Introduction
The primary etiology of periodontal diseases is various periodontopathogenic bacteria and their products. Plaque formation and maturation is the first step in the initiation of the periodontal disease process. The calcified plaque or calculus harbor plaque on its surface, thereby facilitating more plaque accumulation. Historically, it was well understood that achieving plaque and calculus free root surface is the prime requirement for periodontal health. So, initial surgical procedures were primarily designed to get access to the diseased root surface, whereas, later on with the passage of time surgical procedures were aimed at achieving clean root surface along with the removal of diseased gingival tissue. Furthermore, it was believed earlier that crestal bone adjacent to the periodontal pocket was infected. So, the initial surgical procedures were resective, aimed at removing the diseased tissue with crestal bone. As these techniques did not adequately address esthetic concerns so, new techniques were introduced which, along with the removal of the infected tissue also maintained good esthetics.
Periodontal surgical procedures have come ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Know More…
Classification of periodontal flaps:
Historically, flap surgeries have been classified by various authors. Ramfjord (1979) classified periodontal flap surgeries, according to the main purpose of the procedure such as pocket elimination flap, reattachment flap surgery, and mucogingival repair. Carranza (1979) classified flap as full-thickness flap and partial-thickness flap. Full-thickness flap is the flap where all the soft tissue along with the periosteum are reflected. Partial or split-thickness flap is an elevated flap which includes only epithelium and the layer of underlying connective tissue. The periosteum overlying the bone is not elevated in partial-thickness flap.
Later on, in 1990 Carranza classified flaps according to their final positioning. He classified them as repositioned /positioned/displaced flaps where the flap is placed apical, coronal, or lateral to its original position and un-reposition or un-replaced flap where the flap is sutured exactly at the same position as it was present before the procedure.
Historical aspect of surgical periodontal pocket therapy
As stated above, the initial surgical procedures to reduce probing depth in periodontitis cases employed resective methods. These surgical procedures established the gingival margins apical to their original position, thereby achieving healthy periodontium at a reduced level. It was believed that the destruction that has already occurred is irreversible and cannot be reversed.
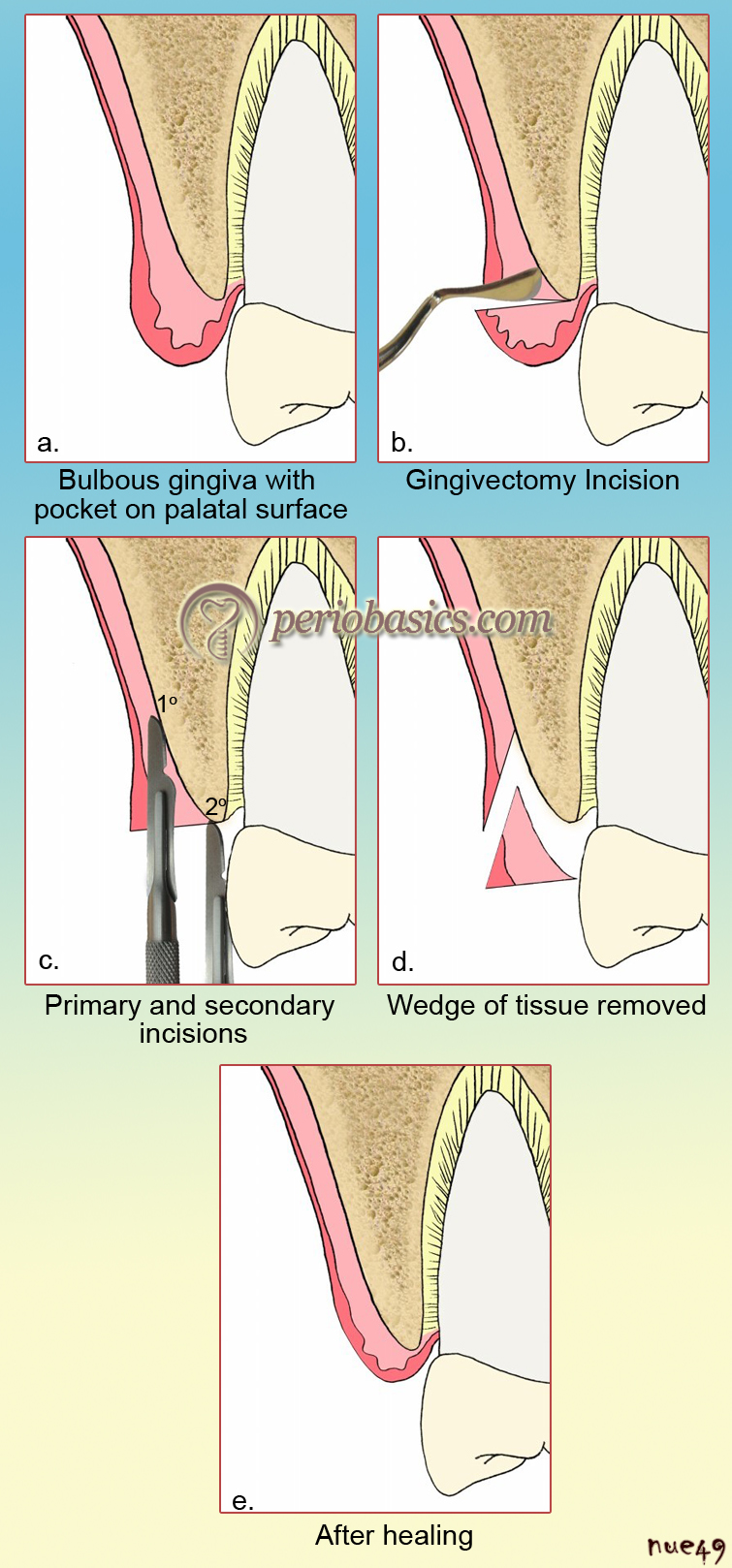
The earliest form of periodontal resective surgical procedures was ‘gingivectomy’. It was Pierre Fauchard 1 in 1742, who specifically designed instruments for resecting excessive tissue and crestal bone. This procedure was modified by Robicsek 2 in 1884 and later on Pickerill 3 in 1912 termed this procedure “Gingivectomy”. Zentler 4 in 1918 modified the procedure by advocating scalloped incision to achieve fine gingival margins after healing. Other authors that contributed and modified gingivectomy procedure include G V Black 5, Ward 6, and Crane and Kaplan 7. The procedure described by Ward, known as “the obliteration method” was ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
The gingivectomy procedure as it is employed today was described in 1951 by Goldman.

The concept that prevailed at that time was that bone adjacent to the periodontal pocket was either infected or necrotic and should be removed. So, these researchers advocated the removal of the crestal bone during the gingivectomy procedure. It was Kronfeld 8 in 1935, who in an autopsy study showed that bone adjacent to the periodontal pockets was neither necrotic nor infected but rather destroyed by an inflammatory process. These findings were further supported by Orban 9. Now, the focus shifted on ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
A periodontal flap is a section of the gingiva and/or mucosa, surgically separated from the underlying tissues to provide visibility of and access to the bone and root surfaces. Flap surgeries are resective procedures introduced during the beginning of the 20th century. Neumann (1920) 10 claimed the introduction of the mucoperiosteal flap in 1911. The procedure involved an intrasulcular incision and two releasing incisions on both sides of the defect area, involving up to 6 teeth. The flaps were raised up to the mucobuccal fold on both buccal and lingual aspect. Approximately 2 mm of gingival margin and bone was removed in the areas of deep pockets. The flaps were sutured back in their original position. Neumann described his technique as “the radical treatment of alveolar pyorrhea.”
Widman in 1916 presented a modification of Neumann’s flap to the Scandinavian Dental Association, which was published in 1918. He claimed that he had been performing this procedure as early as 1911. The procedure involved elevation of the trapezoidal flap with two vertical releasing incisions at the midline of the teeth and a reverse bevel incision made parallel to the surfaces of the teeth, 1 mm from the free gingival margin, extending to the ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………

Cieszynski (1914) 11 is credited with the introduction of the reverse bevel incision in the periodontal flap operation. It is important to note here that all the above-described procedures were radical as they advocated thorough scaling, removal of granulation tissue and removal of bone because it was believed that bone adjacent to pocket was either infected or necrotic.
As stated earlier, studies by Kornfeld 8 and Orban 9 showed that the bone adjacent to the pocket was neither infected nor necrotic but lost due to inflammation. So, surgical procedures proposed after their findings did not include unnecessary removal of the bone. Now, the focus shifted on preserving the healthy tissue and achieving good esthetic results. As stated earlier, gingivectomy became popular at this time as it completely removed the periodontal pocket consistently. But, problems associated with this procedure included excising the attached gingiva, the frenum attachment, and the creation of shallowed vestibular depth.
Know More…
Pocket elimination/pocket reduction or maintenance procedures:
Pocket elimination procedures:
The surgical procedures which completely eradicate the periodontal pocket are termed as pocket elimination procedures. Now, how can a pocket be completely eliminated? One procedure is the complete excision of the tissue supporting the pocket (Gingivectomy). The other procedure is positioning the margin of the gingiva at the base of the pocket, thereby creating healthy gingival tissue at a reduced level (Apically positioned flap). The main disadvantages of these procedures include ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Pocket reduction or maintenance procedures:
The surgical procedures which do not completely eradicate the pocket, but reduce pocket depth or maintain it with healthy tissue are termed as pocket reduction or maintenance procedures. These include procedures like, modified Widman flap or Kirkland flap, where the pocket lining is removed keeping the healthy tissue intact. These procedures, unlike pocket elimination procedures, do not cause unwanted root exposure (recession).
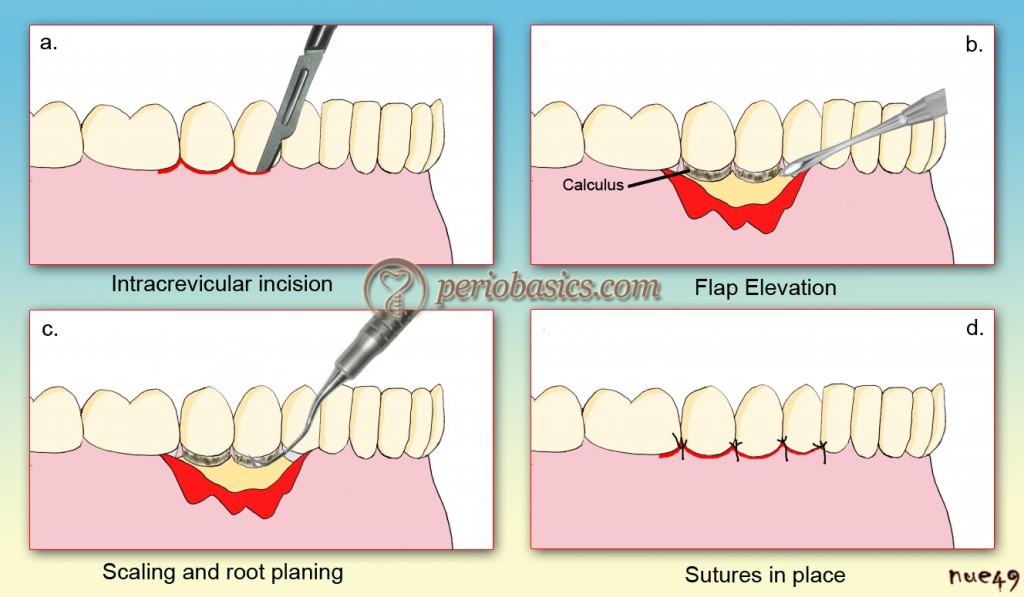
Kirkland (1931) 12 in 1931 published a flap procedure which he called the “modified flap operation”. In this procedure, incisions were made intracrevicularly through the bottom of the pocket on both the labial and lingual aspects of the interdental area. After elevation of the flap, the root surfaces were scaled. The pocket lining and the granulation tissue are ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Nabers 13 in 1954, introduced “apically repositioned flap”. The procedure was named as “repositioning of the attached gingiva.” He described this procedure with only one vertical releasing incision, which was placed mesially to the area of the deepest pocket. After raising the mucoperiosteal flap, teeth were thoroughly scaled, all granulomatous tissue was removed, the flap was curetted and the gingival margins were trimmed up to the depth of at least 2 mm. Now, the flap was positioned apically to the crest of the bone and sutured loosely. This procedure accomplished the complete elimination of periodontal pocket as well as maintenance of existing attached gingiva. In 1957, Nabers modified the procedure by adding ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
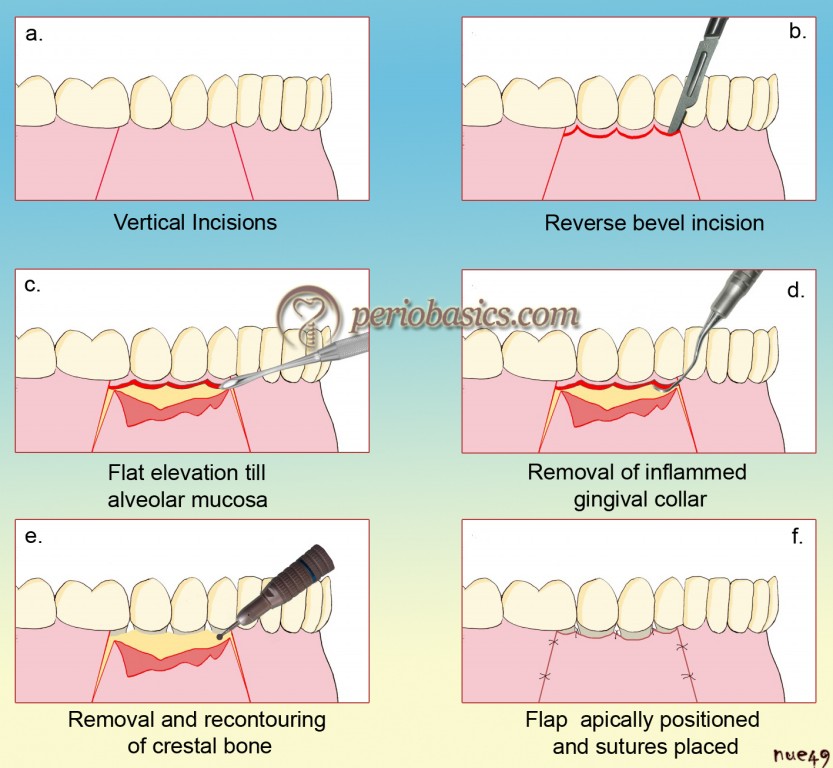
Ariaudo and Tyrrell (1957) 14 in the same year, modified Nabers’ technique by using 2 vertical releasing incisions. It provided greater flexibility and easy manipulation of the flap. Friedman (1962) 15 in 1962 explained the surgical technique and coined the term “apically repositioned flap”. Presently, the term “reposition” is not used as repositioning means placing the flap at its original position; instead, term “position” is used. The major advantages of this procedure are reduction of probing depth, preserving or increasing the pre-surgical zone of gingiva, facilitation of healing, better accessibility to the crestal bone, root surfaces, furcations, subgingival caries and other anatomical aberrations. Major disadvantages associated with this procedure are esthetic problems due to root exposure, which may cause root sensitivity and inability to treat infra-bony pockets.
Ochsenbein 16 in 1958 explained the modified partial-thickness palatal flap. The technique for this procedure was re-described by Ochsenbein and Bohannan in 1963 and later on popularized by Prichard in 1965. It is commonly known as “ledge and wedge technique”. It is indicated in palatal areas with thick mucosa where along with a pocket-depth reduction, thinning of the flap is required. The procedure includes marking the pocket depth on palatal gingiva with the help of probe or pocket marker and making an external bevel incision in such a way that a ledge of the tissue is formed. Now, two incisions are given: a primary incision is made to raise a partial-thickness flap and a secondary incision is made along ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
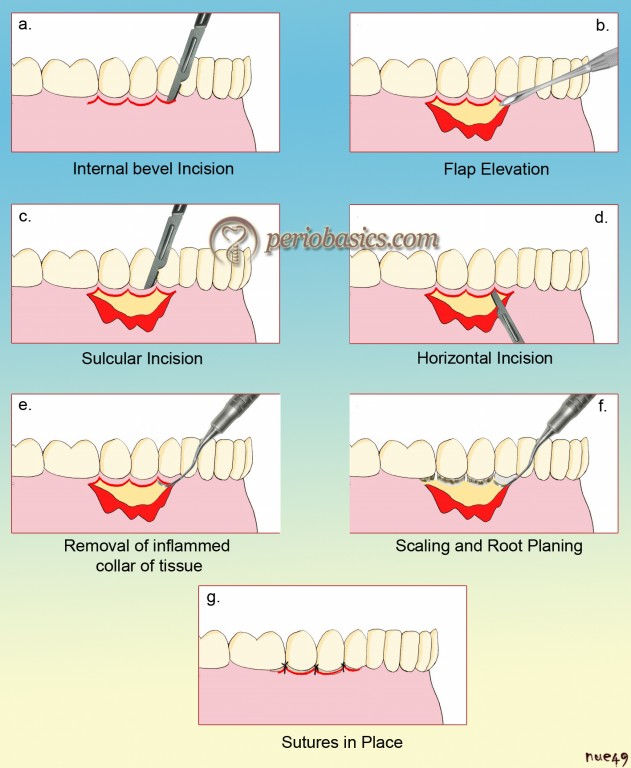
Ramfjord and Nissle (1974) 17 in 1974, modified the original Widman flap procedure and coined the term “Modified Widman flap”. Essentially, the same procedure was employed by Morris 18 in 1965 who termed it as “the un-repositioned mucoperiosteal flap”. The procedure was described as “the simple mucoperiosteal flap, combined with the inverted beveled incision and osseous resection.” The modified Widman flap utilized three incisions. The first incision is the internal bevel incision. This incision is directed apically, starting 0.5 to 1 mm away from the gingival margin towards the alveolar bone crest following the gingival margin scalloping. During making an incision, care should be taken to insert the blade in such a way that the papilla is left with a thickness similar to that of the remaining facial flap. The second incision is called as crevicular incision which starts from the bottom of the pocket to the bone, circumscribing the triangular wedge of tissue containing the pocket lining. Finally, the third incision or the horizontal incision is placed in the interdental spaces, coronal to the bone and then with a curette or an interproximal knife, the gingival collar is removed.
The flap procedure usually causes interdental soft tissue recession. To preserve the interdental soft tissues and for maximum soft tissue coverage following surgical intervention a new technique “papilla preservation flap technique” was introduced by Takei et al. (1985) 19. Later on Cortellini et al. (1995, 1999) 20, 21 described modifications of the flap design to be used in combination with regenerative procedures. The procedure involved the inclusion of the interdental papilla in the incision line. The intrasulcular incision is extended to make a semilunar incision interdentally on the ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Know More…
Gingival curettage:
Gingival curettage refers to the scraping of gingival wall of periodontal pocket to remove the inflamed soft tissue. Subgingival curettage refers to procedure that is performed apical to junctional epithelium in which the connective tissue attachment is severed down to osseous crest. The primary objective of this procedure is to reduce pocket depth by enhancing gingival shrinkage and new connective tissue attachment.
Clinical procedure:
As this procedure does not eliminate the etiological factors of inflammation (such as bacterial plaque, calculus), so it should always be preceded by scaling and root planning. The area to be operated is anesthetized with local anesthesia spray or injection. A curette is adapted against the soft tissue wall of the involved tooth. The instrument is inserted so ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Present status:
This procedure was originally aimed at reducing the pocket depth by enhancing gingival shrinkage and new connective tissue attachment. However, most of the studies have reported that the end result of this procedure is the formation of long junctional epithelium, which is the same result, obtained from scaling and root planing. Furthermore, it is a blind procedure. This procedure offers no additional benefit when compared with scaling and root planing alone 45.
Deep periodontal pockets on the distal aspect of last molars are difficult to treat due to the presence of bulbous tissues over the tuberosity or a prominent retromolar pad. Robinson (1966) 22 in 1966 published “distal wedge procedure” to access the bone defect distal to the last molars and preserve a sufficient amount of gingiva to achieve soft tissue coverage.
R A Yukna in 1976 23 described a surgical procedure, “excisional new attachment procedure (ENAP)” where the sulcular and junctional epithelium is resected with a knife. The aim of the procedure is to remove the diseased tissue and allow healing of the dentogingival and periodontal attachments. It is a definitive subgingival curettage procedure performed with a knife. The procedure involves making an internal bevel incision from the margin of free gingiva apically to a point below the bottom of the pocket both on buccal and lingual aspect. This incised tissue containing pocket wall is then removed with a curette.
In recent years, with the introduction of LASER, new treatment procedures have been introduced in periodontal surgical therapy. The Laser-assisted New Attachment procedure (LANAP), is a LASER assisted pocket therapy, which has recently been approved by the US food and drug administration. The objective of LANAP laser therapy is pocket reduction achieved by establishing a new connective tissue attachment to the tooth at a more coronal level. The major advantage of LANAP therapy is that it allows us to treat periodontal disease with a minimally invasive procedure which eliminates the need of conventional blade surgery in most cases. The procedure involves the application of a free-running pulsed Nd:YAG laser beam in the ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Historical aspect of osseous resective surgery
As already described, the initial periodontal surgeries involved removal of superficial radicular and interproximal alveolar crestal bone, considering it to be necrotic or infected. So, the earlier rationale for osseous surgery was that the bone surface was considered infected or necrotic and had to be removed. During gingivectomy, denudation of the radicular and interproximal crestal bone followed by some osseous removal was advocated by pioneers in periodontal surgeries which included S Robicsek, GV Black, AD Black, A Crane, H Kaplan, A Ward and W Ziesel.
The pioneers in the flap surgery such as R Neumann, A Cieszynski and A Zentler, also advocated the removal of bone because its surface was considered to be necrotic or infected. As already discussed, the landmark work done by Kronfeld (1935) 8 and Orban (1939) 9 showed that ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Carranza in 1989 42 re-described osseous resective surgery with a rationale of recontouring the bone to facilitate the reduction of pockets by allowing the gingival tissues to follow a more physiological contour. S Schluger (1949) 43 is credited with outlining the “principles of osseous surgery” where he described the clinical procedure for recontouring the bone, facilitating predictable elimination or reduction in pocket depth and its maintenance in the long term. Other clinicians who popularized osseous resective surgery include J Prichard, N Friedman and C Ochsenbein.
It is important to know a few terms in osseous resective surgery. These are osseous surgery, osteoplasty, and ostectomy. In the third edition of the American Academy of Periodontology’s Glossary of periodontal terms 44, these have been defined as,
- Osseous surgery: periodontal surgery involving modification of the bony support of the teeth.
- Osteoplasty: reshaping of the alveolar process to achieve a more physiological form without removal of the supporting bone.
- Ostectomy: the excision of bone or a portion of the bone. In periodontics, ostectomy is done to correct or reduce deformities caused by periodontitis in the marginal and intra-alveolar bone and includes the removal of supporting bone.
Siebert (1976) 46 described the advantages of resective osseous surgery. These are,
- The simplicity of procedure.
- Minimal treatment time.
- Visualization of the osseous defect.
- Elimination of additional surgical sites.
- The major disadvantage of this procedure is the loss of attachment.
Review of literature on surgical periodontal pocket therapy
Many investigations have been done to find out the outcome of various surgical pocket therapies. A few of them have been summarized below,
Healing after gingivectomy:
Listgarten (1972) 47 studied healing after gingivectomy in monkeys. He demonstrated that the complete re-establishment of junctional epithelium takes place as early as 12 days post-operatively. Donnenfeld and Glickman (1986) 48 in ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Key elements in the success of surgical therapy:
Ramfjord (1977) 49 reviewed the present status of modified Widman flap and stated that the key elements in the success of surgical therapy are the creation and maintenance of biologically acceptable root surface. He also enumerated the advantages of modified Widman flap which include, access to the root surface, esthetic results, fewer chances of root sensitivity and root caries and favorable environment for oral hygiene maintenance.
Comparison of different surgical procedures:
Rosling et al. (1976) 50 conducted a 2 year clinical trial where they compared apically positioned flap, apically positioned flap and osseous surgery, Widman flap, Widman flap and osseous surgery for their healing and pocket-depth reduction. Results showed that all the procedures were effective in reducing the pocket depth to various levels. Gingivectomy cases showed a reduced pocket depth, the greatest reduction in alveolar bone height and least regeneration in intrabony defects.
Becker et al. (1988) 51 in a longitudinal study compared scaling and root planing (SRP), apically positioned flap with osseous surgery and modified Widman procedures for pocket depth reduction. A split-mouth design was used. After one year, the surgery resulted in greater pocket depth reduction in the 4 to 6 mm and > 7 mm groups than the ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Isidor and Karring (1986) 52 in a five-year longitudinal study compared SRP, modified Widman flap (MWF), and apically positioned flap (APF) in 16 patients. In this study, osseous surgery was not done. The results did not show any significant differences between the observed clinical parameters among different treatment methods. Both surgical and non-surgical treatments resulted in pocket depth reduction that was sustained for five years.
Excisional new attachment procedure (ENAP)
Yukna RA et al. (1980) 53 in a 5 years longitudinal study after performing the ENAP, evaluated clinical measurements of free gingival margin height, pocket depth, and width of keratinized gingiva were made from the cementoenamel junction in 56 surgical sites and compared to the same parameters recorded pre-surgically and at 1 and 3 years postsurgically. An overall mean net gain in the clinical attachment of 1.5 mm was found at most of the sites except for a few which showed a loss of attachment, at 5 years after treatment.
Laser-assisted New Attachment procedure (LANAP)
Yukna RA et al. (2007) 24 in a histological study investigated the regenerative effects of LANAP. Teeth with moderate to advanced periodontitis were treated with LANAP. 3 months after the therapy, all the treated teeth were removed en bloc for histologic processing. LANAP-treated teeth exhibited greater probing depth reductions and clinical probing attachment level gains than the control teeth.
Review of literature on resective osseous surgeries
Bony architecture:
O’Connor and Biggs (1964) 54 in a human skull study, examined 118 skulls with intact and presumably healthy periodontium around the teeth, to evaluate the alveolar bone anatomy around the teeth. They concluded that the interproximal bony architecture in the molar regions in buccal to lingual perspective is predominantly flat. As we move to the ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
Healing following osseous surgery:
Wilderman et al. (1970) 55 studied healing following osseous resective surgeries. They concluded that during healing there is more osteoclastic activity than osteoblastic activity. So, while achieving physiological bone contour during osseous resection it must be kept in mind not to remove too much of the bone, which may later on after healing may lead to a thin bony housing of the teeth.
Crestal bone loss from resorption after osseous resective surgery:
Aeschlimann et al. (1979) 56 in a surgical re-entry procedure evaluated the loss of crestal bone due to post-surgical remodeling. They found an additional mean vertical bone loss of 0.28 mm due to post-surgical remodeling. Moghaddas and Stahl (1980) 57 also in a re-entry procedure evaluated bone levels 3 and 6 months after osseous resective surgery. After 3 months the mean height of crestal bone loss was 0.38 mm in the inter-radicular area, 0.84 mm in the radicular area and 0.79 mm in the furcation area. After 6 months, the mean crestal bone loss was 0.23 mm in the inter-radicular area, 0.55 mm in the radicular area and 0.88 mm in the furcation area.
Soft tissue response to osseous resective surgery:
Recession due to the removal of underlying bone has been reported in many studies 58-60. Becker et al. (1988) 51 reported a mean recession of 1.32 mm at 8 weeks post-surgery, 0.93 mm at six months and 0.95 mm at 1 year post surgery in 16 periodontal patients following osseous resective surgery in 1 to 3 mm probing ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ……… Contents available in the book ………
A detailed description of various aspects of osseous resective surgeries has been given in “Osseous resective surgery”.
Conclusion
It is important to know the history of periodontal surgical procedures to understand their present status. How the initial surgical procedures were designed, the rationale behind them and how the modifications were done, gives us an idea that where we were and where we have reached. Present status of surgical periodontal procedures has been discussed in detail in “Periodontal flap surgeries: current concepts”. Presently, we are focusing on periodontal regeneration. A detailed description of the biological aspect of periodontal regeneration has been given in “Biology of periodontal regeneration”.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

