences the severity and outcome of the disease. Initial Defense Mechanisms: The innate immune system provides the first line of defense against pathogens that colonize the implant surface. When bacteria form a biofilm around the implant, immune cells such as neutrophils, macrophages, and dendritic cells are recruited to the site. These cells recognize microbial components through pattern recognition receptors (PRRs) like Toll-like receptors (TLRs). The activation of PRRs triggers the release of pro-inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α) and chemokines, which amplify the inflammatory response. While this is intended to eliminate the infection, excessive or dysregulated cytokine production can lead to tissue damage and bone resorption.
The adaptive immune response is characterized by the activation of T and B lymphocytes. T-helper cells (Th1 and Th17) are particularly important in peri-implantitis. Th1 cells produce IFN-γ, which activates macrophages, while Th17 cells produce IL-17, promoting the recruitment of neutrophils and further inflammation. B cells produce antibodies against bacterial antigens, but in peri-implantitis, this response may contribute to chronic inflammation rather than resolution of the infection. Under normal conditions, regulatory T cells help to control excessive immune responses and prevent tissue damage. In peri-implantitis, a failure in immune regulation, possibly due to inadequate Treg function, may lead to uncontrolled inflammation and disease progression.
Immune cells release MMPs, which degrade extracellular matrix components, including collagen. This breakdown of tissue integrity contributes to the destruction of the peri-implant mucosa and bone. The cytokines released during the immune response, particularly RANKL (Receptor Activator of Nuclear Factor Kappa-B Ligand), promote the differentiation and activation of osteoclasts, leading to bone resorption. This process is a hallmark of peri-implantitis and can result in implant failure if not controlled. In some cases, the immune response fails to ……….Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…….
Certain individuals may have a genetic predisposition to an exaggerated immune response, making them more susceptible to peri-implantitis. For example, polymorphisms in genes encoding cytokines like IL-1β or TNF-α can influence the intensity of the inflammatory response. Conditions such as diabetes, smoking, and osteoporosis can exacerbate the immune response in peri-implant tissues. These factors may impair the immune system’s ability to control infection and enhance the inflammatory response, leading to greater tissue destruction.

Review of literature on host response and peri-implantitis
Berglundh et al. (2011) in a landmark study, examined the host response in peri-implantitis, focusing on the cellular and molecular mechanisms involved in the disease. The authors described how the immune response to bacterial biofilms around implants leads to the release of inflammatory mediators, such as cytokines and matrix metalloproteinases (MMPs), which contribute to tissue destruction and bone loss. The study emphasized the importance of understanding these mechanisms for developing targeted therapeutic strategies. Mombelli et al. (2012) in a review focused on the immune response to the bacterial biofilm in peri-implantitis. The authors discussed the role of both innate and adaptive immunity in recognizing and responding to biofilm-associated bacteria. They emphasized the importance of immune cell activation, cytokine production, and the release of tissue-destructive enzymes in the progression of peri-implantitis. In another review, Zitzmann et al. (2014) provided insights into the host response to peri-implant infections, with a focus on identifying risk factors and potential therapeutic approaches. The authors discussed how genetic predispositions, systemic health conditions, and local factors (such as implant design) influence the host response and the development of peri-implantitis. They also highlighted the importance of personalized treatment strategies based on an individual’s immune profile. In another narrative review, Renvert and Quirynen (2015) discussed various risk indicators for peri-implantitis, including the host immune response. The authors noted that genetic factors, such as polymorphisms in cytokine genes, can influence an individual’s susceptibility to peri-implantitis. The review also explored the role of systemic conditions, like diabetes, in modulating the host response and increasing the risk of peri-implantitis.(References are available in the book)
Kotsakis et al. (2017) in a study explored the dual role of the host immune response in peri-implant inflammation. While the immune system is essential for defending against bacterial infection, an exaggerated or dysregulated immune response can lead to tissue damage and bone resorption. The authors discussed the potential for therapeutic interventions that modulate the immune response to prevent or treat peri-implantitis. Salvi et al. (2017) in another study, provided a comprehensive overview of the host immune response in peri-implant mucosa. It highlighted the similarities and differences between peri-implantitis and periodontitis, particularly in the expression of cytokines and the inflammatory response. The study also emphasized the role of the innate immune system in recognizing pathogens through Toll-like receptors (TLRs) and the subsequent activation of pro-inflammatory pathways. Schwarz et al. (2018) in a systematic review evaluated the impact of different implant-abutment connection designs on the peri-implant immune response. The findings suggested that certain designs could minimize bacterial colonization and reduce the inflammatory response, thereby potentially lowering the risk of peri-implantitis. The review highlighted the importance of considering implant design in managing the host immune response.
Wang et al. (2019) in a pilot study investigated the role of microRNAs in regulating the host immune response in peri-implantitis. The authors found that specific microRNAs were differentially expressed in peri-implantitis tissues compared to healthy peri-implant mucosa. These microRNAs were associated with the regulation of inflammation and immune cell function, suggesting a potential role in the pathogenesis of peri-implantitis. Kim et al. (2021) investigated how systemic conditions like diabetes and smoking influence the host immune response in peri-implantitis. The authors found that both conditions exacerbate the inflammatory response, leading to increased cytokine levels (e.g., IL-6, TNF-α) and greater tissue destruction around implants. The study emphasized the need for managing these systemic conditions to mitigate their impact on peri-implant health. Huang et al. (2022) examined the role of macrophage polarization in peri-implantitis. The authors found an increased presence of M1 pro-inflammatory macrophages in peri-implantitis tissues compared to healthy controls. M1 macrophages were associated with higher levels of inflammatory cytokines and tissue destruction, while M2 macrophages, which are typically involved in tissue repair, were less prevalent. The study suggested that modulating macrophage polarization could be a potential therapeutic strategy. Wang et al. (2023) in another study, explored the expression profiles of microRNAs in peri-implantitis tissues and their impact on immune regulation. The study identified several microRNAs that were differentially expressed in peri-implantitis and found that they influenced immune cell function and cytokine production. The findings suggested that targeting specific microRNAs could help modulate the immune response and potentially offer new therapeutic options for peri-implantitis.(References are available in the book)
In a cohort study, Le et al. (2023) investigated the levels of inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α) in peri-implantitis patients and their correlation with tissue destruction. The results indicated that elevated cytokine levels were associated with more severe tissue loss and bone resorption. The study provided insights into how cytokine-driven inflammation contributes to the progression of peri-implantitis and highlighted the potential for targeting these cytokines in treatment. In a clinical trial, Zhang et al. (2023) evaluated the effects of systemic immune modulators on peri-implantitis. The study found that patients treated with immune-modulating agents, such as corticosteroids or immunosuppressants, showed reduced inflammation and improved clinical outcomes compared to those receiving standard care. The findings suggest that systemic immune modulation can help manage the inflammatory response in peri-implantitis. Liu et al. (2024) in their article in periodontology 2000, focused on …….Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…….
Outcome of research on host response and peri-implantitis
The recent studies highlight several key aspects of the host immune response in peri-implantitis:
- Genetic predisposition can affect the severity of the immune response.
- Systemic conditions like diabetes and smoking exacerbate inflammation.
- Macrophage polarization and microRNA expression play significant roles in disease progression.
- Targeting inflammatory cytokines and systemic immune modulation can improve treatment outcomes.
- Effective biofilm removal and the role of Tregs offer additional avenues for management.
These findings suggest a multifaceted approach to managing peri-implantitis, focusing on immune system modulation, systemic health management, and targeted therapies to improve patient outcomes.
Mechanical factors and peri-implantitis
Mechanical factors play a significant role in the development and progression of peri-implantitis.
Implant design
Implant design encompasses various aspects, including shape, size, and surface characteristics, all of which can influence the susceptibility to peri-implantitis. Threaded implants are designed to provide better mechanical stability and are often preferred for their ease of placement and initial stability. However, the threads can create microenvironments that may trap plaque and bacteria, particularly if they are not properly cleaned. Non-threaded implants, while potentially less prone to bacterial entrapment, might not offer the same initial stability and could be more susceptible to mechanical failure in certain situations. The dimensions of an implant can affect its mechanical stability and how well it integrates with the surrounding bone. Implants that are too short or too narrow might not achieve optimal osseointegration, potentially leading to increased mobility and a higher risk of peri-implantitis. Conversely, oversized implants can create excessive pressure on the surrounding bone and soft tissues, leading to complications.
Another important factor is implant-abutment connection. The connection between the implant and abutment can impact the seal and stability of the implant. Hexagonal connections are common and can provide a secure fit, but they may be prone to microleakage if not well-sealed. Conical connections can offer a more precise fit and better seal, potentially reducing bacterial infiltration and the risk of peri-implantitis. Platform switching also affects soft tissue response around neck of implant. Platform switching involves using an abutment with a narrower diameter than the implant platform. This design aims to maintain the crestal bone level by shifting the load away from the bone-implant interface. Research suggests that platform switching can reduce bone loss and the risk of peri-implantitis by preserving the bone around the implant.
Surface characteristics of implant
The surface of a dental implant is critical in determining its biocompatibility, osseointegration, and susceptibility to bacterial colonization. Various surface treatments and coatings have been developed to enhance implant performance, but they also have implications for peri-implantitis. Implants with rough surfaces, such as those treated with sandblasting or acid etching, tend to achieve better osseointegration due to increased surface area for bone growth. However, rough surfaces can also harbor more bacteria and plaque, potentially increasing the risk of peri-implantitis. On the other hand, smooth surfaces are less likely to trap bacteria but may not integrate as effectively with the bone. Hydrophilic surfaces attract water and can improve the initial adhesion of bone cells, promoting faster osseointegration. Hydrophobic surfaces repel water and may be less prone to bacterial adhesion, but they can also be more challenging to clean. The balance between these properties is crucial for minimizing the risk of peri-implantitis.
From the above discussion, it can be summarized that omplants with rough or porous surfaces may be more prone to bacterial colonization, as these surfaces provide niches for plaque accumulation. The presence of bacteria can lead to inflammation of the surrounding tissues, resulting in peri-implantitis. Effective oral hygiene practices and regular maintenance are crucial in mitigating this risk. The design of an implant, including its shape and connection type, affects its mechanical stability and load distribution. Implants that are improperly aligned or overloaded may experience …….Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…….
Review of literature on mechanical factors and peri-implantitis
Studies on mechanical factors and peri-implantitis have explored various aspects, including implant design, occlusal forces, and prosthetic components. A study by Albrektsson et al. (1986) found that rough implant surfaces have enhanced osseointegration compared to smooth surfaces, but they can also harbor more bacteria, which might increase the risk of peri-implantitis. This balance between improved bone integration and bacterial colonization is critical in implant design. In another study, Buser et al. (1997) indicated that threaded implants might be more susceptible to bone loss around the threads if not properly cleaned. This study emphasized the need for effective oral hygiene and regular maintenance to prevent peri-implantitis. A study by Jemt and Book (1996) demonstrated that implants placed at improper angles or depths can create difficult-to-clean areas, leading to increased plaque accumulation and a higher risk of peri-implantitis. Research by Koeck et al. (2011) showed that platform switching, which involves using a narrower abutment than the implant platform, can reduce the risk of peri-implantitis by shifting the load away from the crestal bone and minimizing bone loss.(References are available in the book)
A study by Pjetursson et al. (2007) found that excessive occlusal forces on implants could lead to bone loss and inflammation, increasing the risk of peri-implantitis. Proper occlusal adjustment is crucial to prevent mechanical overload and subsequent complications. Research by Reddy et al. (2013) highlighted the importance of biomechanical factors, including implant size and bone quality, in influencing the risk of peri-implantitis. Implants that are too large or small relative to the bone can experience uneven stress distribution, contributing to bone loss and inflammation. Another study by Abrahamsson et al. (2000) found that poorly fitting prosthetic components can lead to plaque accumulation and inflammation around the implant. The design and fit of crowns and bridges are essential in preventing peri-implantitis. Research by Stamatakis et al. (2005) indicated that a high crown-to-implant ratio, where the crown is disproportionately large compared to the implant, can lead to increased mechanical stress and a higher risk of peri-implantitis. A study by Lang et al. (2004) emphasized the importance of regular professional cleaning and patient oral hygiene in preventing peri-implantitis. Mechanical factors like implant design can affect how easily patients can clean around their implants. Research by Klinge et al. (1999) showed that implants exhibiting signs of mobility, often due to mechanical failure or poor osseointegration, are at a higher risk for developing peri-implantitis. Ensuring proper implant stability during and after placement is crucial to prevent complications.
de Melo et al. (2021) investigated the effect of surface treatments on biofilm formation around implants. They found that implants with certain surface treatments, such as titanium plasma-sprayed (TPS) and hydroxyapatite-coated surfaces, had different levels of biofilm accumulation, which could influence the risk of peri-implantitis. The study highlighted the need for balancing bioactivity with ease of cleaning. A 2021 study by Zhang et al. explored the impact of prosthetic design on peri-implantitis risk. The research found that prosthetic components with inadequate fit or design could lead to increased plaque accumulation and subsequent peri-implantitis. The study highlighted the need for precise prosthetic design and regular maintenance to prevent complications. Research by Kim et al. (2022) evaluated the impact of crown-to-implant ratio on peri-implantitis. The study concluded that high crown-to-implant ratios could lead to increased mechanical stress on implants, contributing to bone loss and a higher risk of peri-implantitis.(References are available in the book)
Research by Schneider et al. (2022) examined the impact of different thread designs on peri-implantitis risk. They found that implants with deep, wide threads could lead to greater plaque accumulation in thread grooves, potentially increasing the risk of peri-implantitis. The study suggested that optimizing thread design for easier cleaning could mitigate this risk. Wang et al. (2023) explored the impact of implant …….Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…….
Management of peri-implantitis
Managing peri-implantitis involves a comprehensive approach aimed at controlling inflammation, halting disease progression, and preserving the implant and surrounding tissues. A case of peri-implantitis should be treated in a systematic manner to achieve acceptable outcome. A peri-implantitis patient is managed in following steps,
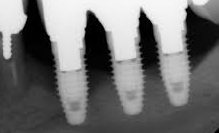
Diagnosis and assessment
Accurate diagnosis and assessment are crucial for effectively managing peri-implantitis. Examine the implant site for signs of inflammation, such as redness, swelling, and suppuration (pus). Look for signs of plaque or calculus buildup around the implant. Measure the probing depths around the implant using a periodontal probe. Increased probing depths compared to baseline measurements can indicate peri-implantitis. Pay attention to bleeding on probing (BOP) and suppuration, which are signs of inflammation. Check for any signs of implant mobility, which can suggest issues with osseointegration or mechanical failure. A stable implant should not show any movement. Periapical radiographs provide detailed images of the implant and surrounding bone. Assess bone levels around the implant to determine the extent of bone loss. Look for signs of bone loss around the implant threads or any radiolucencies indicating potential infection. While less detailed than periapical radiographs, panoramic images can provide an overview of the implant and surrounding structures. They are useful for assessing general bone loss and the position of multiple implants. For a more detailed evaluation, CBCT imaging can provide three-dimensional views of the implant site, allowing for a precise assessment of bone volume, density, and the extent of bone loss. In certain cases, microbiological testing may be performed to identify specific pathogens associated with peri-implantitis, such as Porphyromonas gingivalis or Aggregatibacter actinomycetemcomitans. This can help guide targeted antibiotic therapy if needed.
Review the patient’s medical history to identify any systemic conditions (e.g., diabetes, autoimmune diseases) that could influence the risk or progression of peri-implantitis. Assess lifestyle factors such as smoking, which is a known risk factor for peri-implantitis. Understanding these risk factors helps tailor the management plan and address potential contributing issues. Assess the occlusion to identify any signs of excessive forces on the implant. Poor occlusal balance or high occlusal loads can contribute to implant failure and peri-implantitis. Evaluate the design and fit of the prosthetic components. Poorly fitting prosthetics can contribute to plaque accumulation and peri-implantitis.
Classifications of peri-implantitis
There are number of classifications of peri-implant defects quoted in medical literature with their pros and cons but till date there is no uniformly accepted classification. Various system of classification proposed in literature described below.
Spiekermann (1984) characterized peri-implant defect into the type of bone resorption pattern into 5 categories.
Class I – Horizontal,
Class II – Hey-shaped
Class III a – Funnel shaped
Class III b – Gap-like
Class IV – Horizontal-circular form
This classification describes 5 different patterns of bone resorption around implant. No clinical criteria and treatment protocol for each class is given in it.
Nishimura et al. (1997) gave the following classification,
Class 1: Slight horizontal bone loss with minimal peri-implant defects
Class 2: Moderate horizontal bone loss with isolated vertical defects
Class 3: Moderate to advanced horizontal bone loss with broad, circular bony defects.
Class 4: Advanced horizontal bone loss with broad, circumferential vertical defects, as well as loss of the oral and/or vestibular bony wall
This classification reveals horizontal bony defect along with other types of bony defects around implant. No clinical picture, treatment modality and prognosis is highlighted.
Lang NP et al. (2004) in their classification included clinical signs, radiographic features and treatment to describe various stages of peri-implantitis.
Pocket depth (PD) <3 mm, no plaque or bleeding: No therapy
Stage A PD <3 mm, plaque and/or bleeding on probing: Mechanical cleansing and polishing, oral hygienic maintenance instructions.
Stage B PD 4–5 mm, radiologically no bone loss: Mechanical cleansing and polishing, oral hygienic maintenance instructions plus local anti-infective therapy (e.g Chlorhexidine).
Stage C PD >5 mm, radiologically bone loss <2 mm: Mechanical cleansing and polishing, microbiological test, local and systemic antibiotic therapy.
Stage D PD >5 mm, radiologically bone loss >2 mm: Respective or regenerative surgery
Schwarz et al. (2008) classified peri implant defect depending on the configuration of the bony defect as:
Class I defect – Intraosseous
Class II defect – Supra-alveolar in the crestal implant insertion area.
This Classification informs about only two classes. No clinical and radiological interpretation is evident.
Froum and Rosen (2012) Peri-implantitis is classified into,
- Early Peri-implantitis: PD≥4 mm, Bleeding and/or suppuration on probing, Bone loss <25% of the implant length.
- Moderate Peri-implantitis: PD≥6 mm, Bleeding and/or suppuration on probing, Bone loss ranging from 25% to 50% of the implant length.
- Advanced Peri-implantitis: PD≥8 mm, Bleeding and/or suppuration on probing, Bone loss >50% of the implant length.
(Bleeding and/or suppuration noted on two or more aspects of the implant. Bone loss measured on radiographs from time of definitive prosthesis loading to current radiograph. If not available, the earliest available radiograph following loading to be used.)
American Academy of Periodontology and the European Federation of Periodontology (2017)
In 2017, the world workshop planned and conducted jointly by the American Academy of Periodontology and the European Federation of Periodontology presented a consensus report (of workgroup 4) in which classification of Peri-Implant Diseases and Conditions was done,
- Peri‐implant health
- Peri‐implant mucositis
- Peri‐implantitis
- Soft‐ and hard‐tissue deficiencies
Non-surgical management of peri-implantitis
Non-surgical management of peri-implantitis focuses on controlling infection, reducing inflammation, and maintaining implant stability without resorting to surgical procedures. These methods are generally preferred due to their lower morbidity, reduced cost, and minimal patient discomfort. Non-surgical approaches are often the first line of treatment and can be effective, particularly in the early stages of peri-implantitis.
Mechanical Debridement
Mechanical debridement involves the removal of bacterial biofilm and calculus from the implant surface. This can be achieved through various instruments and techniques. Manual scaling using plastic, titanium, or carbon fiber curettes is a common approach. These instruments are designed to minimize damage to the implant surface while effectively removing biofilm and calculus. Ultrasonic scalers equipped with specialized tips for implant maintenance can be used to disrupt and remove biofilm. These devices use high-frequency vibrations to dislodge deposits and are considered effective for non-surgical debridement. Air abrasion involves the use of a stream of air mixed with abrasive particles to clean the implant surface. This method can effectively remove biofilm and surface contaminants without causing significant damage to the implant.
LASER treatment
Among the various non-surgical treatment modalities, laser therapy has emerged as a promising approach due to its antimicrobial properties, precision, and minimally invasive nature. This section will delve into the types of lasers used in treating peri-implantitis, their mechanisms of action, clinical efficacy, advantages, and potential limitations. Several types of lasers have been studied and utilized in the management of peri-implantitis, each with unique properties and applications. Erbium laser operates at a wavelength of 2940 nm and is well absorbed by water and hydroxyapatite, making it suitable for both hard and soft tissue applications. It is particularly effective in removing biofilm and calculus from implant surfaces without causing significant thermal damage to the surrounding tissues. Diode lasers, typically operating in the wavelength range of 810-1064 nm, are known for their bactericidal effects and ability to …….Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…….
Antimicrobial treatment
Antimicrobial treatments aim to reduce bacterial load and control infection in peri-implant tissues. Local delivery of antibiotics, such as minocycline or doxycycline, can be effective in managing peri-implantitis. These antibiotics can be applied directly to the affected area, providing high local concentrations while minimizing systemic exposure. Topical antiseptics, such as chlorhexidine or povidone-iodine, can be used as adjuncts to mechanical debridement. These agents have broad-spectrum antimicrobial activity and can help reduce bacterial load. Photodynamic therapy (PDT) involves the use of a photosensitizing agent and a specific wavelength of light to produce reactive oxygen species that kill bacteria. PDT has shown promise in reducing bacterial load and inflammation in peri-implantitis.
Adjunctive Therapies
Adjunctive therapies can enhance the effectiveness of non-surgical treatment and promote healing. Probiotics are beneficial bacteria that can help restore a healthy microbial balance in the oral cavity. They can be used as adjuncts to mechanical debridement and antimicrobial treatments to enhance the therapeutic outcome. Host modulation therapy aims to alter the host response to inflammation. Agents such as nonsteroidal anti-inflammatory drugs (NSAIDs) or subantimicrobial-dose doxycycline can help reduce inflammation and promote tissue healing. Photobiomodulation, also known as low-level laser therapy (LLLT), uses low-intensity lasers or light-emitting diodes (LEDs) to promote tissue healing and reduce inflammation. This therapy can be used as an adjunct to other non-surgical treatments to enhance their effectiveness.
Maintenance and Prevention
Regular maintenance and preventive measures are essential to managing peri-implantitis and preventing recurrence. Patients should receive comprehensive oral hygiene instructions to ensure effective plaque control. This includes proper brushing techniques, the use of interdental brushes, and the importance of regular dental check-ups. Regular professional maintenance visits are crucial for monitoring implant health and performing necessary interventions. This includes routine cleaning and debridement to prevent biofilm accumulation and the early detection of any signs of peri-implantitis. Addressing and managing risk factors, such as smoking cessation and controlling systemic conditions like diabetes, is vital for preventing peri-implantitis. Patients should be educated about the impact of these factors on implant health and encouraged to adopt healthier lifestyles.
Surgical management of peri-implantitis
The primary goals of surgical intervention are to eliminate infection, detoxify the implant surface, regenerate lost bone, and re-establish a healthy peri-implant environment. Effective surgical management requires a thorough understanding of the disease process, careful patient selection, and the application of appropriate surgical techniques. The objectives of surgical management of peri-implantitis include:
Complete Removal of Inflamed and Infected Tissues: This involves the excision of granulation tissue and debridement of the infected peri-implant pocket to reduce bacterial load and inflammation.
Detoxification of the Implant Surface: Effective cleaning and decontamination of the implant surface to remove biofilm, calculus, and endotoxins are crucial for reducing bacterial colonization and promoting tissue healing.
Regeneration of Lost Bone: Where possible, regenerative techniques aim to restore the lost bone around the implant, improving the support and stability of the implant.
Re-establishment of a Healthy Peri-implant Environment: Creating conditions that facilitate the reattachment of soft tissues to the implant surface and prevent further bacterial colonization.
Indications for Surgical Treatment
Surgical treatment of peri-implantitis is indicated in the following scenarios:
Advanced Peri-implantitis: When there is significant bone loss, deep peri-implant pockets, and non-surgical treatments have failed to arrest the progression of the disease.
Persistent Infection: Cases where non-surgical debridement and antimicrobial therapy have not resolved the infection.
Structural Defects: Presence of significant structural defects around the implant that require reconstruction.
Aesthetic Concerns: Situations where peri-implantitis affects the aesthetic appearance of the implant site, particularly in the anterior region.
Surgical Techniques
Several surgical techniques are available for the management of peri-implantitis, each with specific indications and protocols. The choice of technique depends on the extent of the disease, the morphology of the defect, and the goals of treatment.
Open Flap Debridement (OFD)
Open flap debridement is a fundamental surgical technique that involves raising a mucoperiosteal flap to gain access to the peri-implant pocket for thorough debridement and implant surface decontamination. It is performed in presence of moderate to advanced peri-implantitis with significant bone loss and presence of deep peri-implant pockets that are inaccessible through non-surgical means.
Procedure involves placing a crestal incision is made, and a full-thickness flap is raised to expose the peri-implant tissues and the implant surface. Granulation tissue and inflamed soft tissue are removed using curettes or ultrasonic devices. Mechanical debridement is performed to remove biofilm and calculus from the implant surface. Implant surface decontamination id done using various methods, including chemical agents (e.g., chlorhexidine, citric acid), air abrasion, or laser therapy, can be used to detoxify the implant surface. The flap is repositioned and sutured to achieve primary closure. The primary advantage of the procedure is that it provides direct access to the peri-implant pocket, allowing thorough debridement and implant surface cleaning. However, it has limited potential for bone regeneration and does not address significant bone defects.
Resective Surgery
Resective surgery involves the removal of peri-implant hard and soft tissues to create a more maintainable environment and reduce pocket depths. Indications include advanced peri-implantitis with severe bone loss and vertical defects and cases where regenerative procedures are not feasible or indicated. A mucoperiosteal flap is raised to expose the affected area. Bone recontouring is performed to remove defects and create a more favorable architecture. Soft tissue resection may also be performed to reduce pocket depths. As explained in open flap debridement, the implant surface is cleaned and detoxified. The flap is …….Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…………Content available in the book…….
Regenerative Surgery
Regenerative surgery aims to restore lost bone around the implant using bone grafts, barrier membranes, or growth factors. It is indicated in cases with moderate to advanced peri-implantitis with significant horizontal or vertical bone defects and it is intended to restore lost bone and improve implant stability. A mucoperiosteal flap is raised to expose the peri-implant defect. Thorough debridement and cleaning of the defect and implant surface are performed. Autogenous bone grafts, allografts, xenografts, or synthetic bone substitutes are placed in the defect to promote bone regeneration. Resorbable or non-resorbable membranes may be used to stabilize the graft and prevent soft tissue invasion. The flap is repositioned and sutured to achieve primary closure, ensuring stability of the graft. The procedure has advantage as it has potential for significant bone regeneration and improved implant stability. However, the procedure is technique-sensitive, with higher risk of complications, and longer healing time.
Implantoplasty
Implantoplasty involves the mechanical modification of the implant surface to reduce its roughness and make it less conducive to bacterial colonization. The procedure is indicated in cases with advanced peri-implantitis with exposed implant threads and in cases where implant surface modification is necessary to facilitate cleaning. A mucoperiosteal flap is raised to expose the implant. Rotary instruments are used to smoothen the implant surface, removing exposed threads and creating a polished surface. Thorough debridement and cleaning of the modified implant surface are performed. The flap is repositioned and sutured to achieve primary closure. Advantages of the procedure include reduced surface roughness, making the implant less susceptible to bacterial colonization and easier to maintain. On the other hand, limitations include potential for structural compromise of the implant and difficulty in achieving smooth surface in some cases.
Combined Surgical Approaches
In some cases, a combination of surgical techniques may be necessary to achieve optimal results. For example, resective surgery may be combined with regenerative procedures to address both the removal of infected tissues and the restoration of lost bone. These approached are indicated in cases with complex peri-implantitis with both horizontal and vertical bone defects and cases requiring both pocket reduction and bone regeneration. The procedure involves a combination of the steps outlined in the respective techniques, tailored to the specific needs of the patient and the clinical presentation. These procedures provide a comprehensive approach that addresses multiple aspects of peri-implantitis. However, the procedures have increased complexity, longer surgical time, and higher risk of complications.
Conclusion
Peri-implantitis is a condition characterized by inflammation in the tissues surrounding dental implants, leading to the loss of supporting bone. Its management is crucial to ensuring the longevity and success of dental implants. Non-surgical management of peri-implantitis encompasses a range of approaches aimed at controlling infection, reducing inflammation, and maintaining implant stability. Mechanical debridement, laser therapy, antimicrobial treatment, and adjunctive therapies each play a role in managing this condition. Regular maintenance and preventive measures are essential to preventing recurrence and ensuring the long-term success of dental implants. Ongoing research and emerging therapies hold promise for further improving the non-surgical management of peri-implantitis, ultimately enhancing patient outcomes and implant longevity. Surgical management of peri-implantitis is a critical component in the comprehensive treatment of this challenging condition. Various surgical techniques, including open flap debridement, resective surgery, regenerative surgery, implantoplasty, and combined approaches, offer tailored solutions based on the severity and morphology of the peri-implant defects. Successful surgical management requires careful patient selection, thorough understanding of the disease process, and meticulous execution of surgical protocols. Post-operative care and long-term maintenance are equally important to ensure the stability and health of the implant.
Continued research and advancements in surgical techniques and materials hold promise for further improving the outcomes of surgical management of peri-implantitis. By integrating evidence-based practices and staying abreast of the latest developments, dental professionals can enhance the prognosis for patients with peri-implantitis and contribute to the long-term success of dental implants.
References
References are available in the hardcopy of the website “Periobasics: A Textbook of Periodontics and Implantology”.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:

