Introduction
Fungi are important constituents of the normal microflora of the oral cavity. Like most of the bacterial species, they do not cause any disease in a healthy individual. Fungal infections are mostly observed in immunocompromised patients. In other words, we can say that these are opportunistic infections, which precipitate when the immune system of the patient is not able to control their growth. There are many predisposing factors for fungal infections, including certain drugs, nutritio-nal deficiencies, systemic diseases (such as uncontrolled diabetes mellitus, hypothyroidism, hypoparathyroidism, Addison’s disease) and infections like HIV. In elderly patients, one important cause of fungal infections is xerostomia, which leads to decreased levels of immunoglobulins in the saliva, lowering the efficiency of the humoral‑mediated immuno-logical defense mechanism for control of fungal infections, primarily Candidal infection. The commonly seen fungal infections and their causative species have been enumerated in Table 29.1.
In the following discussion, we shall read about various commonly encountered fungal infections in the oral cavity and their management.
Candidiasis
Candida species are the most common cause of fungal infections. Candida albicans is the most common species causing candidiasis. Candida glabrata, Candida parapsilosis, and Candida tropicalis are responsible for most of the remaining infections. Organisms such as Candida krusei, Candida lusitaniae, and Candida guilliermondii are less common causes of infection. Candida species are 2 to 6 µm yeast-like organisms that reproduce by budding. They are dimorphic fungus that can exist in both a yeast phase (blastospore, blastoconidial) and a hyphal (mycelial) phase. The oral Candida infection primarily presents in two forms: white lesions, in which hyphal forms are common (include thrush, candidal leukoplakia, and chronic mucocutaneous candidosis) and red lesions, in which yeast forms predominate (include denture-related stomatitis, median rhomboid glossitis, and erythematous candidosis).
Classification of candidiasis
The commonly used classification categorizes candidiasis into following types,
Pseudomembranous,
Erythematous,
Hyperplastic,
Candida-associated Lesions:
- Denture stomatitis,
- Angular cheilitis,
- Median rhomboid glossitis, and
- Linear gingival erythema.
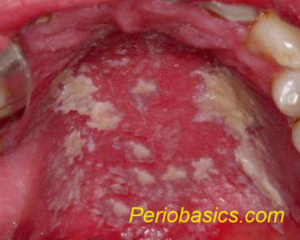
Acute pseudomembranous candidiasis (thrush)
This type of candidiasis is characterized by extensive white pseudomembranes consisting of desquamated epithelial cells, fibrin, and fungal hyphae. The patient presents with creamy white lesions on the oral mucosa, and a diagnostic feature of this infection is that these plaques can be removed by gentle scraping leaving behind an underlying erythematous mucosal surface. The oral surfaces frequently involved include labial and buccal mucosa, tongue, hard and soft palate, and oropharynx. The histological examination reveals desquamated epithelial cells together with yeast and filamentous forms of Candida. This condition is usually observed in patients with extremes of age, patients on prolonged corticosteroid therapy, immunocompromised patients, especially in AIDS, diabetics, prolonged broad-spectrum antibiotic therapy, and hematological and other malignancies.
Erythematous candidiasis:
Erythematous candidiasis is usually associated with a burning sensation in the mouth or on the tongue. It is the only form of candidiasis which is associated with pain. It is relatively rare and manifests as both acute and chronic forms. Erythematous candidiasis is most often associated with the use of broad-spectrum antibiotics or corticosteroids. The chronic form is usually seen in HIV patients involving the dorsum of the tongue and the palate and occasionally the buccal mucosa. On the tongue, this form of candidiasis typically presents as depapillated areas. Palatal lesions are more common in HIV patients.
Hyperplastic candidiasis
The hyperplastic candidiasis is the third clinical candidal variant which mainly presents as chronic form. It is also known as ‘candidal leukoplakia’. Many authors suggest that chronic hyperplastic Candida infection is associated with a diagnosis of dysplasia. It has been suggested that that up to 15% of all chronic hyperplastic candidal infections may prog-ress to dysplasia. Biopsy of suspected chronic hyperplastic candidiasis is recommended to rule out any dysplastic changes in epithelium. There are two clinical variants of the condition: homogeneous adherent white plaque-like or erythematous multiple nodular/speckled type. Commonly, the lesions are observed in the commissural region of the buccal mucosa and less frequently on ……….. Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…….

Candida-associated lesions
Denture stomatitis:
It is also referred to as “chronic atrophic candidiasis”. It is a chronic inflammatory condition of the denture-bearing mucosa and is considered to be the erythematous variant of candidal infection. The porosity of the acrylic allows for fungal and bacterial contamination in the denture. Clinical reports suggest that this condition is observed in around 50-65% of denture wearers. Clinically, the lesions appear as pinpoint hyperemia, diffuse erythematous or granular/papill-ary type. The lesions are commonly seen on the palate and mandibular mucosa is less commonly involved. Usually, these lesions are painless; however, some patients may complain of a burning sensation. This condition is often associated with angular cheilitis and median rhomboid glossitis. This condition is usually seen in patients not maintaining proper oral and denture hygiene, nocturnal denture wearers, patients with xerostomia and in cases of ill-fitting prosthesis.
Angular cheilitis:
Angular cheilitis is a mixed bacterial-fungal infection commonly noted at either or both corners of the mouth. The condition is characterized by erythematous or ulcerated fissures of the lips. Facial wrinkling along nasolabial folds and reduced occlusal vertical dimension are predisposing factors for the development of this condition because they promote a moist environment conducive to the growth of etiologic agents. Other causes of angular cheilitis include vitamin B12 deficiency and iron deficiency anemia.
Median rhomboid glossitis:
Median rhomboid glossitis is a chronic symmetrical area on the tongue, anterior to the circumvallate papillae. It is made up of atrophic filiform papillae. Clinically, it manifests as a well-demarcated, symmetric, depapillated area arising anterior to the circumvallate papillae. The surface of the lesion can be smooth or lobulated. This lesion is commonly observed in smokers and patients using steroid inhalers.
Linear gingival erythema:
This condition is typically seen in HIV infected patients. It was previously referred to as “HIV-gingivitis”. Clinically, the condition manifests as linear erythematous band of 2-3 mm on the marginal gingiva. Along with this, petechial or diffuse erythematous lesions can also be present on the attached gingiva. Recent investigations suggest that along with C. albicans, C. dubliniensis is also associated with the etiology of this condition.
Many systemic diseases which are associated with immunodeficiency may have candidiasis as a secondary manifestation. These diseases include Di George syndrome, hyper-immunoglobulin E syndrome, Nezelof’s syndrome MPO deficiency, SCID syndrome and endocrine disorders like Addison’s disease and hypoparathyroidism.
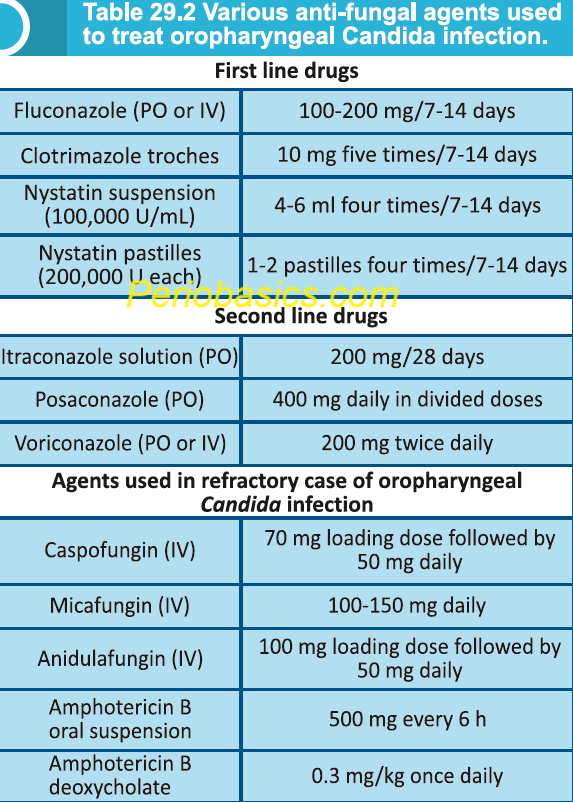
Management of oral candidiasis
The suggested protocol for the management of candidiasis is as follows,
1. Diagnosis through detailed medical and dental history, clinical manifestations confirmed with laboratory tests.
2. Correction of predisposing factors where achievable.
3. Maintenance of proper hygiene of the oral cavity and oral prostheses, if any.
4. Selection of antifungal therapy based on the severity of the infection and susceptibility of the Candida species prevalent in that patient.
The diagnosis of the Candida infection and determination of its type is the first and foremost step in the management of the case. A detailed case history of the patient should be recorded and the etiology of the diseases should be established. Along with the treatment of the infection, it is also important to treat the underlying cause of the disease. If the infection is present in the immunocompromised patient, the reason for depressed immune response should be identified and treated appropriately. The diagnosis of Candia infection is confirmed by obtaining a smear from the lesion or biopsy examination showing ……….. Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…….
Blastomycosis
Blastomycosis is caused by Blastomyces dermatitidis, a thermally dimorphic fungus that grows as a mold in the environment and as a yeast in tissues. Infection occurs mainly via the respiratory tract. The conidia produced in the environmental mold phase cause infection when aerosolized and inhaled into the alveoli, where conversion to the yeast phase occurs. From the lungs, the fungus can spread to other areas of the body, including skin, bones, joints and central nervous system. In the lung, the phagocytic actions of alveolar macrophages, neutrophils, and monocytes provide natural resistance to infection with conidia of B. dermatitidis. In addition, alveolar macrophages have been shown to inhibit the transformation of conidia to the pathogenic yeast form. It should be noted here that the ability to convert from mold to yeast is an essential event in the pathogenesis of B. dermatitidis. Almost 50% of cases with B. dermatitidis infections are asymptomatic. In symptomatic patients, illness typically begins 30 to 45 days after exposure manifesting as a mild self-limited pulmonary infection or ”summer cold.” In severe cases with respiratory infection, patients complain of cough (most common symptom), followed by fever, night sweats, weight loss, chest pain, dyspnea, myalgias, and hemoptysis. Chest radiographs reveal a patchy pneumonitis, a mass-like infiltrate, or nodules. It should be noted here that ……….. Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book……. Genitourinary tract involvement is common in men and the prostate is the usual target organ. The severe form of the disease is associated with involvement of CNS manifesting as meningitis, brain abscesses, and cord lesions. CNS involvement is usually seen in immuno-compromised patients. The diagnosis is made by examining stained clinical specimens and culturing. The culture of Blastomyces provides a definitive diagnosis.
Management
Treatment depends on the severity of the disease. All patients with chronic pulmonary or disseminated extrapulmonary blastomycosis and all immunocompromised patients with blastomycosis should receive antifungal therapy. The recommended protocol for treatment of blastomycosis has been ……….. Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book……..
Cryptococcosis
In humans, this disease is caused by two Cryptococcus spec-ies, namely, Cryptococcus neoformans and Cryptococcus gattii. C. neoformans infection generally affects immuno-compromised hosts. The organism is acquired by inhalation of spores found in soil, specially excreta of birds like pigeons, canaries, parrots, and rotting fruit and vegetables. The incubation period ranges from 2 to 13 months and pulmonary disease may precede brain infection by months or years. Remarkably, Cryptococcus is the only eukaryotic pathogen that produces a polysaccharide capsule, which serves as the major virulence factor. Cryptococcosis may present as ……….. Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book……. Diagnosis is by direct observation of the causative agent, in histopathologic studies, by isolation in culture, and by the presence of the capsular antigen.
Management
The immunocompetent patients who present with mild to moderate symptoms should be treated with fluconazole, 200 to 400 mg/day for 6 to 12 months. In severe or progressive disease, amphotericin B is recommended, 0.4 to 0.7 mg/kg/day for a total dose of 1-2 gm. In case of suspicion of CNS infection, it is essential to examine the cerebrospinal fluid (CSF) before the treatment is started. Patients with cryptococcal meningitis often present with severe disease. The treatment protocol includes a combination of amphoteri-cin B (0.7-1mg/kg/day or the more expensive lipid formulation in the case of renal impairment) and oral flucytosine (100 mg/kg/day) for 2 weeks, followed by fluconazole (400 mg/day) for a minimum of 8 weeks.
Histoplasmosis
Histoplasmosis is an infection resulting from the inhalation of spores belonging to the fungus Histoplasma capsulatum. The disease is also known as “Reticuloendotheliosis”, “Caver’s Disease” and “Ohio Valley disease”. It is the most common endemic mycosis which causes infection. Histoplasma capsulatum is found in soil rich with excreta of bats and birds. After inhalation of the spores, the conidia are recognized and phagocytized by resident macrophages in the alveolar space. Inside the macrophages, conidia convert into yeast, which is a necessary step in the pathogenesis of histoplasmosis. During the first couple of weeks, histoplasma yeasts multiply inside alveolar macrophages and spread throughout the reticulo-endothelial system. Majority of the patients infected with H. capsulatum are asymptomatic or minimally symptomatic. In symptomatic patients, the symptoms include fever, chills, headache, dry cough, chest discomfort, and muscle aches. Less commonly joint pain and rash can develop. The fungus presents the greatest threat to those who are ……….. Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…….
Management
In most cases of pulmonary histoplasmosis, treatment is not recommended because the degree of exposure is not heavy; the infection is asymptomatic or symptoms are mild, subacute, and not progressive; and the illness resolves without therapy. Treatment is indicated in all symptomatic patients with acute pulmonary histoplasmosis causing diffuse infiltrates, especially with hypoxemia and in patients with chronic pulmonary and disseminated histoplasmosis.
Paracoccidioidomycosis
Paracoccidioidomycosis is caused by Paracoccidioides brasi-liensis. It is considered to be the most important systemic fungal infection affecting countries in South America. It is a soil fungus that undergoes a dimorphic switch following host inhalation. In its mycelial form, Paracoccidioides species appear as thin septated hyphae with occasional chlamydo-spores and conidia. In the yeast form, Paracoccidioides species are characterized by oval or round budding yeast cells of varying sizes (4 to 40 microns). The typical appearance is that of a large mother cell surrounded by multiple budding daughter cells known as blastoconidia. The primary pulmo-nary infection is usually unapparent and the individual may remain infected throughout the lifetime without developing symptoms. Once in the host, the fungus converts into its yeast form, and this process is regarded as a fundamental step for the successful establishment of the infection.
The disease may manifest itself in acute, subacute or chronic forms. The acute or subacute forms of the disease can occur in young individuals, generally developing from a primary undetected pulmonary lesion that evolves quickly with lymphatic and hematogenous spread to organs of the monocyte-macrophage system, such as spleen, liver, lymph nodes, bones and bone marrow, leading to a significant deterioration of the patient’s clinical condition. On the other hand, a chronic infection develops from the primary pulmonary complex or from the reactivation of a quiescent pulmonary or metastatic focus. Most cases begin in the lungs and progress slowly; they are usually observed in adult males over 30 years of age, presenting prolonged duration, typically over six months of clinical history, and often expressed by pulmonary and tegumental (cutaneous and/or mucosal) damage.
Management
Paracoccidioides brasiliensis is very sensitive when exposed to anti-fungal drugs. Even sulfonamides can inhibit its growth. So there is a large therapeutic armamentarium to treat Paracoccidioidomycosis. The drugs of choice include sulfona-mides (sulfadiazine, sulfadoxine, sulfamethoxypyri-dazine, cotrimazine, and trimethoprim-sulfamethoxazole), ampho-tericin B, azoles (eg, ketoconazole, itraconazole, fluconazole, voriconazole, and posaconazole), and terbinafine (Table 29.5).
Coccidioidomycosis
Coccidioidomycosis is caused by Coccidioides immitis, a soil fungus. The infection is acquired by inhaling spore-laden dust. Once inhaled, C. immitis spores convert to large tissue-invasive spherules. As spherules enlarge and then rupture, each releases thousands of small endospores, which may form new spherules. Pulmonary disease is characterized by an acute, subacute, or chronic granulomatous reaction with varying degrees of fibrosis. Lesions may cavitate or form nodular-like coin lesions. In severely immunocompromised patients, there may be widespread involvement of the lungs and/or systemic dissemination. Coccidioidomycosis is a recognized opportunistic infection among HIV-positive persons. Oral lesions are uncommon and have been described as ulcerated granulomatous nodules. Clinically, the ulcers appear nonspecific and usually ……….. Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…….
Management
The clinical presentation of coccidioidomycosis varies from mild respiratory syndrome, or an uncomplicated community-acquired pneumonia to progressive pulmonary destruction or lesions in other parts of the body. Because the severity varies widely, the optimal management strategies also vary widely among individual patients. The majority of patients who present with early infections will resolve their infection without specific antifungal therapy. However, their manage-ment should routinely include repeated assessment of the patient every 3-6 months for up to 2 years. Patients who develop severe pneumonia need systemic antifungal therapy. Along with this, patients who develop chronic pulmonary or disseminated disease also require antifungal therapy. Specific antifungal drugs and their usual dosages for treatment of coccidioidomycosis include amphotericin B deoxycholate (0.5-1.5 mg/kg per day or alternate day administered intravenously), lipid formulations of amphotericin B (2.0-5.0 mg/kg or greater per day administered intravenously), ketoconazole (400 mg every day administered orally), fluconazole (400-800 mg/day administered orally or intravenously), and itraconazole (200 mg twice per day or 3 times per day administered orally) (Table 29.6).
Mucormycosis
Mucormycosis (also known as zygomycosis), refers to several different diseases caused by infection with fungi in the order Mucorales. Rhizopus species are the most common causative organisms. In descending order, the other genera with mucormycosis-causing species include Mucor, Cunningha-mella, Apophysomyces, Lichtheimia (formerly Absidia), Saksenaea, Rhizomucor, and other species. The infection is more common among people with weakened immune systems, but it can occur (rarely) in people who are otherwise healthy. The risk factors for developing mucormycosis include uncontrolled diabetes, cancer, organ transplant, neutropenia and skin trauma (cuts, scrapes, punctures, or burns). The infection is acquired by inhalation of the spores from the air. Symptoms of pulmonary mucormycosis include fever refractory to antibiotics, cough, pleuritic chest pain, and dyspnoea. Invasion of blood vessels can lead to fatal hemoptysis. Invasive mucormycosis is characterized by ……….. Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book…………… Content available in book……. Preliminary diagnosis is made by patient history, physical examination, and the patient’s risk factors for mucormycosis. Histopathological examination of surgical specimens can confirm the clinical diagnosis.
Management
The therapeutic approach to mucormycosis is multimodal, including antifungal agents, surgical debridement, and correction of the underlying condition predisposing the patient to the disease. The recent therapeutic developments in mucormycosis treatment are the lipid formulations of amphotericin B, which are now the drugs of choice.
Conclusion
Oral fungal infections, also known as oral mycoses, are infections in the mouth caused by fungi. Oral fungal infections have been around since the days of Hippocrates (around 460-370 BCE). At present we have an in depth knowledge about the mechanism of oral fungal infections. However, many aspects still need to be investigated. The most common type of oral fungal infection is oral candidiasis (thrush), which is caused by Candida species, particularly Candida albicans. Recent advancements in the field of microbiom analysis has further elaborated our knowledge regarding these diseases. Oral fungal infections are usually treatable with appropriate antifungal therapy and good oral hygiene practices. Along with this, patient awareness is very important to restrict these infections.
References
References are available in the hardcopy of the website “Textbook of Basic sciences for MDS students”.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:

