Introduction
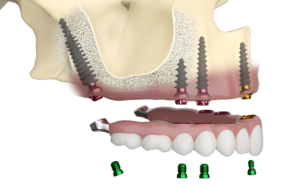
Pterygoid implants are used in dental procedures to provide support in the posterior maxilla, particularly in cases where traditional implant placement is challenging due to bone resorption or sinus pneumatization. These implants engage the pterygoid plates of the sphenoid bone, offering several advantages such as avoiding sinus augmentation and providing immediate load-bearing capacity. The pterygoid plate, part of the sphenoid bone, serves as the placement site for these implants. These implants are anchored at a 45-degree angle into the pterygoid bone.
Anatomical considerations
The pterygoid processes are paired posteroinferior projections of the sphenoid bone. The process bifurcates into two parts; the medial pterygoid plate which is the inner part of the process and lateral pterygoid plate which is the outer part of the process. Let us discuss the important anatomical structures related to placement of pterygoid implants,
Pterygoid process of the Sphenoid Bone:
Medial and Lateral Pterygoid Plates: The pterygoid implants are anchored into these bony plates.
Pterygoid Hamulus: Serves as a landmark for the correct placement of the implant.
Maxilla:
Posterior Maxilla: The area of the upper jaw where bone loss often necessitates the use of pterygoid implants.
Maxillary Tuberosity: The rounded posterior end of the alveolar process of the maxilla, located near the pterygoid process.
Pterygomaxillary Fissure:
A vertical gap between the maxilla and the pterygoid process. The implant placement should avoid encroaching into this space to prevent damage to neurovascular structures.
Pterygopalatine Fossa:
A cone-shaped depression deep to the pterygomaxillary fissure, containing important neurovascular structures such as the maxillary artery and the maxillary nerve (a branch of the trigeminal nerve).
Implant Placement Considerations
Anatomical Landmarks: Precise knowledge of the anatomical landmarks is crucial for avoiding complications. The implant is placed posteriorly through the maxillary tuberosity and directed towards the pterygoid process.
Length and Angle: Pterygoid implants are typically longer than conventional implants and are placed at an angle to maximize contact with dense cortical bone of the pterygoid plates.
Avoiding Vital Structures: Care must be taken to avoid the pterygopalatine fossa and the maxillary sinus, as well as ensuring the implant does not impinge on the neurovascular contents of these areas.
Treatment planning for pterygoid implants
Patient Assessment
Medical History: Review the patient’s medical history to identify any contraindications for implant surgery, such as uncontrolled diabetes, osteoporosis, or conditions that affect bone healing.
Dental History: Assess previous dental treatments, particularly any history of maxillary sinus issues or previous implant failures.
Clinical Examination: Conduct a thorough intraoral examination to evaluate the condition of the oral mucosa, the presence of any pathology, and the extent of alveolar ridge resorption.
Radiographic Evaluation
Cone Beam Computed Tomography (CBCT): Obtain CBCT scans to evaluate the quality and quantity of bone in the pterygoid region, the position of the maxillary sinus, and the proximity of critical anatomical structures like the maxillary artery and the pterygopalatine fossa.
Panoramic Radiographs: Useful for a broad overview but less detailed than CBCT.
Planning the Implant Position
3D Planning Software: Use specialized software to simulate implant placement. This allows for precise planning of the implant trajectory, angle, and depth to maximize bone contact and avoid critical structures.
Surgical Guide: Consider using a custom surgical guide based on the 3D planning to assist in accurate implant placement during surgery.
Surgical Procedure
Pre-Surgical Preparation: Ensure sterile conditions and appropriate anesthesia. Preoperative antibiotics and anti-inflammatory medications may be administered.
Incision and Flap Design: Make a careful incision and reflect a mucoperiosteal flap to expose the maxillary tuberosity and the posterior maxilla.
Osteotomy Preparation: Use sequential drills to prepare the osteotomy site. The preparation should be done with great care to avoid overheating the bone and damaging adjacent structures.
Implant Insertion: Insert the pterygoid implant at the planned angle and depth. The implant should engage the cortical bone of the pterygoid process for stability.
Flap Closure: Suture the flap back in place, ensuring tension-free closure to promote healing.
Post-Surgical Care
Immediate Post-Operative Instructions: Provide instructions on diet, oral hygiene, and activity restrictions. Prescribe appropriate pain management and antibiotics as necessary.
Follow-Up Visits: Schedule regular follow-up visits to monitor healing and detect any signs of infection or complications early.
Prosthetic Rehabilitation
Healing Period: Allow adequate time for osseointegration, which may vary depending on the patient’s bone quality and overall health.
Prosthetic Phase: Once osseointegration is confirmed, proceed with the prosthetic phase. This involves taking impressions and fabricating the final prosthetic restoration.
Final Restoration: Attach the prosthetic restoration to the implants, ensuring proper fit, occlusion, and esthetics.
Advantages of pterygoid implants
Stability: Pterygoid implants provide enhanced stability for dental prostheses in patients with significant posterior maxillary bone loss, reducing the need for bone grafting procedures.
Function: They restore masticatory function and improve the quality of life for patients with severe maxillary atrophy or resorption.
Complications associated with pterygoid implant placement
While pterygoid implants offer a solution for patients with severe maxillary bone loss, their placement is associated with specific complications due to the complex anatomy of the area. Here are some potential complications:
Intraoperative Complications
Hemorrhage: The pterygoid region is close to significant vascular structures, such as the maxillary artery. Accidental injury to these vessels can cause severe bleeding.
Nerve Damage: The posterior superior alveolar nerve and branches of the maxillary nerve run near the implantation site. Injury to these nerves can result in paresthesia or anesthesia.
Maxillary Sinus Perforation: The implant may accidentally penetrate the maxillary sinus, leading to sinusitis or other sinus complications.
Postoperative Complications
Infection: As with any surgical procedure, there is a risk of postoperative infection. This can be mitigated with proper aseptic techniques and postoperative care.
Implant Failure: Osseointegration may fail due to poor bone quality, inadequate initial stability, or biomechanical overload.
Pain and Swelling: Postoperative pain and swelling are common and usually managed with analgesics and anti-inflammatory medications. However, excessive or prolonged symptoms may indicate complications.
Long-Term Complications
Peri-Implantitis: Inflammation of the tissues around the implant can lead to bone loss and implant failure. This risk is increased with poor oral hygiene.
Prosthetic Complications: Issues such as loosening of the prosthetic components, occlusal discrepancies, or prosthetic fractures may occur and require adjustment or repair.
Specific Anatomical Complications
Pterygoid Plexus Injury: The pterygoid plexus of veins is located in the vicinity of the implant site. Injury to this plexus can result in significant bleeding and hematoma formation.
Pterygopalatine Fossa Encroachment: Incorrect implant placement can encroach into the pterygopalatine fossa, potentially damaging the neurovascular contents, leading to serious complications such as excessive bleeding or nerve damage.
Conclusion
Effective treatment planning for pterygoid implants requires a comprehensive approach that includes detailed patient assessment, meticulous radiographic evaluation, precise surgical planning, and thorough post-operative care. By following these steps, clinicians can achieve successful implant outcomes, providing patients with stable and functional dental restorations.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:

