Introduction
Viral infections are commonly seen on the oral mucosa and surrounding soft tissues. Many infections are subclinical and subside without any complication. However, with an increasing number of patients with immunosuppression, iatrogenic immunosuppression, anticancer therapy and organ transplant, these infections present with significant morbidity and complications. In the following discussion, we shall read about various viral infections that involve the oral cavity, their diagnosis, and treatment.
Herpesviruses
These are a large group of DNA viruses, with at least eight well-known herpes subtypes which are pathogenic in humans. These include herpes simplex virus-1, herpes simplex virus-2, varicella–zoster virus, Epstein–Barr virus, human cytomega-lovirus, human herpesvirus-6, human herpesvirus-7, and human herpesvirus-8. The Herpesviridae family is divided into the alpha, beta and gamma subfamilies. The alpha family consists of herpes simplex virus-1 (oral-facial type), herpes simplex virus-2 (genital type), varicella-zoster virus. The beta subfamily consists of human cytomegalovirus, human herpesvirus-6, and human herpesvirus-7. The gamma subfamily consists of Epstein–Barr virus and human herpesvirus-8. Table 29.7 enumerates the herpetic infections of the oral mucosa.
Let us now discuss these viruses and infections caused by them in detail.
Herpes simplex virus
Herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2) are double-stranded DNA viruses of the Herpesviridae family. HSV infection most commonly causes genital or orolabial ulcerative disease. Genital HSV is the leading cause of genital ulcerative disease worldwide. Orolabial herpes infection is most commonly caused by HSV type 1; whereas, genital infection is commonly seen with HSV-2 Infection occurs from contact with infectious secretions on oral, genital or anal mucosa or abraded skin. The herpes simplex virion consists of four components:
- An electron-dense core containing viral DNA;
- An icosadeltahedral capsid;
- An amorphous, at times eccentric layer of proteins, designated tegument, which surrounds the capsid; and
- An envelope.
HSV-1 causes primary (acute) herpetic gingivostomatitis. The initial exposure of the virus usually occurs during childhood, causing primary infection between 6 months to 5 years of age. Most infections are subclinical. The virus replicates in the nucleus of the host cell. The vesicles formed by the lysis of epithelial cells rupture to leave behind ulcers which heal without scar formation. Spread occurs through the infected saliva or droplets. Infectivity exists even in the absence of visible lesions. The virus remains latent in the regional ganglion after the primary infection and reappears whenever there is a trigger.
The affected children present with fever, localized lymphadenopathy, irritability, and poor feeding. Most comm-only, small vesicles appear on the gingiva which eventually rupture, leaving behind small, shallow, irregular painful ulcers. These ulcers often have a yellow exudate. Primary infection in adults is similar to children; however, the ulcers may be limited to posterior pharynx and tonsils. In young adults, who present with pharyngotonsillitis, the diagnosis of primary infection should be considered, which should be confirmed by laboratory tests. The disease is generally limited to the oral cavity and usually subsides within 10-14 days. Interferon and humoral, mucosal, and cellular immunity are important defenses against this infection. Herpes labialis is ………..Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book…….. ‘Herpetic whitlow’. Herpes simplex virus infections are more severe in immunocompromised hosts where non-mucosal or systemic HSV infection can occur. HSV eye disease includes keratoconjunctivitis and acute retinal necrosis. Systemic HSV infection may result in pneumonia, hepatitis, esophagitis, and CNS disease. HSV infection of the CNS can cause aseptic meningitis, encephalitis, myelitis, and radiculopathy.

Diagnosis of the infection is done on the basis of clinical examination and confirmatory tests in the lab. Microscopi-cally, HSV infected tissue demonstrates intraepithelial cell balloonings, inflammatory cells, virus-infected epithelial cells, and acantholytic epithelial cells (Tzanck cells), although these findings are not specific for herpes. The most useful and accurate test is PCR (polymerase chain reaction) test. Swabs should be taken from the base of the lesion or fluid from the vesicle. A positive PCR test must be interpreted in context with the clinical presentation and histology.
Management
Ideally, the anti-viral treatment should be started at the onset of prodromal symptoms. Acyclovir is the drug of choice and it acts via inhibition of viral DNA replication. Application of 5% topical acyclovir ointment 5 times a day decreases the duration of herpes labialis. Primary genital herpes can be treated with 200 to 400 mg acyclovir 5 times a day. With any primary lesion, supportive therapy is indicated (analgesics, nonsteroidal anti-inflammatory drugs, lavage, hydration). Prophylactic treatment with acyclovir 400 mg twice a day, valacyclovir 1 gm daily, or famciclovir 250 mg twice daily reduces the prevalence and severity of recurrence. It is important to note here that dental professionals should follow the universal precautions and maintain appropriate hygiene while treating these patients.
Varicella
Varicella (chickenpox) is caused by primary varicella-zoster virus (HHV-3) infection. The Varicella-zoster virus is highly contagious; about 95 percent of adults show serologic evidence of infection. Reactivation of latent virus (usually in adults) causes herpes zoster (shingles), manifesting as a vesicular rash with a dermatomal distribution and acute neuritis. The primary infection is commonly acquired during the childhood, usually presenting as a benign self-limiting illness with fever and generalized pruritic vesicular rash. Following primary infection, VZV establishes lifelong latency in the cells of the dorsal root ganglia. Reactivation of this infection causes herpes zoster disease that usually occurs during immunocompromised states, stress and in HIV infection. Reactivation is more common in HIV seropositive patients, and in those with advanced immune deficiency, it may result in severe and disseminated clinical disease. As with herpes simplex virus, interferon and cellular and humoral immunity are important defenses.
Cutaneous disease, Herpes zoster usually appears as a localized, erythematous, maculopapular eruption along a single dermatome, but may be multi-dermatomal. The vesicular distribution is unilaterally in a linear fashion. Typically, it affects the sensory nerves of the trunk, head, and neck, resulting in symptoms of pain or paresthesia in those dermatomes. Vesicular primary lesions ulcerate and heal over in 1 to 2 weeks. The second division ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book……..
The diagnosis is made primarily on the basis of clinical examination. The microscopic analysis demonstrates acan-tholysis of epithelial cells that results in numerous free-floating Tzank cells, with margination of chromatin along the nuclear membrane and occasional multinucleation.
Management
The treatment is supportive and symptomatic, with topical or systemic antipruritics and analgesics that do not contain aspirin. A high dose of oral acyclovir (800 mg five times daily for seven days) is recommended for treating both primary and recurrent infections in immunocompromised patients. The patient should stay hydrated. Controlling autoinoculation to other sites can be a challenge in a child patient. Systemic antiviral treatment, if at all given, should be initiated as early as possible in the prodromal stage.
Epstein-Barr virus (HHV-4)
Infectious mononucleosis
The infection with Epstein-Barr virus (EBV) has been associ-ated with the development of infectious mononucleosis, which is a clinical entity characterized by pharyngitis, cervical lymph node enlargement, fatigue, and fever. The spread of the virus occurs from oral secretions. The virus is spread by intimate oral contact among adolescents (also known as “Kissing Disease”), but how preadolescents acquire the virus is not known. Shedding of EBV ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book……..
As already stated, the infection is most common in young adults. Most of the times, the infection is sub-clinical and unrecognized, especially in adolescents. The main symptoms of the disease include fever, malaise, and lymphadenopathy. The disease may be indistinguishable from upper respiratory tract infection. Sometimes the patients have a high fever with a rubelliform rash. Misdiagnosis may result in the administra-tion of antibiotics (amoxicillin, ampicillin or penicillin) which may result in a maculopapular rash, which again is misdiagnosed as penicillin allergy. Oral lesions include transient petechial hemorrhages that occur on soft palate and pharynx and usually resolve within 1-2 days. The pharyngeal tonsils may be swollen and may have white exudate.
The diagnosis of the suspected patient is made by hematologi-cal examination. Complete blood count reveals elevated leukocytes and peripheral blood smears shows atypical lymphocytes. Monospot test is a rapid screening test in which antibodies (heterophile antibody) against EBV cross-react and agglutinates with sheep red blood cells.
Management
The treatment is primarily supportive and symptomatic. Most cases resolve spontaneously within 4 to 6 weeks and only require treatment of clinical symptoms. Nonsteroidal anti-inflammatory drugs are used for fever reduction and bed rest is advised for malaise and fatigue. Acyclovir is the drug of choice during the early phase of the disease. However, many studies suggest that it is not so effective. Hence, treatment is primarily supportive.
Oral hairy leukoplakia (OHL)
OHL is a white, vertically corrugated, non-removable lesion on the lateral or ventral margin of the tongue. This lesion is caused by the EBV and has no premalignant potential. It occurs almost exclusively in human immunodeficiency virus (HIV)-infected patients and is predictive for the development of progressive immune suppression and acquired immuno-deficiency syndrome (AIDS). In many cases, Candida albicans can be demonstrated within the leukoplakia. However, after the elimination of the yeast with antifungal therapy, the plaques persist which supports the viral etiology of the disease. Furthermore, Epstein-Barr virus ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book……..
Management
Because OHL is a benign lesion with low morbidity, It does not require specific treatment in every case. Indications for treatment include symptoms attributable to the lesion, or a patient’s desire to eliminate the lesion for cosmetic reasons. Systemic antiviral drugs such as desciclovir, valacyclovir, acyclovir, and ganciclovir have been used for OHL treatment with recurrence observed after discontinuation.
Cytomegalovirus (HHV-5)
The cytomegalovirus (CMV) causes a primary infection and then remains latent in the body. Despite causing a usually harmless primary infection, CMV can be life-threatening for immunocompromised patients and can cause serious fetal damages. The virus replicates mainly in the salivary glands and kidneys and is shed in saliva, semen, and urine. Therefore, people can be easily infected (including pregnant women) by person-to-person contact, sexual contact or taking care of young infected children. The infection manifests clinically in three forms. The congenital ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book…….. In about 10 % of older children and adults, primary cytomegalovirus infection causes a mononucleosis syndrome with fever, malaise, atypical lymphocytosis, and pharyngitis. The immunocompromised patients (transplant recipients and human immunodeficiency virus [HIV]-infected individuals) may develop life-threatening disseminated disease involving the lungs, gastrointestinal tract, liver, retina, and central nervous system.
The diagnosis of the infection is done on the basis of clinical examination and investigations like, the polymerase chain reaction (PCR) and serological tests. A biopsy can be performed and should be done in chronic ulcers for imm-unocompromised patients that do not respond to conservative therapy.
Management
Although most of the cases resolve spontaneously, intraven-ous ganciclovir is recommended for treatment of CMV infections. The treatment is particularly recommended in patients with HIV/AIDS. In these patients, the best treatment is an improvement of their immune status by treatment with highly active antiretroviral therapy (HART).
Kaposi’s sarcoma
Kaposi’s sarcoma is characterized by angioproliferative multifocal tumors of the skin, mucosa and less frequently the viscera. It is caused by Kaposi sarcoma-associated herpes-virus (KSHV), also known as human herpesvirus-8 (HHV-8). The reason for the proliferative lesion is that the virus brings genes into the cells that can cause the cells to divide too much and to live longer than they should. These types of changes may eventually turn them into cancer cells. Most of the people who get infected with this virus do not show any clinical sign or symptom. However, in HIV seropositive ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book…….. There are four different epidemiological forms of Kaposi’s sarcoma,
- Classic Kaposi’s sarcoma, affecting elderly men of Medit-erranean or Eastern European Jewish ancestry;
- Endemic Kaposi’s sarcoma, existing in Central and Eastern Africa, which has been described long before The HIV pandemic and often affects children;
- Iatrogenic Kaposi’s sarcoma, developing in immunosupp-ressed individuals; and
- Epidemic or AIDS-associated Kaposi’s sarcoma, a major AIDS-defining malignancy.
The diagnosis is primarily done on the basis of clinical features, histological examination, and PCR test. Typical findings at manifestation are a few asymptomatic purple macules or nodules. These lesions have a predilection for distribution along relaxed skin tension lines. Plaque-like and nodular Kaposi’s sarcoma lesions often become confluent and can be accompanied by massive lymphedema. In the oral cavity, the hard palate is frequently affected (Figure 29.4). Lesions begin with purplish erythema and progress to plaques and nodules that ulcerate easily. The histological examination of Kaposi’s sarcoma lesions reveals that they are largely comprised of cells of endothelial origin with a unique spindled morphology, and these are accompanied by a variable chronic inflammatory infiltrate.

Management
With the introduction of highly active antiretroviral therapy (HAART), there has been a substantial reduction in the prevalence, morbidity, and mortality associated with AIDS-related Kaposi’s sarcoma. There are many modalities of treatment for Kaposi’s sarcoma, which are divided into two main types, local and systemic. Local treatment includes surgical excision, cryotherapy, radiotherapy, laser, sclerothe-rapy, photodynamic therapy, intralesional chemotherapy (vinblastine, vincristine, bleomycin), intralesional IFN-α and Intralesional IL-2 therapy. Systemic treatment includes administration of drugs like vinblastine, vincristine, bleomy-cin, doxorubicin, liposomal doxorubicin or daunorubicin and etoposide. Recently, anti-angiogenesis therapy has been introduced for the treatment of Kaposi’s sarcoma.
Papilloma viruses
Human papillomavirus (HPV) is a DNA virus that can cause a chronic infection of either skin or mucosal epithelium. More than 90 subtypes of papillomaviruses have been identified so far out of which 25 strains of HPV have been associated with oral lesions. The commonly observed HPV associated oral lesions are,
Focal epithelial hyperplasia (Heck’s disease)
It presents with multiple asymptomatic, slightly elevated, mucosa-colored, smooth-surfaced nodules that occur on the labial or buccal mucosa gingivae or tongue in children. The nodules are usually between 1 and 2 mm in diameter and are of the same color as the normal mucosa. The lesions are symptomless and there is no evidence of induration or inflammation. Histological examination demonstrates acan-thosis of the oral epithelium. The rete ridges are commonly widened, often confluent, and sometimes club-shaped. Some superficial keratinocytes show koilocytic changes which are specific to HPV infection.
Management
The lesions demonstrate low infectivity and occasionally show spontaneous remission. However, sometimes the lesions are extensive and do not resolve spontaneously. They may cause significant cosmetic problems to the patient. Surgical removal is one option for extensive lesions; however, it has limited use if the lesions are widespread. Alternatively, Lasers can be used because of their hemostatic effect. Another treatment is systemic therapy with IFN-α. But, it is expensive with significant side effects. Recently, topical IFN-β treatment has been described with good results.
Squamous cell papilloma
Squamous cell papilloma is a benign, hyperplastic wart-like localized proliferation, representing an exaggerated growth of normal squamous epithelium. It is caused by human papilloma virus 6 and 11 (HPV 6 and HPV 11) which are less virulent and have a low infectivity rate. The benign proliferation of the stratified squamous epithelium occurs most frequently on the hard and soft palate, uvula, tonsil, or epiglottis, but any surface of the oral cavity can be affected. These lesions are often asymptomatic and tend to progress slowly.
Management
Surgical removal with laser ablation, electrocautery, intra-lesional injections of interferon, cold-steel excision, and cryosurgery have been used in the treatment of oral squamous papillomas.
Verruca vulgaris
Verruca vulgaris or the common wart is a discrete, benign, epithelial hyperplasia that tends to manifest as papules and plaques with cleft surfaces. They are caused by certain types of HPV that commonly infect the keratinized skin, usually at sites of minor trauma. The most frequent HPV infection is HPV-2, followed by HPV-4, HPV-7, HPV-26, and HPV-27. It replicates simultaneously with the differentiation of epidermal cells, leading to maturation of viral particles in the granular cell layer. The viral particles are released ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book……..
Management
Conservative surgical excision with safe margins is the treatment of choice for intraoral warts. Extra-oral warts can be treated by scalpel excision, liquid nitrogen cryotherapy or application of lasers.
Condyloma accuminatum
Condyloma acuminatum is caused by HPV-6 or HPV-11. The latency of condyloma acuminatum is 2 to 3 months. This infection primarily occurs in the genital region; however, other sites may also be involved. Multiple verrucous papules of papillary or cauliflower shape occur in the genitalia or perianal region. The virus invades through minor external injury of the genitalia, perianal region, or vaginal introitus, and infects epidermal basal cells, inducing abnormal cellular proliferation. The papules are infiltrative at the surface and may give off a foul odor. The most common intra-oral sites are the labial mucosa and the lingual frenum and soft palate.

Management
No treatment is usually required for focal epithelial hyper-plasia, as the nodules undergo spontaneous regression during puberty. However, if required, the growth can be removed with scalpel excision, liquid nitrogen cryotherapy or applica-tion of lasers.
Picornaviruses
Picornaviruses are nonenveloped, single-stranded, positive-sense RNA viruses with a virion diameter of approximately 30 nm. The Picornaviridae family consists of nine genera and contains several serious pathogens, including poliovirus, hepatitis A virus, rhinovirus, and the hand, foot and mouth disease virus. The Enterovirus genus in the picornavirus family includes Coxsackie virus (23 serotypes), echovirus (28 serotypes), poliovirus (3 serotypes) and human enterovirus (4 serotypes).
Herpangina and hand, foot, and mouth disease
This disease is caused by Coxsackie viruses. Coxsackie viruses are divided into group A and group B viruses. Type A viruses cause herpangina (sores in the throat) and hand, foot, and mouth disease. Type B viruses cause epidemic pleuro-dynia, and inflammation in the chest. In this disease, there is inflammation of the mouth and throat. It most often affects young children (1 to 10 years). Most commonly, small red spots appear at the back of the mouth which then become little fluid-filled sacs (vesicles) that quickly pop, leaving small ulcers or sores. The ulcers are ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book……..
Management
There is no specific treatment for these infections. The ulcers formed usually heal within 7-10 days. Symptomatic treatment is indicated in very painful cases of herpangina, in which case non-aspirin antipyretics and topical anesthetics can be used.
Paramyxoviruses
Paramyxoviridae is a family of RNA viruses. They cause a variety of diseases in humans, such as mumps, measles, respiratory infections in infants. The family Paramyxoviridae consists of three genera: Paramyxovirus, which includes the parainfluenza viruses and mumps virus; Pneumovirus, which includes respiratory syncytial virus; and Morbillivirus, which includes the measles virus.
Rubeola (Measles)
Rubeola belongs to the family paramyxovirus, an RNA enveloped virus that is highly contagious. Rubeola is spread via airborne droplets through the nasopharyngeal respiratory epithelium. The disease is characterized by fever, conjuncti-vitis, upper respiratory tract symptoms and characteristic maculopapular eruptions on the trunk. Oral manifestations usually precede the onset of the disease, with characteristic white spots occurring on the buccal mucosa (Koplik spots). These spots represent the foci of epithelial necrosis and are pathognomonic for measles. The lesions heal spontaneously and no treatment is required. This disease is now uncommon because of widespread use of immunization.

Mumps
Mumps is an acute viral illness caused by a paramyxovirus. It is generally a mild childhood disease, most often affecting children between five to nine years of age. However, the mumps virus can infect adults as well and when it does, possible complications are more likely to be serious. The classic symptom of mumps is parotitis (i.e., acute onset of unilateral or bilateral tender, self-limited swelling of the parotid or other salivary gland [s]), lasting at least 2 days, but may persist longer than 10 days. The incubation period for the disease is 12-25 days, but ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book…….. Very rarely, mumps can cause encephalitis and permanent neurological damage. Mumps vaccine is available and is recommended for children at 12 months of age, with a second dose recommended at 4 to 6 years of age. This vaccine is given as measles-mumps-rubella (MMR) vaccine.

Retroviruses
Retroviridae is a family of enveloped viruses that replicate in a host cell through the process of reverse transcription. These viruses cause a variety of diseases such as cancer, AIDS, autoimmune diseases, and diseases of the central nervous system, bone and joints. The retroviruses complete their life cycle in two phases. The early phase refers to the steps of infection from cell binding to the integration of the viral cDNA into the cell genome, whereas the late phase begins with the expression of viral genes and continues through to the release and maturation of progeny virions. The most important virus in this family of viruses is the human immunodeficiency virus or HIV.
Human immunodeficiency virus
The human immunodeficiency virus (HIV) is a retrovirus belonging to the family of lentiviruses which causes AIDS (acquired immune deficiency syndrome) in humans. Since the identification of this virus, extensive research has been done on HIV to understand its life cycle, routes of transmission, pathogenesis of AIDS and possible cure for the disease. Although development of anti-HIV drugs and vaccines have been ongoing for a long time, but still many aspects of HIV pathogenesis remain unclear. The main reason, because of which the successful treatment of HIV infection is so difficult is “its rapid rate of evolutionary change”. We are still in a process to reconstruct the ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book……..
Structure of HIV
HIV consists of a cylindrical center surrounded by a sphere-shaped lipid bilayer envelope. The virus particle has a diameter of about 1/10,000 mm. Structurally, the virus is composed of three components: viral envelope, HIV matrix proteins, and the viral core.
Viral envelope
As already stated, the viral envelope consists of a lipid bilayer. In the lipid bilayer, there are two major glycoproteins, gp120 and gp41. These glycoproteins are primarily involved in recognition of CD4+ cells and chemokine receptors, thereby enabling the virus to attach to and invade CD4+ cells. HIV infects cells that carry the following receptor and co-receptor,
- CD4: Expressed on the surface of CD4 T lymphocytes (helper T lymphocytes) and macrophages (including dendritic cells).
- CCR5: Expressed on CD4+ T lymphocytes and on macrophages.
- CXCR4: Expressed on CD4+ T lymphocytes and T cell lines.
HIV matrix proteins
The HIV matrix protein consists of p17 protein, which lies between the envelope and core.
Viral core
It is formed of viral capsule protein p24 which surrounds two ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book…….. to make structural proteins for new virus particles.
‘gag’ gene contains around 1500 nucleotides. It gives rise to a 55-kilodalton (kD) gag precursor protein p55. This protein is later on cleaved into four smaller proteins which form the building blocks for the viral core,
- CA (Capsid protein p24).
- MA (Matrix protein p17) (this protein is part of the “matrix” which anchors the core to the viral envelope).
- NC (Nucleocapsid protein p9).
- p6.
‘pol’ gene encodes for enzymes required for various cellular processes in HIV which include,
- Protease.
- RNAse H.
- Integrase.
‘env’ gene encodes for a single protein, gp160. After synthesis, this protein travels to the cell surface where it is split into two parts gp120, and gp41, by enzymatic action.
The HIV lifecycle
All viruses are obligate, intracellular parasites of cells, which means that they require a living cell in order to reproduce. The life cycle of HIV starts in a host after its transmission from an infected person. The HIV is primarily transmitted by three routes: sexual, parenteral (blood-borne), and perinatal. Virtually all cases of HIV transmission can be attributed to these exposure categories. The sexual transmission of HIV can occur through male-to-female, female-to-male, male-to-male, and female-to-female sexual contact. The parenteral transmission may occur in recipients of infected blood or ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book…….. Transmission occurs through parenteral or mucous membrane exposure to blood. However, the risk is less than 1% and can be further reduced by the availability of more effective Antiretroviral Therapy (ART).
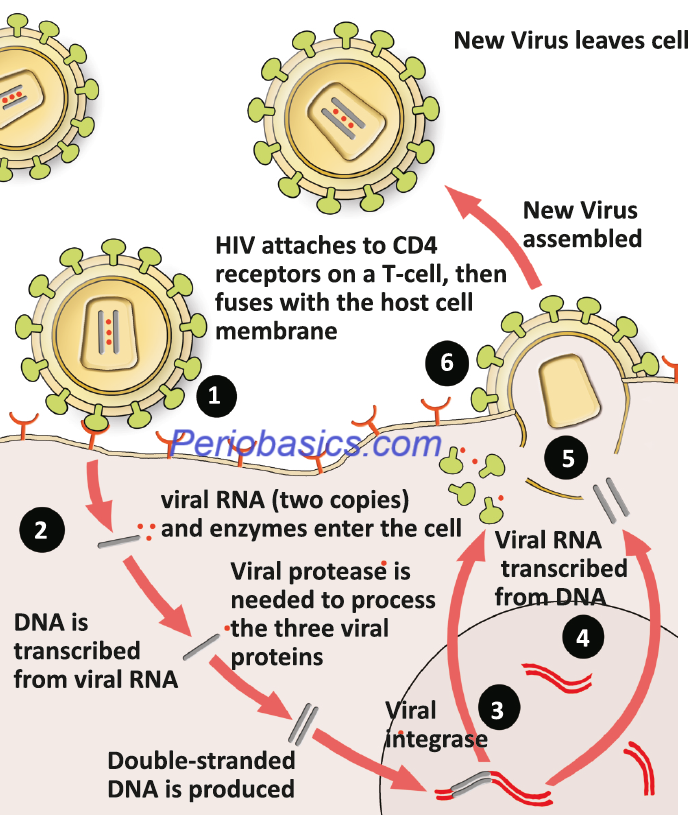
The lifecycle of HIV starts in a host with the fusion of GP120 glycoprotein on the HIV envelope with the CD4 receptor and one of two co-receptors, CCR5 or CXCR4, on the surface of a CD4+ T- lymphocyte. The virus then fuses to the host cell and releases its genetic material, that is, RNA into the host cell cytoplasm. Next step is the formation of viral DNA. Reverse transcriptase, an HIV enzyme converts the single-stranded HIV RNA to double-stranded HIV DNA. The newly formed HIV DNA, then enters the host cell’s nucleus. In the nucleus, the viral DNA gets embedded into the host cell DNA with the help of a viral enzyme, DNA integrase. The integrated HIV DNA is called a provirus. This provirus may remain inactive for many years, producing……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………
After an individual gets infected with HIV, there is an initial burst of viral replication. The population of viral particles in the blood may reach 10,000,000/ml. The infected person may experience flu-like symptoms for up to 2 weeks. The patients usually complain of their condition as ‘worse flu ever’. Other symptoms include fever, swollen glands, sore throat, rash, muscle and joint aches and pains, fatigue, and headache. This phase of HIV infection is referred to as “acute retroviral syndrome” (ARS) or “primary HIV infection. The seroconversion occurs after 3 to 8 weeks. Because large numbers of viruses are produced during the initial period following infection, they use CD4 cells to replicate and destroy them in the process. Hence, there is a sharp downfall in CD4 cell count.
After the initial TH cell decline, the body starts generating an antibody response against HIV. This reduces the HIV count in the blood. The helper T-cell population recovers and the immune response is generated against the virus which keeps it at a low and steady level. This level of virus in the blood is referred to as “viral set point”. Over a period of time, the immune system fails to cope up with the viral load due to infection of helper T-cells and viral levels rise again. The patient starts experiencing opportunistic infections such as Candida albicans infections of the mouth or vagina, persistent diarrhea, fever, weight loss and reactivation of previous infections such as shingles and tuberculosis. Eventually, the body fails to recover from these infections and the patient dies.
Staging of HIV
The WHO (2005) clinical staging for HIV disease in adults/ adolescents and children sorts patients into one of four hierarchical clinical stages ranging from stage 1 (asympto-matic) to stage 4 (AIDS) (Table 29.8). Patients are assigned to a particular stage when they demonstrate at least one clinical condition in that stage’s criteria. Patients remain at a higher stage after they recover from the clinical condition which placed them in that stage.
Centers for Disease Control and Prevention Surveillance Case Classification for AIDS
Patients with AIDS have been grouped as follows, according to the 1993 CDC Surveillance Case Classification:
Category A: Patients with acute symptoms or asymptomatic diseases as well as individuals with persistent generalized lymphadenopathy with or without malaise, fatigue, or low-grade fever.
Category B: Patients have symptomatic conditions such as oropharyngeal or vulvovaginal candidiasis, herpes zoster, oral hairy leukoplakia, or idiopathic thrombocytopenia, or consti-tutional symptoms of fever, diarrhea, or weight loss.
Category C: Patients are those with outright AIDS as mani-fested by life-threatening conditions or as identified by CD4+ T-lymphocyte levels of less than 200 cells/mm3.

Anti-retroviral therapy
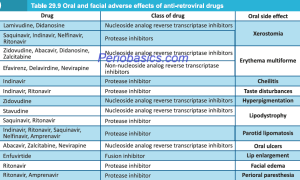
The anti-retroviral therapy has evolved tremendously since the introduction of zidovudine (AZT) which was approved by the US FDA in 1987. Zidovudine (AZT) is a nucleoside reverse transcriptase inhibitor (NRTI). Subsequently, more NRTI drugs were introduced, but even in combination, they were not able to suppress the virus for long periods of time and patients still inevitably died. With ……….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book………….Content available in book……..Presently, six classes of antiretroviral agents are used for the treatment of HIV infected patients,
- Nucleoside analog reverse transcriptase inhibitors (NRTIs): e.g. Lamivudine, Didanosine, Abacavir, Emtri-citabine, Zidovudine, Stavudine, and Tenofovir.
- Non-nucleoside analog reverse transcriptase inhibitors (NNRTIs): e.g. Efavirenz, Delaviridine, Etravirine, and Nevirapine.
- Protease inhibitors (PIs): e.g. Atazanavir, Darunavir, Saquinavir, Indinavir, Nelfinavir and Ritonavir.
- Integrase inhibitors (IIs): e.g. Dolutegravir and Ralte-gravir.
- Fusion inhibitors (FIs): e.g. Enfuvirtide and Maraviroc.
- Chemokine receptor antagonists (CCR5 antagonists): e.g. Aplaviroc, Vicriviroc, and Maraviroc
Conclusion
Viral infections of the oral cavity are significant due to their potential to cause discomfort, pain, and more severe health complications. The oral cavity, encompassing the lips, tongue, gums, and throat, is susceptible to a variety of viral pathogens. These infections can manifest in different forms, affecting individuals of all ages and varying in severity from mild discomfort to serious health issues. Understanding these infections involves recognizing their causes, symptoms, diagnosis, treatment, and preventive measures.
References
References are available in hardcopy of the website “Textbook of Basic sciences for MDS students”.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:

