Introduction
The intra-operative management of the patient primarily includes soft tissue management and hemostasis. Because periodontal surgeries are delicate surgeries and the final outcome of the surgical procedure depends upon the vascularity of tissue, gentle handling of the tissue is very important during periodontal surgeries. In the following paragraphs, we shall read about the above-stated issues.
Soft tissue management
Any surgical procedure is initiated with the placement of incisions. Once an incision is placed, it can be altered only partially. So, selection of the incision and its placement should be precise so that incision related problems can be avoided. Following points should be considered during the placement of an incision,
1. An adequate blood supply to the flap should be secured.
2. Adequate overview of the surgical site and osseous topography.
3. Adjacent vital structures should be protected.
4. Adequate adaptation of the flap after surgery.
5. Wound closure on underlying bone.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Incisions:
While designing a tissue flap, various incisions can be selected. These include horizontal incision, submarginal incision, sulcular incision and vertical releasing incision. The flap can be full thickness or partial thickness. In a full-thickness flap periosteum is included in the flap, exposing the bone while in a partial-thickness flap, periosteum is left on the bone surface. Following are the most commonly used incisions in periodontal surgical procedures,

Horizontal incision:
The objective of placing a horizontal incision is to detach the soft tissue from the root surface. The horizontal incision may be coronally directed or it may be apically directed. The coronally directed incision is called as external bevel incision and apically directed incision is called as internal bevel incision. The external bevel incision is placed in case of gingivectomy while internal bevel incision is placed in case of periodontal flap surgeries. This incision can be marginal or paramarginal or sulcular. In the case of paramarginal incision, the distance of the incision from the gingival margin depends on the pocket depth, thickness of the gingiva, width of attached gingival and postoperative flap positioning.
Sulcular incision:
This incision is placed into the gingival sulcus and the scalpel is pushed as far as possible into the interdental space around the tooth. This incision detaches the soft tissue from the root surface, causing least possible loss of soft tissue. The pocket lining and granulation tissue on the inner surface of the flap is removed by using a sharp surgical scissor or scalpel. This incision is indicated in cases with narrow width of keratinized gingiva (≤ 3 mm), areas with esthetic concern and during regenerative procedures such as guided tissue regeneration. As minimal soft tissue loss is there, the flap margins can be adapted at its pre-surgical level. Minimum recession is expected with this incision.
Marginal incision:
This incision is difficult to make and is usually placed only in cases where the gingival margin is very thick. The scalpel is placed on the top of gingival margin and is directed towards the alveolar crest moving it forward and keeping the scalpel on gingival margin. This incision is rarely used due to problems associated with its placement.
Para-marginal incision:
This incision is placed at a distance from the gingival margin. The scalpel is placed at an acute angle to the tooth surface directed towards the alveolar bone crest. The incision is placed at a distance from the gingival margin, which is half the pocket depth measured in that area. However, the thickness of the incision also depends on the thickness of soft tissue, the width of keratinized gingiva and esthetic zone. This incision is placed in combination with sulcular incision so that the collar of the gingival soft tissue containing the pocket lining can be removed.
While placing this incision on the buccal aspect, a minimum width of attached gingiva (≥3 mm) should remain after incision placement. The incision should be more scalloped than the gingival margin itself so that interdental papillae in flap adapt appropriately in the interdental areas.
In crown lengthening cases, the incision is placed according to the desired clinical length of the crown for restoration or for esthetic requirements. It must be remembered that while doing crown lengthening for the restorative purpose, the biological width should be maintained by doing the necessary osseous reduction. This incision should be placed cautiously in areas with esthetic concern (maxillary and mandibular anterior areas) because recession may result, leading to a un-esthetic smile.
Vertical incisions:
These incisions help in increasing the mobility of the flap, thus providing better access to the surgical area. These incisions are must if the flap has to be positioned in some other location than its pre-surgical position, such as coronal or lateral or apical. The incisions are placed in such a way that they render base of the flap wider than the coronal marginal flap.
Dimensions of flap reflection:
It is important to establish the dimensions of flap reflection after carefully investigating the soft tissue. As already stated, when the horizontal releasing incision is placed; it should be extended more mesially and distally to the actual area to be operated. The level of the incision determines the final closure of the flap. In the case of insufficient keratinized gingiva, the incision should be placed as coronal as possible so that the width of keratinized gingiva does not reduce further.
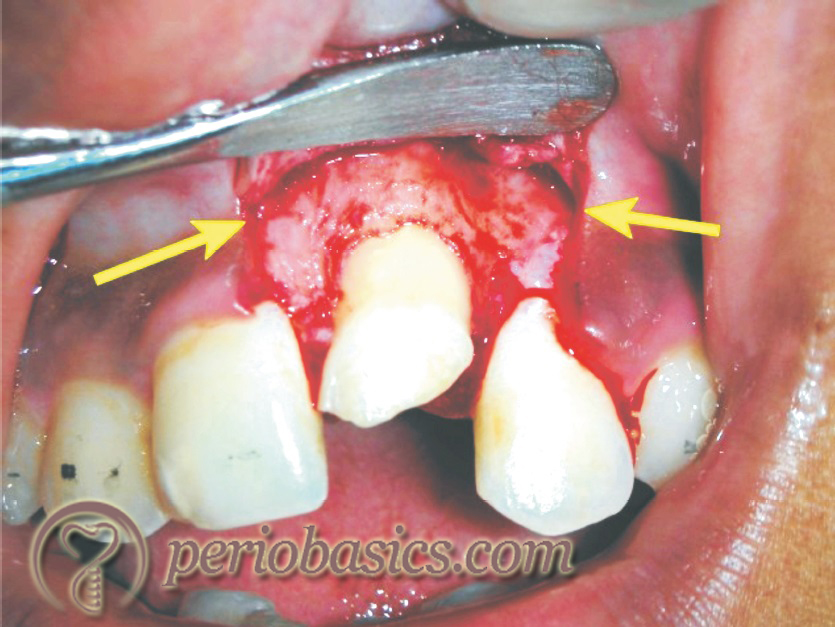
Flap reflection:
Once the objective of the surgery is established, clinician decides whether to reflect a full-thickness or a partial-thickness flap. In most of the cases, full-thickness flap is reflected. For raising full-thickness flap, the periosteal elevator is used. The reflection of the flap begins at the papilla. The sharp end of the Woodson elevator or no. 9 periosteal elevator is used to initiate flap reflection. The sharp end of the periosteal elevator is slipped underneath the papilla in the area of the incision and turned laterally to push the papilla away from the underlying bone. All the interdental papillae and the gingival margins are detached from the underlying bone. If the flap is difficult to elevate at a particular point, the incision may be incomplete and requires re-incision in that area. Once the entire free gingival edge of the flap has been reflected with the sharp end of the periosteal elevator, the broad end is used to reflect the mucoperiosteal flap to the desired extent.
In case where vertical releasing incisions have been placed, the sharp end of Woodson elevator is first used to release the marginal gingiva and interdental papillae similarly as discussed in the previous section, then broad end of the periosteal elevator is inserted at the anterior corner of the flap, and the dissection is carried out with pushing strokes in the apical and posterior direction to reach the incision line and complete flap is reflected.
It must be remembered that tissue should be handled gently. Undue stretching or pulling of the tissue may cause excessive tissue injury and may result in increased post-operative discomfort to the patient and delayed wound healing. The primary requirement of a precise flap reflection is using sharp instruments. Dull instruments cause excessive trauma to the tissue.
Hemostasis during surgery
Bleeding during periodontal surgery depends on various factors such as systemic factors, local factors, and surgical technique. Hemorrhage varies significantly between patients and within the same patient at various times 18-20. Studies have been done to measure blood loss during various periodontal surgical procedures. Ariaudo (1970) 21 observed that full-mouth periodontal flap procedures performed under general anesthesia resulted in blood loss of 350 ml. Another study demonstrated that during periodontal flap procedures involving an average of 5 1/2 teeth in posterior sextants, an average blood loss was 134 ml with a range of 16 to 592 ml 22. On an average, the volume of blood lost during a single quadrant flap surgery, which involves thinning of the flap, tuberosity reduction and some amount of bone re-contouring ranges from 300-350 ml.
During periodontal surgery, if a bleeding episode is encountered, the most effective way of stopping the bleeding is identifying the bleeder and tying off the offending vessel. Because blood vessels can be rarely isolated in periodontal tissue, tying off the blood vessel is done by a suture noose. The clinician must have the basic knowledge of blood vessels supplying that area. The most effective way to identify the bleeding vessel is to apply pressure with the back of instrument on a trial basis over the soft tissue from where the bleeding vessel is suspected to reach the bleeding site. Once the bleeding stops after applying pressure the soft tissue in that area is tied up tightly with a blind suture. If bleeding does not stop, another trial suture may be placed. After the bleeding has stopped, the patient should be placed in a recumbent position for 15-30 minutes. If the bleeding does not recur during this period, the patient can be dismissed after giving usual post-operative instructions.
Bleeding from minor blood vessels can be controlled by using local hemostatic measures, the most common of them being the application of local pressure. Following local hemostatic techniques and agents are used to control local bleeding,
1. Positive pressure.
2. Vasoconstrictor.
3. Surgicel (Johnson and Johnson).
4. Bone Wax (Ethicon).
5. Tranexamic acid.
6. Hemostatic collagen.
7. Gelfoam (Pharmacia).
8. Topical thrombin.
9. Tisseel (Baxter).
10. HemCon (HemCon Medical Technologies).
11. Electrocautery.
12. Avitene (Davol).
13. Bleed-X.

Bone reshaping:
While doing bone reshaping during periodontal flap surgery, extra care should be exercised not to remove excess of bone. The objective of bone reshaping is to achieve a physiological bony architecture which is conducive to the maintenance of periodontal health and does not facilitate re-formation of the periodontal pocket. Most of the clinicians use slow or intermediate speed handpieces for bone reshaping. A straight handpiece at slow speed provides better control to the operator during bone removal. It must be remembered that overzealous bone removal over the root prominences may result in fenestration or dehiscence. Air driven turbines are not recommended for bone reshaping because these operate at a high speed and may gauge into the bone. Secondly, the escaping aerosols from the handpiece may cause emphysema.
Least damaging of all techniques of bone reshaping is hand instrumentation using file and chisel. These are available in various sizes and shapes which facilitate their use on different types of bony architecture. Because they remove a small amount of bone, they are used in areas where little bone modification is required. These are commonly used in combination with slow or intermediate speed handpieces. The bulk of the bone is removed with a round bur and fine reshaping is done with the file or chisel.
Conclusion
Soft-tissue management and hemostasis are the cornerstones of periodontal surgical procedures. Periodontal tissues should be handled very gently to preserve an adequate blood supply of the operated area. The incisions should be designed and placed in such a way that the vascular supply of the flap is not compromised. Various local hemostatic agents should be kept ready so that they can be used whenever needed.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

