Introduction to history taking
Case history recording is the first and the most important step in the treatment of a patient. A correct diagnosis leads us to a correct treatment plan. The case history is a planned professional conversation with the patient that enables the patient to communicate their symptoms. The interest, warmth, and compassion exhibited by the clinician during history taking helps in establishing a rapport with the patient and to gain the confidence of the patient. A good clinician starts examining the patient when he/she walks into the clinic. Ideally, the case history should be recorded in a consultation room or a private room, so that the patient is free of the anxiety of dental operatory room. The clinical examination is done in dental operatory in a calm and friendly atmosphere. A proper clinical and radiographical examination can reveal many other findings which help us to find out associated problems in a particular case thus helping us to provide a good periodontal health and a functional occlusion to the patient. Following figure describes the sequence of various steps involved in the recording of case history.

Biographic and demographic information
This is the first step in history taking where we record patient’s name, address, and telephone number; identification number (e.g. social security number); age (date of birth); gender; race or ethnicity; name, address and telephone number of the referring dentist or physician, as well as that of the dentist(s) and physician(s) whom the patient consults for routine problems; and insurance and billing data which is usually handled by clerical personnel and is readily computerized. The accuracy of the data provided by the patient should be confirmed.
Name:
It is very important to know the patient’s name. It helps us to develop a personal bond with the patient and also the patient feels that the doctor is not treating him like just another case. It also helps in eliciting the case history as well as psychologically the patient is assured that the doctor is giving him personal attention. In pediatric patients, addressing the child by his/her name/ pet name facilitates the child to talk freely.
Age:
It is important to know the age of the patient because many conditions are more common in certain age groups. For example, gingivitis and bleeding gums are often seen during puberty. Grade C (aggressive) periodontitis cases are usually young patients, whereas Grade B/C (chronic) periodontitis cases are usually old patients. Wasting diseases like ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Gender:
Certain diseases are more common in a particular gender. For example, localized Grade C periodontitis with circum-pubertal onset has been shown to be more common in females as compared to males 1. However, presently it is a controversial issue because studies suggesting both, higher distribution of disease in females than males 2, 3 and no sex predisposition 4, 5 are there. Genetic polymorphisms are commonly associated with severe periodontal diseases. These may also be unequally expressed in males and females. Osteoporosis is the disease associated with a decreased bone density. It is usually found in postmenopausal women due to the decrease of estrogen levels in the body. It is well established that estrogen maintains the bone mineral density and its decreased levels are associated with a decrease in bone mineral density. Moreover, it has been observed that women are more proactive than men in maintaining their teeth and periodontal health.
Religion:
It is importnat to know the religion of the patient because unknowingly we should not hurt the religious sentiments of the patient. For example, Muslim women cover their hair and neck with a headscarf called a ‘hijab’, which they wear in the presence of the opposite sex. It may pose a problem for dentists as it may interfere with a required extra-oral examination. In some cases, we can see women covering their face, which causes difficulty for a dentist to examine her oral cavity. Careful consent is required in examining and providing treatment for such patients. If a female dentist is available with the working unit, she should take care of these patients. Muslim men avoid wearing gold jewelry. So, gold restorations should be done after consent of the patient.
In Hindu religion, eating of animal meat is prohibited. Some patients may object to certain dental materials, which they think may consist of animal parts. So, it becomes important to assure these patients regarding the materials used in their treatment. In many religions intake of alcohol is prohibited. Strict followers of these religions are apprehensive about the materials used during the treatment as it may contain alcohol as one of its constituents. So, the dentist should be aware of any religious and cultural rituals that impact on the management of the patient in order to treat the patient with empathy and understanding.
Social status:
The relationship between socio-economic status and oral health is well-established. It has been shown by many different studies that economically sound and socially well-placed people have less dental problems owing to awareness as well as frequent visits to the dentist. On the other hand, people with poor social status have more dental problems due to ignorance of oral hygiene and fewer visits to the dentist as well as the lack of dental insurance.
Occupation:
One of the most important risk factors associated with oral health today is stress. Many people have dental and periodontal problems because they have occupational stress. This is especially with those people who have public dealings every day and are subjected to work overload. These patients usually have gingival inflammation, which if ignored may lead to periodontitis. Another problem that is commonly associated with mental stress is attrition of teeth.
People working in chemical factories usually have tooth erosion associated with dentinal sensitivity. In certain occupations, the workers are exposed to abrasive dust in the environment that may cause severe attrition. Health care workers such as nurses may become carriers of transmissible diseases if infected by the patient. Sex workers ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Address:
Address helps in communication with the patient. It also helps to assess the availability of dental health facilities in the area where the patient resides. Patients follow up visits should be reduced if it is difficult for him to come frequently. Certain diseases have a geographical distribution. This distribution may vary in different parts of the country, in different regions in a state, in different villages or even in different parts of the same village. For example, fluoride levels in different drinking water sources may vary. It results in the fluorosis in the affected area where fluoride levels are more than optimum. The personal habits of the patient also vary according to geographical distribution. For example, in certain parts of the world, tobacco is smoked, whereas in some other parts it is mostly chewed in different forms. The resulting diseases with both of them are different. Tropical diseases can be seen in tropical countries.
Chief complaint
The chief complaint consists of a brief statement, preferably in the patient’s own words, concerning his reason for seeing the dentist. Actually, in the past the term “chief complaint” was used for a single problem as the patient commonly used to see a dentist for a single illness. The patients rarely sought relief for chronic, multiple, interacting problems as they do today. “Active problems” is a better term to explain patients’ presenting problems. For example, a patient with few remaining teeth has pain in a particular tooth and says “I want treatment for this painful tooth as well as artificial teeth to replace missing teeth.” So, in this case, both the problems are important: pain in the tooth as well as the inability to eat due to missing teeth. The active problems of the patient should be recorded in a chronological order. If these problems started simultaneously, these should be recorded in the order of severity.
Ideally, open-ended questions like “What brings you here? How can I help you? What seems to be the problem?”, are a good way to start with. It is important to hear the ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
History of present illness
A detailed description of the patient’s current problem(s) in a chronological order is called, the “history of present illness”. Every symptom and sign have a beginning and a course of development which must be recorded in a chronological order. Usually, a patient reports to a dentist when in pain and/or has swelling.
Pain
There is a set pattern of questions which must be asked in a sequential manner to identify the complete history of pain. These questions can easily be recalled using the word OLD CARTS (Onset, Location/radiation, Duration, Character, Aggravating factors, Reliving factors, Timing and Severity).
Onset: The patient is asked about the onset of the pain or problem. Simple question here is “when it started?” For example, if a patient has come with swelling, its onset should be asked. A swelling is usually preceded by pain so everything should be recorded in a chronological order.
Location: The patient should be asked to locate the pain. In endodontic problems the pain is usually sharp and patient can easily locate it, pointing out the concerned tooth. In the case of a periodontal problem, the pain is usually dull and gnawing in nature which is commonly felt deep in the bone, which the patient cannot usually localize to a particular tooth but to a region. Sometimes, the pain is radiated to the temporal region in case of maxillary teeth or towards the angle of the mandible when a mandibular tooth is involved. It should be recorded.
Duration: The question to be asked here is “ For how long the pain has been there?” The patient should be asked when he was absolutely fine. This gives us information about the duration of the pain.
Character: As already stated, pain may be sharp or dull in character. Sharp pains are usually associated with endodontic origin, whereas dull pains are usually associated with periodontal origin.
Aggravating factors: The patient should be asked about factors which increase the pain. For example, the endodontic pain is aggravated on lying down. Any thermal stimulus usually aggravates endodontic pain, whereas it may not have any effect on periodontal pain.
Relieving factors: Reliving factors of the pain should be recorded. In periodontal problem patient sometimes is relieved of the pain by forceful clenching of the teeth.
Timing and Severity: If the tooth has reversible pulpitis the pain should last usually within 30 seconds following a stimulus like thermal changes. In the case of irreversible pulpitis, the pain may stay for a longer duration. In both cases, the pain shall be sharp in nature. The periodontal pain may start on its own without any stimulus, is dull in nature and may stay for a variable duration.
Along with the above findings, movement of the pain if any should be noted. Referred, shifting or migrating pain should be recorded in the case history. Sometimes pain may also be accompanied by neurological signs and symptoms. A sensation of hyperesthesia, anesthesia or dysesthesia should be noted, if present.
Swelling
The duration of the pain should be noted so that its chronic or acute nature can be determined. Swelling associated with periodontal abscess usually has an acute onset and has pain associated with it. Sometimes ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Past dental history
The past dental history is one of the most important components of the patient history. In this step, we record the patient’s attitude towards previous dental treatment, the frequency of past dental visits, previous periodontic, restorative, endodontic or oral surgical treatment; the reasons for loss of teeth; fluoride history and radiation or other therapy for oral or facial lesions. Any untoward complications in any of previous dental treatment must be asked. If the patient has undergone orthodontic treatment, his/her experience with orthodontic appliances and dental prosthesis should be recorded. It is also required to record the names, addresses, and telephone numbers of the dentists involved in the previous dental treatments, especially to get complete information regarding any untoward complications which occurred during previous treatments.
Past medical history
Eliciting a patient’s past medical history is an essential clinical skill. Many medical problems have a significant effect on dental treatment. Often, the patient presents with complicating dental and medical factors such as restorative and periodontal needs coupled with a systemic disorder, such as diabetes. It is important to record any medical ailment, treatment or hospitalization for any reason. Any systemic condition for which patient is presently under treatment and the medication he/she is taking should be recorded. If the patient has undergone any radiation therapy it is important to find out the diagnosis, dose of radiation therapy and anatomic location of the treatment. In brief, past medical history consists of the following,
Major illnesses, beginning in childhood
The patient should be asked about any illness for which he was on medication. These are illnesses that require physician attention that necessitated staying in bed for longer than 3 days, or for which the patient was (or is being) routinely medicated. The patient should be asked specific ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Hospitalization
Hospitalization of the patient indicates serious illness. The record of hospitalization should be studied which is a very important source of the patient’s medical status. It also gives information about any kind of surgical procedure carried out as well as complications that may have appeared during the procedure.
Significant injuries
Many injuries are important from the dental point of view. Any injury with regard to the orofacial region should be recorded. For example, an injury to chin due to falling down may result in the temporomandibular joint problem. Any trauma to teeth may lead to the de-vitalization of teeth.
Medications
Many patients are on medications for systemic diseases, when they come for dental treatment. Complete detail of all the medicines which the patient is taking must be recorded. This is important because during the dental treatment, if we want to prescribe a medicine to the patient, any drug interaction should be taken care of. Also, conditions like drug-induced gingival enlargement are due to medicines taken by the patient for systemic diseases. The physician should be consulted to change the medication, if possible.
Allergies
Any history of classic allergic reactions, such as urticaria, hay fever, asthma, or eczema, as well as any untoward or adverse drug reaction to medications, local anesthetic agents, foods, or diagnostic procedures, should be recorded. The patient should be asked about the history of fainting, stomachache, weakness, flushing, itching, rash, or stuffy nose, and events such as urticaria, skin rash and acute respiratory difficulties. One important thing to be noted here is latex allergy. As we work with latex gloves it is important to ask the history related to latex materials. Atopic individuals, patients who have urogenital anomalies, and those with certain disorders such as spina bifida are predisposed to latex allergy 6.
Immunizations
Immunization is a common procedure these days. Because of the increased prevalence of transmissible diseases, patients without immunization are at a high risk of spreading the disease. For example, if the patient has never been immunized for HBV care should be taken regarding disinfection and transmission of infection from patient to operator.
Transfusions
A history of blood transfusion is important to note because the number of transfused blood units, may indicate a previous serious medical or surgical problem that can be important in the evaluation of the patient’s medical status. Secondly, a blood transfusion may also lead to any persistent transmissible infectious disease.
A brief gynecological and obstetric history for female patients
If a patient is pregnant, care should be taken not to expose the patient to any ionizing radiations. Surgical treatments should be avoided during pregnancy. If necessary, should be carried out during the second trimester of pregnancy. During pregnancy, use medications only if absolutely indicated. Certain antibiotics (streptomycin, kanamycin, and tetracycline) are best avoided entirely during pregnancy because of their teratogenicity. Antibiotics in category A or category B on the FDA list of approved drugs for use during pregnancy can be prescribed during pregnancy (see “Periodontal treatment of female patients” for detail).
Family history
Gathering a complete and accurate family medical history is very important as the genetic basis of periodontal diseases has been well established. Family members have many factors in common, including their genes, environment, and lifestyle. Many investigations, done on families using pedigree analysis, segregation analysis, and linkage analysis have demonstrated the genetic basis of periodontal diseases. Along with this, many systemic diseases like ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
- Has any family member suffered from the similar disease?
- Do you know any disease that runs in your family?
- Number of siblings with and without the disease?
Personal history
In personal history, a detailed description of patient’s personal habits should be recorded. Patient should be asked about his/her oral hygiene and dietary habits. The patient should also be asked about any kind of adverse habits (if he/she has any) like smoking, tobacco chewing, alcohol consumption, as they may also affect the treatment plan. Details should be gathered about the oral hygiene measures exercised by the patient by asking questions like,
- How many times do you brush your teeth?
- What king of toothbrush and toothpaste do you use?
- What brushing technique do you follow?
- Do you use any other oral hygiene measure like flossing, interdental aids or chemical plaque control measures etc?
- How frequently do you replace your tooth brush?
All these details are the indicative of awareness of the patient about the importance of maintaining good oral hygiene. Also, it helps to formulate the treatment plan accordingly and make any required changes in patient’s habits to aid in better post-treatment outcome. Education level of the patient is also an important factor affecting the treatment planning and long term maintenance of the patient. In
general, well educated patients are more aware of their oral health as compared to less educated patients.
Clinical examination
Clinical examination starts with the general physical examination. The general physical examination consists of checking the vital signs of the patient which are pulse, blood pressure, respiratory rate and body temperature. The general physical examination is followed by an extra-oral examination. In this examination, lymph Nodes, temporomandibular joint (TMJ), facial symmetry and lip competence are recorded.
General physical examination
Pulse:
The pulse should be checked for its rate, rhythm, volume, and character. It can be felt by compressing the artery against bone in different parts of the body, such as at the neck (carotid artery), on the inside of the elbow (brachial artery), at the wrist (radial artery), at the groin (femoral artery), behind the knee (popliteal artery), near the ankle joint (posterior tibial artery), and on foot (dorsalis pedis artery). The pulse rate per minute is indicative of heart rate. Pulse rate varies with the age of the patient. In newborn (0-3 months old) pulse rate is 100-150 beats per minute, in infants (6-12 months) it is 80-120, in children (1-10 years) it is 70-130 and in children over 10 years and adults, including seniors it is 60-100. In well-trained athletes, it is 40-60 beats per minute. Pulse rate lower than normal or more than normal should be noted, if present.
A normal pulse is regular in rhythm and force. There are a number of cardiac conditions which result in cardiac arrhythmias such as sinus arrhythmia, ectopic beats, atrial fibrillation, paroxysmal atrial tachycardia, atrial flutter, partial heart block etc. The volume of the pulse is the ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Blood pressure:
Blood pressure is the pressure exerted by circulating blood upon the walls of blood vessels. The normal range of systolic blood pressure is 90-119 mm of Hg and for diastolic blood pressure, it is 60-79. It is an important parameter which must be recorded before doing any invasive procedure such as extraction or periodontal surgery. In a hypertensive patient, excessive bleeding is expected. More details regarding hypertension has been given in “Periodontal treatment of medically compromised patients”. A low blood pressure is referred to as hypotension. It manifests clinically with various signs and symptoms, such as dizziness, fainting, or in extreme cases, shock. Both hyper- and hypotensive patients should be managed appropriately before going for any invasive periodontal procedure.
Respiratory rate:
The respiratory rate is measured by counting the breaths for one minute when the person is at rest. It can be done by simply observing the chest movement of the patient. The respiratory rate of a healthy adult at rest is 12–20 breaths per minute. It is more in children, with a six-month-old child having a respiratory rate of 25-40 breaths per minute. Tachypnea (fast breathing) is usually seen in fever, hypoxia, shock, metabolic acidosis, hysteria and cerebral disturbances. Bradypnea is observed in the case of cerebral compression. The expiratory wheezing sound is observed in bronchitis and asthma. The respiratory rate of the patient should be kept under observation throughout the treatment of the patient. During syncope or anaphylactic reaction, the change in respiratory rate and its character is an important sign of these conditions.
Body temperature:
The normal body temperature of a healthy individual is 37°C or 98.6 F°. It can be easily recorded with a thermometer. Fever or increased body temperature is a common sign of systemic infection. Sometimes endodontic or periodontal infection may get a systemic access which may cause fever. Space infections are also commonly associated with fever.
Extra-oral examination
Facial symmetry:
Although no face is perfectly bilaterally symmetrical, any change from the normal bilateral facial symmetry indicates some kind of pathology on the affected side. Facial asymmetry can be summarized and divided into three main categories,
1. Congenital, originating prenatally.
2. Developmental, arising during growth with inconspicuous etiology.
3. Acquired, resulting from injury or disease.
4. Inflammatory (most common) resulting from endodontic or periodontic origin and involving facial spaces.
| Various causes of facial asymmetry. | |||
|---|---|---|---|
| Congenital | Developmental | Acquired | Inflammatory |
| Cleft lip and palate Hemifacial microsomia Craniosynostosis Tessier craniofacial cleft Vascular disorders Torticollis | Usually, have an unknown cause | TMJ ankylosis Unilateral condylar hyperplasia Facial trauma Childhood radiotherapy Fibrous dysplasia Romberg's disease Other facial tumors | Due to space abscess |
Out of the above causes of facial asymmetry, space abscess is one of the most common causes of facial asymmetry. It can be easily confirmed by the case history of the patient. Temporomandibular joint pathologies are also important causes of facial asymmetry. TMJ ankylosis is most commonly the result of ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Lip seal:
Lip seal is a natural seal made between upper and lower lip at rest, without any effort. The lips may be described as,
- Competent: Here a lip seal is produced with minimal muscular effort when the mandible is in the rest position.
- Incompetent: In this case due to morphologically short upper or lower lip, a lip seal cannot be made in a relaxed state. Lips can only be brought together by the contraction of circumoral muscles.
- Potentially incompetent: In this case lip size is normal, but the lips fail to make a lipseal in a relaxed muscular state due to protruding upper central incisors.
Lymph node examination:
The lymph node examination is an important component of the extraoral examination. Lymph nodes should be examined for their number, location, temperature of the overlying skin, surface, margins and consistency. The lymph node involvement not only gives us the idea as to which group of lymph nodes is involved, but also helps us in making the diagnosis. Lymph node enlargement can be
- Inflammatory: Caused by infection (Examples: Acute lymphadenitis, chronic lymphadenitis, tuberculosis, syphilis etc.)
- Neoplastic: Caused due to neoplasms [primary (lymphosar-coma) or secondary (carcinoma, sarcoma, malignant mela-noma)].
- Hematological: Caused due to hematological disorders (Examples: Hodgkin’s lymphoma, non-Hodgkin’s lymphoma, chronic lymphatic leukemia etc.).
- Immunological: Caused due to immunological disorders (Examples: serum sickness, systemic lupus erythematosus, rheumatoid arthritis etc.).
Normally, lymph nodes are difficult to palpate, however, in an active infection, the lymph nodes draining that area become tender with the overlying skin warm. The generalized or localized lymph node involvement should be identified because some diseases such as Hodgkin’s lymphoma or lymphosarcoma have generalized lymph node enlargement whereas localized infections have regional lymph node enlargement. In the absence of any local infection, an enlarging group of lymph nodes indicates systemic disease.
The lymphatic drainage of head and neck region consists of the following group of lymph nodes,
- Deep cervical lymph nodes.
- Outer circle of lymph nodes.
- Inner circle of lymph nodes.
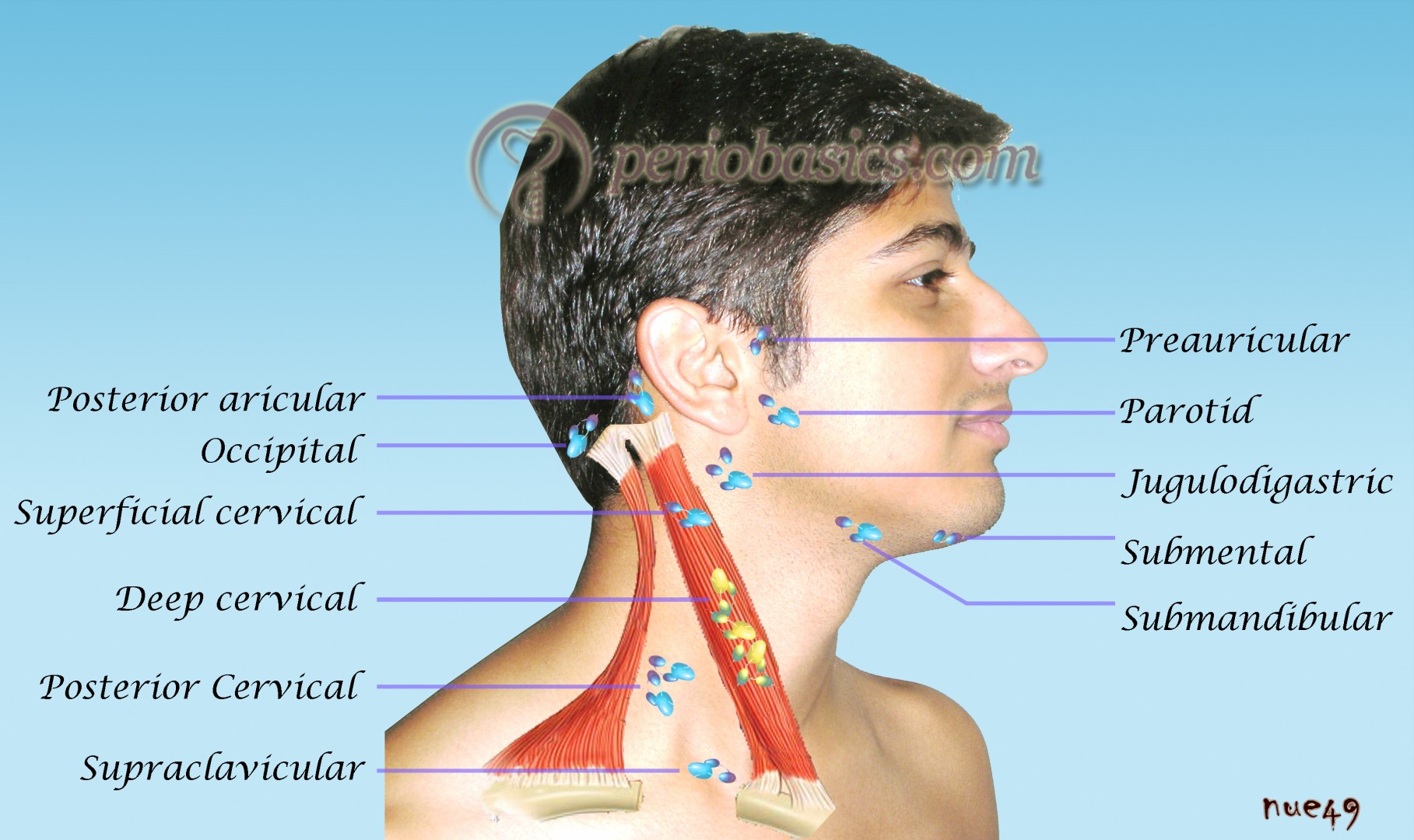
Deep cervical lymph nodes:
These lymph nodes surround the whole length of internal jugular vein and drain lymph from whole of the head and neck region. Most of the lymph reaching these nodes is already filtered by nodes of the outer and inner circle of lymph nodes. These lymph nodes are arranged into upper and lower group of lymph nodes. The upper group of lymph nodes is situated ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
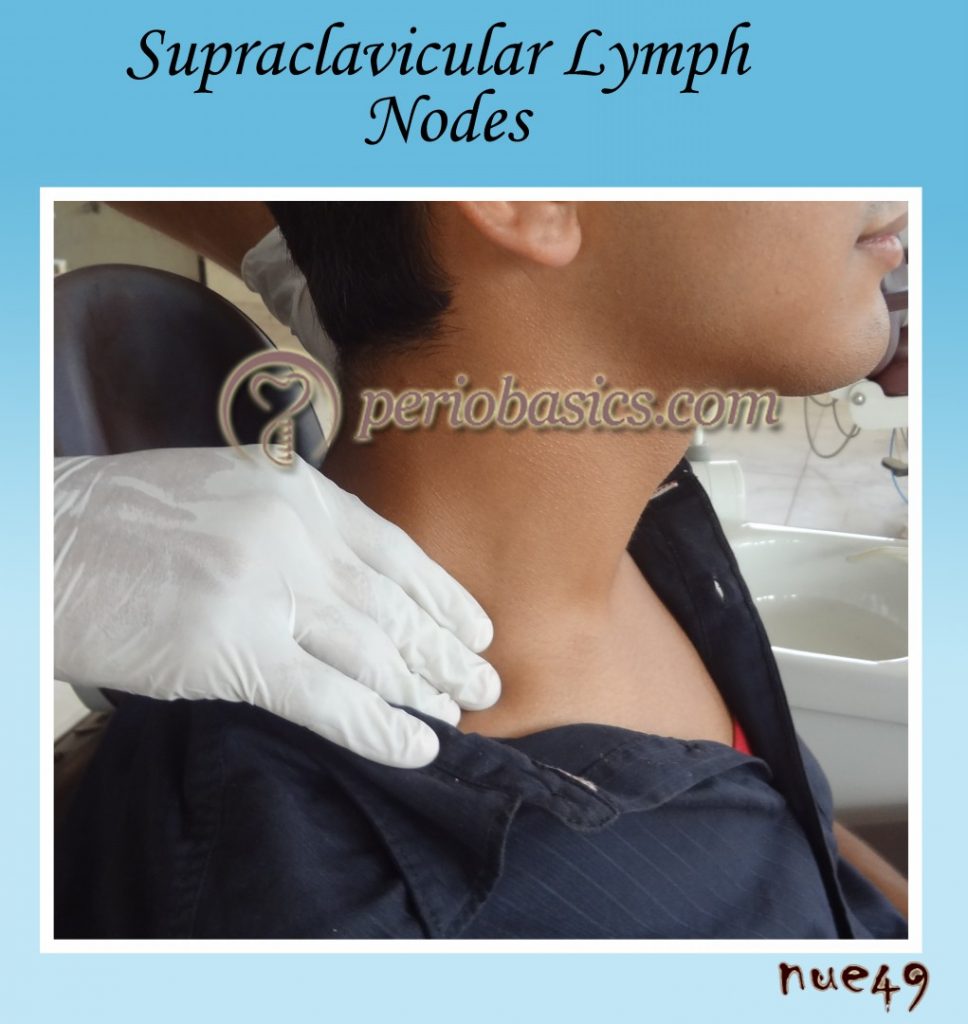
The lower group of lymph nodes is situated in the angle between the sternomastoid and the clavicle. Lymph nodes present deep to sternomastoid and above the inferior belly of omohyoid are called as jugulo-omohyoid lymph nodes. The supraclavicular lymph nodes lie posterior to sternomastoid above the clavicle.
Outer circle of lymph nodes
The outer circle of lymph nodes consists of submental lymph nodes, submandibular lymph nodes, buccal lymph nodes, mandibular lymph nodes, pre-auricular (parotid) lymph nodes, post-auricular (mastoid) lymph nodes and occipital lymph nodes.
Submental lymph nodes:
These lymph nodes lie beneath the chin. These drain the tip of the tongue, floor of the mouth, gingiva surrounding the lower incisors and a part of the lower lip. These provide bilateral drainage of lymph and drain into a submandibular group of lymph nodes, but a few also drain into jugulo-omohyoid lymph nodes.
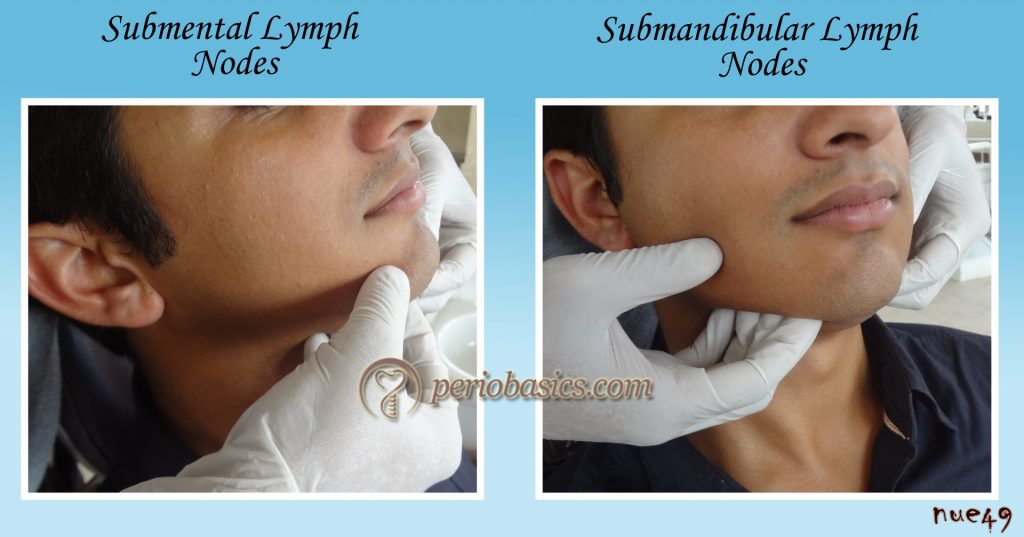
Submandibular lymph nodes:
These lie on the surface of the submandibular salivary gland. These drain from the submental lymph nodes, anterior 2/3rd of the tongue except the tip, the floor of the mouth, anterior half of the ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Buccal lymph nodes:
These lie on the surface of buccinators muscle. These are small in size and drain the surrounding area.
Mandibular lymph nodes:
These lie on the lower border of the mandible at the anterior border of the masseter. These drain a part of the cheek and lower eyelids. These drain into the upper deep cervical lymph nodes.
Pre-auricular (parotid) lymph nodes:
These lie on or within the parotid gland. Drain the vertex, temple, eyelids, orbits and external acoustic meatus. These drain into upper deep cervical lymph nodes.
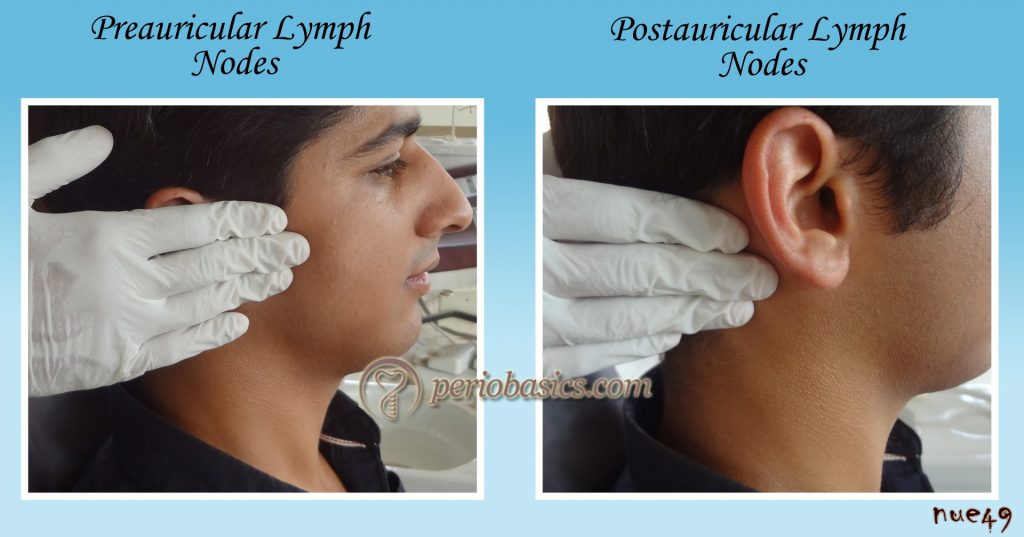
Post-auricular (mastoid) lymph nodes:
These drain the scalp, auricle and external auditory meatus.
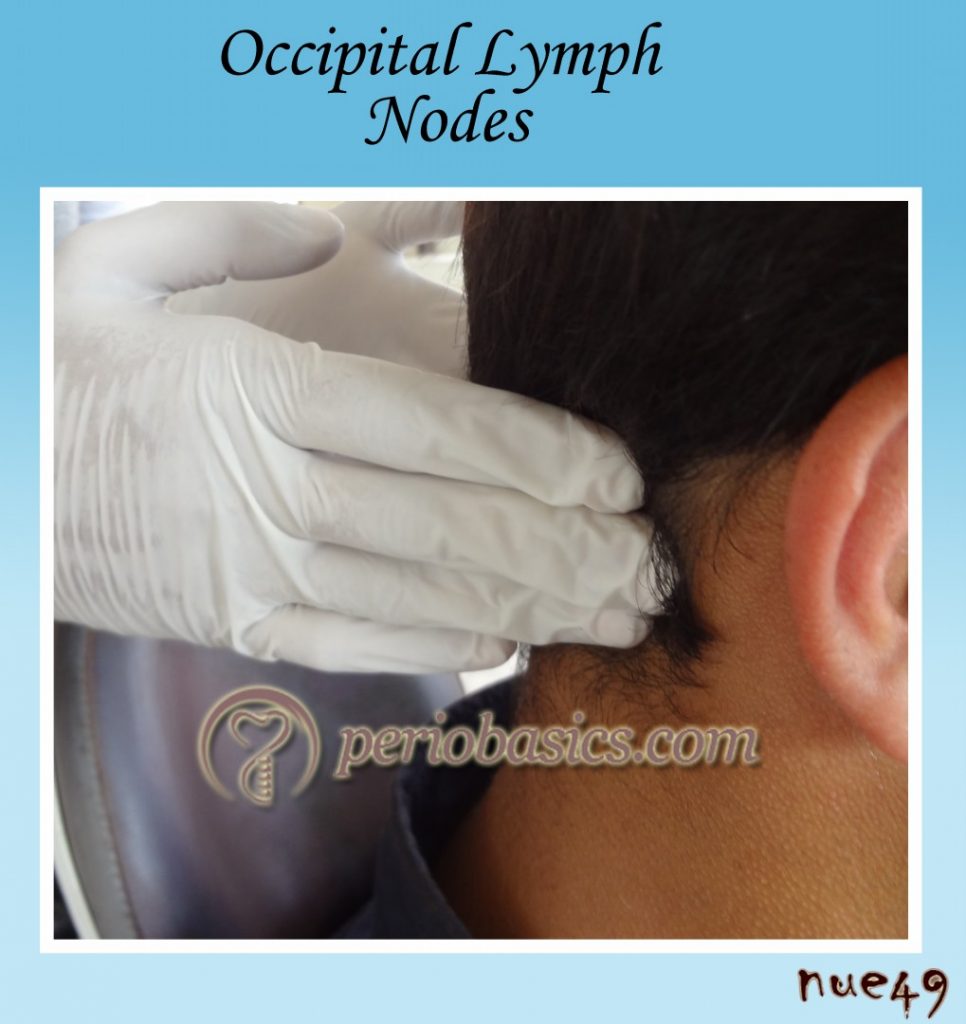
Occipital lymph nodes:
These lie at the apex of the posterior triangle and drain the posterior part of the scalp. Drainage from these lymph nodes occurs into the lower deep cervical lymph nodes.
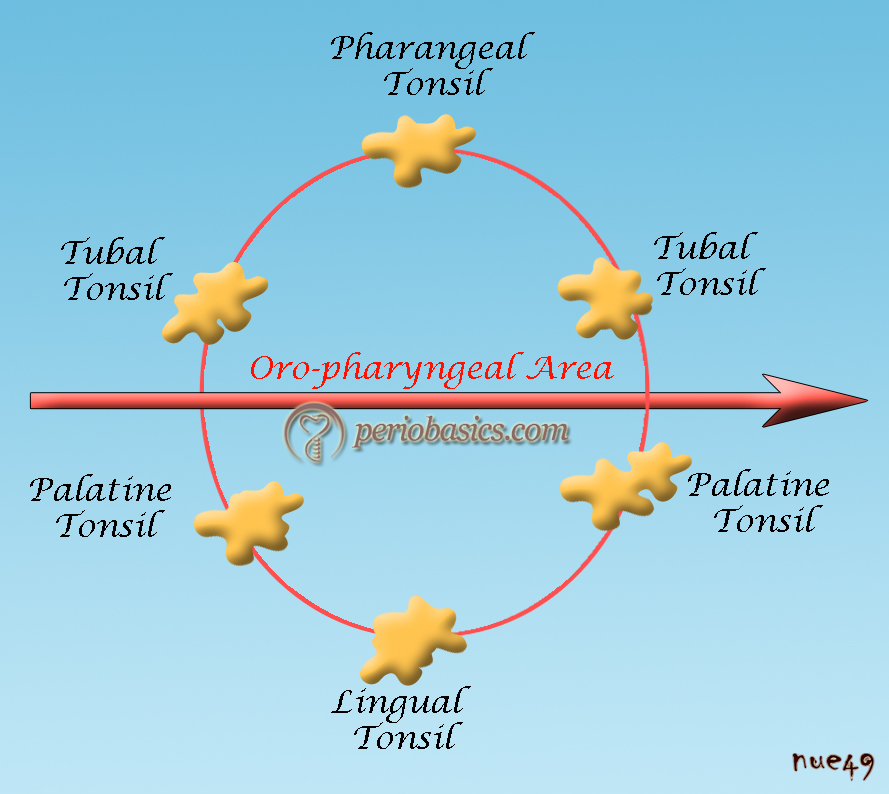
Inner circle of lymph nodes:
These lymph nodes surround the larynx, trachea, and pharynx. In this circle, we have pre-tracheal and paratracheal lymph nodes, which drain the lower larynx, trachea, and isthmus of the thyroid gland. The retropharyngeal lymph nodes drain the soft palate, posterior part of the hard palate, nose, and pharynx. All these lymph nodes drain into the deep cervical lymph nodes. There is an important discontinuous ring of lymphatic tissues around the entrance of the mouth known as the Waldeyer’s ring. This ring is made up of the tonsils, which include,
Paired:
- Palatine tonsils.
- Tubal tonsils.
Unpaired:
- Pharyngeal tonsil.
- Lingual tonsil.
Waldeyer’s ring tissue serves as a defense against infection and plays an important role in the development of the immune system, comprising the first organs in the lymphatic system that analyze and react to airborne and alimentary antigenic stimulation.
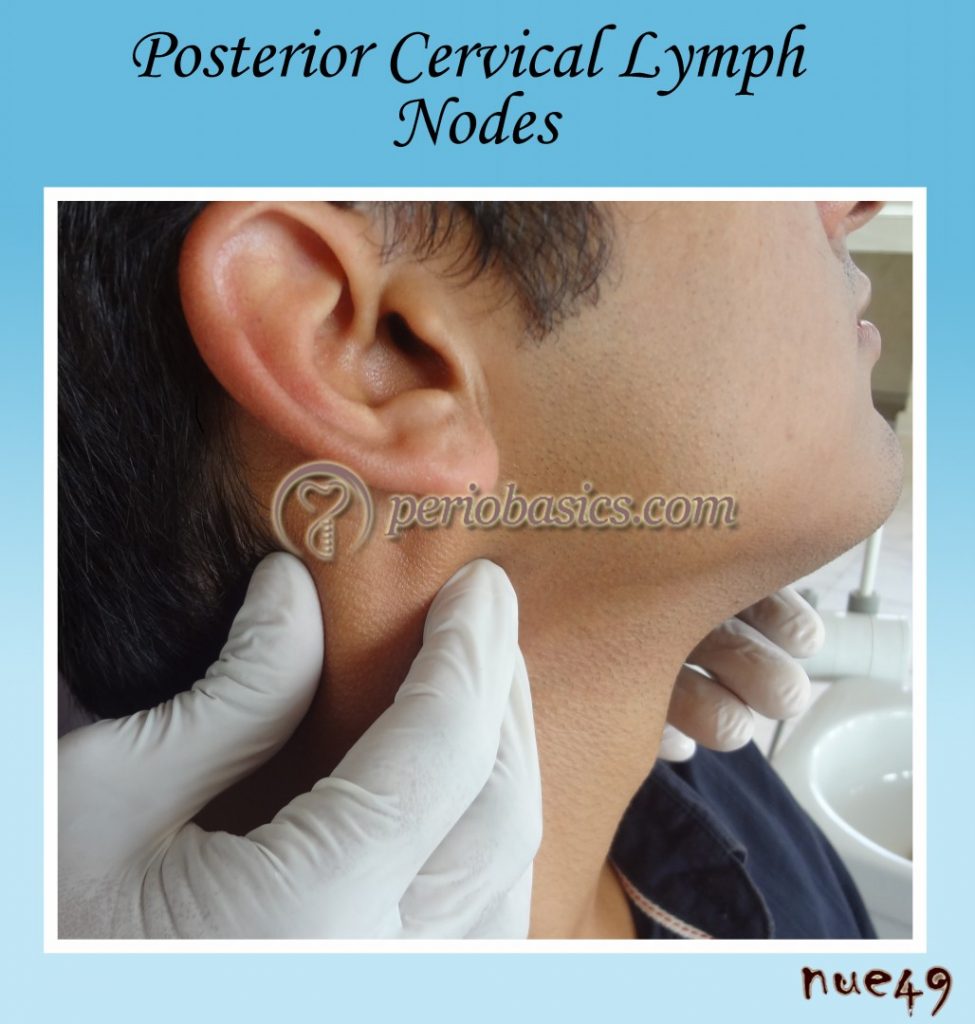
The palpation of the lymph nodes in the orofacial and neck region is usually started with the most superior nodes and continuing downwards to the supraclavicular lymph nodes. The lymph node groups around the oral cavity are palpated starting with the submental lymph nodes and going posteriorly towards pre-auricular, post-auricular and occipital lymph nodes.
Examination of temporomandibular joint
The temporomandibular joint (TMJ) is the articulation of the mandibular condyle with the glenoid fossa of the temporal bone. In TMJ there are two distinct movements, rotation and translation, occur in the joint during mandibular opening and closing. The TMJ, therefore, is called a ginglymodiarthroidal joint.
The pain in the orofacial region originating from the area of the TMJ may be due to intraarticular disease, muscular disorder, disorders of adjacent structures outside the joint, or a combination of these. The patient should be asked about the site, character, radiation and aggravating or relieving factors associated with pain. TMJ pain is often a dull, constant ache that is aggravated by opening the mandible or chewing. There may be a complaint of limited jaw opening and frequent “clicking,” “popping,” or “grinding” noise within the joint associated with mandibular movement or mastication. Other less frequent symptoms include tinnitus, changes in hearing, facial numbness, and headache. One particular symptom in patients who do night grinding is more discomfort or pain in the morning. The patient should also be asked about systemic diseases like rheumatoid arthritis, which may manifest itself in the TMJ. The detailed description of TMJ disorders has been given in “Temporomandibular joint and occlusal considerations in periodontics”.
Clinical examination
In the clinical examination of the TMJ, functions of the joint are evaluated by palpation and auscultation of the joint. In brief, noise in the joint during function is highly suggestive of the intraarticular disease. A grinding or crepitus often indicates ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Lateral and posterior palpation of the joint:
In the lateral palpation, the examiner palpates the lateral pole of the condyle with the index finger or two fingers placed near the tragus of the ear. The patient is asked to slowly open and then close the mouth. The test is positive if pain is present. In posterior palpation, the examiner palpates the posterior portion of the condyle with the little finger in the patient’s ear. The patient is asked to slowly open and then close the mouth. The test is positive if pain is present. Popping or clicking of the joint can also be felt in many cases, if it is present.

Auscultation of the joint:
In this test stethoscope is placed on the lateral aspect of the joint and any sound during joint movement is recorded. Auscultation with a stethoscope is considered positive if the clicking sound is observed at least 4 times during 5 repetitions of mouth opening.
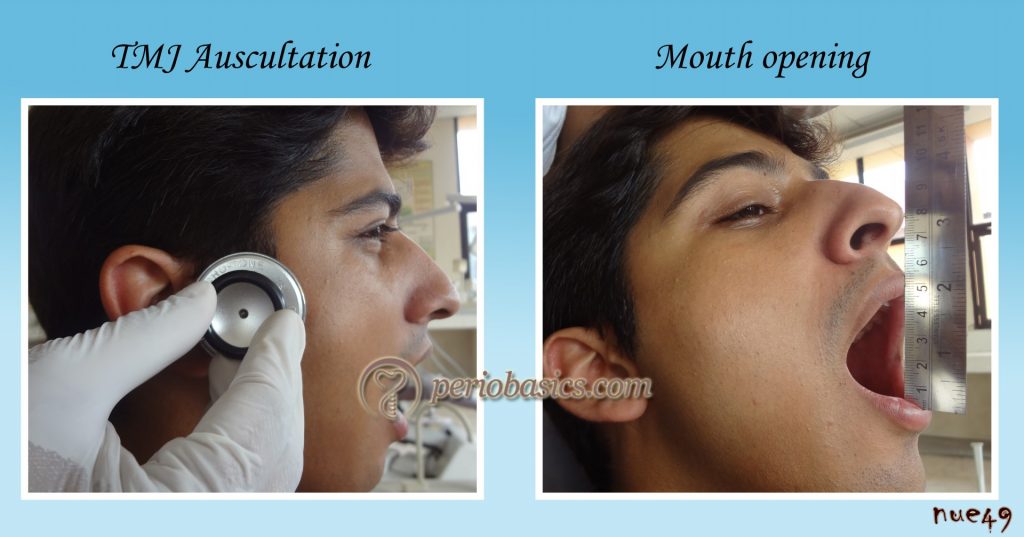
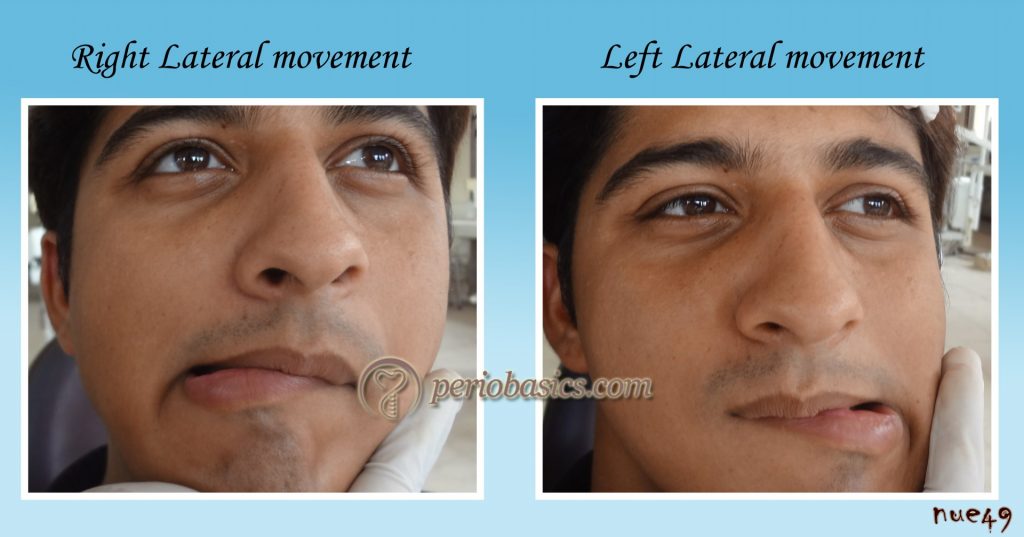
Deviation during movement:
The examiner stands in front of the patient and the patient is asked to slowly open the mouth widely without causing any pain. Normally, in an adult, the maximum mouth opening ranges from 35-50 mm. During opening if the mandible deviates to one side, it indicates disequilibrium between right and left TMJ.
Lateral and protrusive/retrusive movement of the joint:
In lateral movement, the patient is asked to slowly move the mandible to the right and then to the left side to the maximum without causing any pain. The movement should be similar on both sides. The normal lateral movement of the mandible is usually 8-10 mm. Reduced or abnormal movement on one side indicates a TMJ problem. Pain during the movement also indicates a TMJ problem. In protrusive/retrusive movements, the patient is asked to bring the mandible forward and then take it ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Intra-oral examination
The intra-oral examination is carried out by first examining the hard tissue and then examining the soft tissue, discussed as follows,
Hard tissue examination
Hard tissue examination:
In the hard tissue examination, the teeth are examined. Before we record the dental and periodontal findings, we must follow a tooth notation system.
Tooth notation systems:
Following is a brief description of three most commonly used tooth notation systems,
Palmer notation System
In 1861 Adolph Zsigmondy of Vienna introduced the symbolic system for permanent dentition. He then modified it for the primary dentition in 1874. The symbolic system is now commonly referred to as the Palmer notation system or Zsigmondy system.
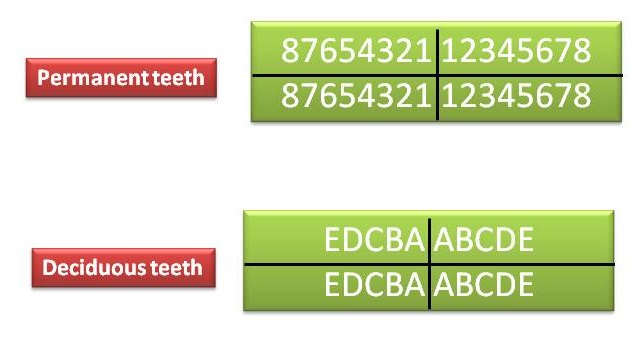
Universal notation system
ADA officially recommended the Universal system in 1968 . In this notation system for the permanent dentition, the maxillary teeth are numbered through 1 to 16 beginning with the upper right third molar. The mandibular teeth are numbered through 17 to 32 beginning with the lower left third molar. The universal system notation for primary dentition utilizes upper case alphabets.
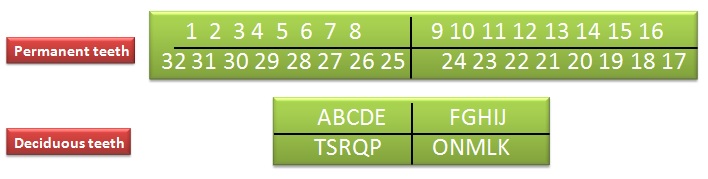
The Federation Dentaire Internationale Numbering System (FDI)
The FDI system has been adapted by WHO and IADR. In this system, each quadrant is assigned a number. The maxillary right quadrant is assigned the number 1, the maxillary left quadrant is assigned the number 2, the mandibular left quadrant is assigned the number 3, and the mandibular right quadrant is assigned the number 4. The teeth within each quadrant are assigned a number from 1 through 8 with 1 being the central incisor and 8 being the third molar.
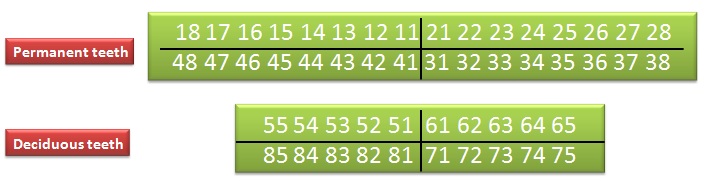
In the present case history discussion, we are following the FDI tooth notation system.
Type of dentition:
Dentition of the patient may be deciduous/permanent/mixed. Type of dentition should be mentioned here.
Number of teeth present:
The total number of teeth present in the oral cavity are mentioned here.
Notation:
In the present case history discussion, we are following the FDI notation system. Although any system can be used, but the name of the notation system should be clearly mentioned.
Carious/Decayed:
All the teeth should be examined with the help of an explorer and carious teeth should be mentioned.
Missing:
The number of missing teeth, as well as the reason for their loss, should be mentioned because it gives us information about the type of dental diseases more prevalent in the patient under examination.
Filled:
Any kind of restoration should be examined and all the teeth with restorations should be mentioned here.
Stains and Deposits:
Patients with staining of teeth should be asked about any habit like tobacco chewing etc. Some patients regularly use chlorhexidine mouthwash. In these cases, although the patient may be ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Wasting Diseases:
Wasting diseases of the teeth is a broad term mainly used to describe the attrition, abrasion, erosion and abfraction of the teeth. In wasting diseases of the teeth, the enamel is worn off. If the disease is not controlled in its initial stage, it may involve the dentine and sometimes the whole tooth gets involved. The most systematic classification of tooth wasting diseases has been given by Grippo (2004) 9 who defined four categories of tooth wear:
Attrition: The loss of tooth substance as a result of tooth to tooth contact during normal or parafunctional masticatory activity.
Abrasion: The pathological wear of tooth substance due to bio-mechanical frictional processes, e.g., tooth brushing.

Erosion: The loss of tooth substance due to dissolution by acid of either an intrinsic or extrinsic origin, e.g., gastric acid or dietary acids.

Abfraction: the pathological loss of tooth substance caused by biomechanical loading forces. It was postulated that these lesions were caused by flexure of the tooth during loading, leading to fatigue of the enamel and dentine at a location away from the point of loading. The word “abfraction” was derived from the Latin word, meaning ”to break away”. Grippo further described five categories of abfraction: hairline cracks, striations (horizontal bands of enamel breakdown), saucer-shaped (a lesion entirely within enamel), semi-lunar-shaped (a crescent-shaped lesion entirely within enamel), and cusp tip invagination (a depression on the cusp tip seen in molar and premolar teeth).
Occlusion class:
Class of Angle’s malocclusion should be mentioned here.
Food impaction:
Food impaction is the forceful wedging of food into the periodontium. There are two types of food impaction,
Vertical food impaction: It occurs due to,
A. Open contacts.
B. Irregular marginal ridge.
C. Plunger cusps: Cusps that tend to forcibly wedge the food interproximally. Causes for plunger cusp formation include occlusal wear or a shift in tooth position following failure to replace the missing tooth. It may cause inflammation of gingiva and may facilitate pocket formation.
| Classification of factors causing food impaction (Hirschfeld 1930) |
|---|
| Class I: Occlusal wear Class II: Loss of proximal contact Class III: Extrusion beyond the occlusal plane Class IV: Congenital morphological abnormality Class V: Improperly constructed restorations |
Horizontal (lateral) food impaction: It is seen mostly in areas with enlarged gingival embrasures due to gingival inflammation. Because of the inflammation, the embrasure is enlarged and lateral pressure from lips, cheeks, and tongue causes lateral food impaction.
Proximal Contacts:
Normal proximal contacts do not allow any food impaction in between the teeth. Open contact areas are usually associated with food impaction and gingival inflammation. Open contact areas can be found commonly in malaligned teeth or in the case of proximal caries where contact has been lost due to tooth decay.
Pathological tooth migration:
Pathological tooth migration is tooth displacement that results when the balance among factors that maintain physiologic tooth position is disturbed by periodontal disease 11. It may present as extrusion, facial flaring, rotation, diastema, and drifting of affected teeth, but most patients with pathological tooth migration appear to have combined forms with the most common being facial flaring and diastema. The position of a tooth depends on the health of the periodontium as well as other factors such as occlusion, oral habits and pressure from lips, cheeks and tongue.
Posterior bite collapse is ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Soft tissue examination
Examination of oral mucosa and other structures:
Any abnormality associated with tongue, lips, buccal mucosa, floor of the mouth, frenum, soft palate, hard palate and vestibule should be noted.
Examination of the gingiva
In the examination of gingiva, the gingival color, contour, consistency, surface texture, size, position (recession), gingival exudate, bleeding on probing, embrasures, McCall’s festoons and Stillman’s cleft are investigated.
Color:
During gingival examination, first of all, color of the gingiva should be noted. The color of “clinically normal” or “clinically healthy” gingiva has a shade of pale or coral pink varied by complexion and pigmentation. In the case of chronic periodontitis, the inflamed gingiva may appear reddish pink/bluish in color, whereas in case of acute inflammation it may appear bright red in color. In mouth breathers, the part of gingiva which is exposed to air is often inflamed due to drying.

Contour:
A healthy gingiva has scalloped contour with knife-edged gingival margins that adapt closely around the tooth. The papilla is pointed and pyramidal in shape, filling the interproximal area between the teeth. If there is space between the teeth, the gingiva is flat or saddle-shaped with normal color. In inflammation, the gingival margins become rounded due to edematous and fibrotic changes and papillae become bulbous, flattened and blunted.
Consistency:
A healthy gingiva is firm and resilient. It can be checked by palpating the gingiva with the side of a blunt instrument (probe). During gingival inflammation, soft, spongy gingiva dents readily when gently pressed with the side of the probe. In chronic inflammation due to fibrotic changes in the gingiva, it is firm and hard. In this case, the gingival tissue may appear pink and well stippled but when probed bleeding usually occurs in pockets. It is important to note here that the gingival margin in healthy gingiva is closely adapted to the tooth surface. When the marginal gingiva can easily be displaced from the tooth surface with a light air blast, it indicates the destruction of gingival fibers that support the gingival margin.
Surface texture:
Healthy gingiva has a stippled appearance. It is usually known as the “orange-peel appearance”. Stippling is a consequence of the microscopic elevations and depressions on the surface of the gingival tissue due to the connective tissue projections within the tissue 12-14. Clinically, it can be seen by drying the gingiva with the help of cotton and viewing it under broad daylight. It is difficult to see it under a focused light ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….

Size:
During gingival examination, size of the gingiva should be checked. Gingival enlargement is a common finding in many patients. There are many reasons for gingival enlargement which include inflammatory, fibrotic (drug-induced and idiopathic), combined, conditioned, genetic and neoplastic gingival enlargements. The detailed description of gingival enlargement has been given in “Gingival enlargement”.
Let us discuss how to record gingival enlargement. There are various indices which have been given to record gingival enlargement. Following table describes the Ingles index which is commonly used index to record drug-induced gingival enlargement.
| Ingles index for drug-induced gingival enlargement (1999) |
|---|
| Grade 0 |
| 1. No overgrowth; firm adaptation of the attached gingiva to the underlying alveolar bone. 2. There is slight stippling; there is no granular appearance or a slightly granular appearance. 3. A knife-edged papilla is present toward the occlusal surface. 4. There is no increase in density or size of the gingiva. |
| Grade 1 |
| 1. Early overgrowth, as evidenced by an increase in density of the gingiva with marked stippling and granular appearance. 2. The tip of the papilla is rounded. 3. The probing depth is less than or equal to 3 mm. |
| Grade 2 |
| 1. Moderate overgrowth, manifested by an increase in the size of the papilla and/or rolled gingival margins. 2. The contour of the gingival margin is still concave or straight. 3. Gingival enlargement has a buccolingual dimension of up to 2 mm, measured from the tip of the papilla outward. 4. The probing depth is equal to or less than 6 mm. 5. The papilla is somewhat retractable. |
| Grade 3 |
| 1. Marked overgrowth, represented by the encroachment of the gingiva onto the clinical crown. 2. The contour of gingival margin is convex rather than concave. 3. Gingival enlargement has a buccolingual dimension of approximately 3 mm or more, measured from the tip of the papilla outward. 4. The probing depth is greater than 6 mm. 5. The papilla is clearly retractable. |
| Grade 4 |
| 1. Severe overgrowth, characterized by a profound thickening of the gingiva. 2. A large percentage of the clinical crown is covered. 3. Same as for grade 3: The papilla is retractable, the probing depth is greater than 6 mm, and the buccolingual dimension is approximately 3 mm. |
Position:
Normally, the position of the gingiva is at cementoenamel junction (CEJ). Apical migration of gingiva from the CEJ is known as the recession. It must not be confused with loss of attachment. Whenever recession is present there is always a loss of attachment but the loss of attachment can also be there in the absence of recession in the form of true periodontal pockets.
Gingival exudate:
Any discharge from the gingival sulcus indicates disease activity going on in the periodontal pocket. It can be demonstrated by putting slight pressure on the lateral surface of gingiva. White purulent material oozing from the gingival margin indicates the presence of gingival exudate.
Bleeding on probing:
Bleeding on probing is an indicator of tissue inflammatory response to bacterial pathogens. It is the first sign of gingivitis. In the absence of the normal signs of inflammation, the gingiva may not be free of inflammation. So, bleeding on probing is an important sign of gingivitis. In chronic inflammation, the gingiva may appear fibrotic but inflammation is actively present in the gingival sulcus and junctional epithelium. It is important to note here that in smokers, bleeding on probing may ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Embrasures:
Gingival embrasures are defined as the embrasure cervical to the interproximal contact 16. The interdental papilla fills the space up to tooth contact in normal conditions. However, due to periodontal disease, there is a loss of interdental soft tissue and bone levels. Due to this, the position of the interdental papilla recedes from its normal position. Nordland and Tarnow (1998) 17 have given a classification of interdental papillary height as follows,
| Nordland and Tarnow (1998) classification of interdental papillary height. |
|---|
| Normal: The interdental papilla occupies the entire embrasure space apical to the interdental contact point/area. |
| Class I: The tip of the interdental papilla is located between the interdental contact point and the level of the CEJ on the proximal surface of the tooth. |
| Class II: The tip of the interdental papilla is located at or apical to the level of the CEJ on the proximal surface of the tooth but coronal to the level of the CEJ mid-buccally. |
| Class III: The tip of the interdental papilla is located at or apical to the level of CEJ mid-buccally. |
Various interdental aids used to clean different types of embrassures have been discussed in “Mechanical plaque control”.
McCall’s festoons:
These are life preserver-shaped rolled margins of gingiva where the gingiva shows fibrotic properties.

Stillman’s cleft:
Sometimes, the first sign of recession is the formation of a small groove in the gingiva. This cleft-like recession is known as Stillman’s cleft.
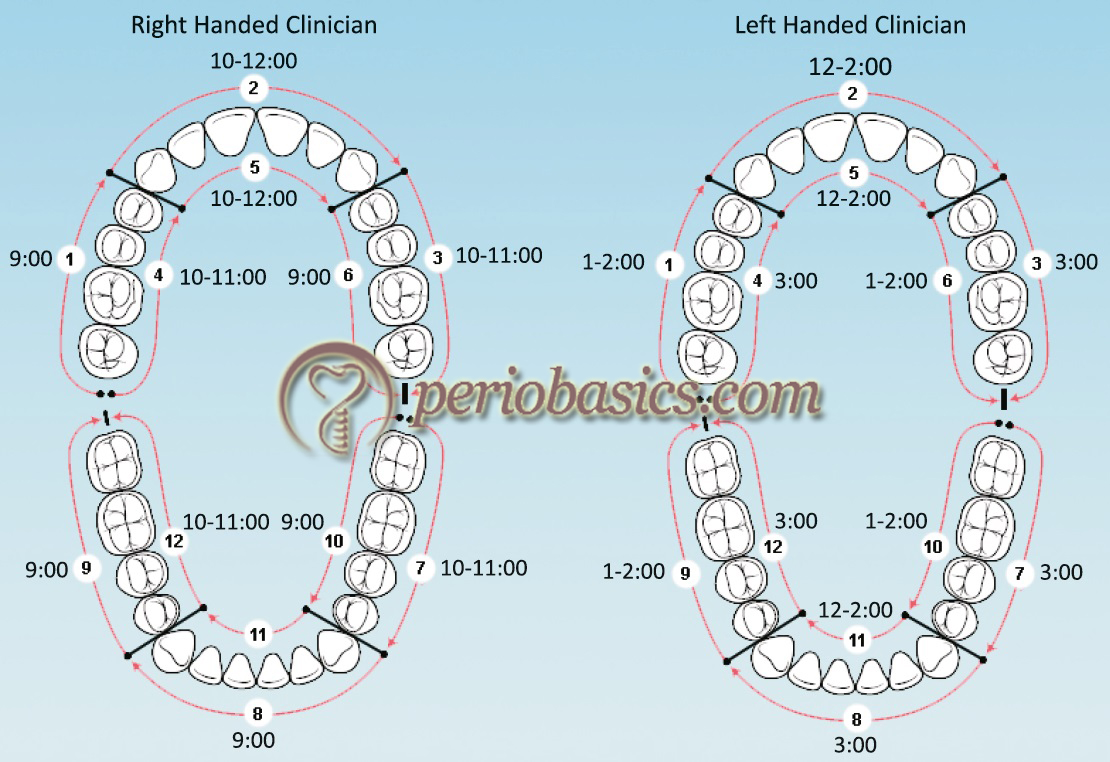
Periodontal examination
After the gingival examination is over, we record the periodontal findings. These include recording of periodontal pocket depth and loss of attachment, furcation involvement, mobility, pulpo-periodontal findings, occlusal findings and mucogingival findings. Periodontal examination is done in a systematic way, examining all surfaces of every tooth and recording the findings in a periodontal chart. Following figure demonstrates the quadrant from where we start the periodontal examination, the chairside position and how to go ahead with recording each and every surface of the tooth systematically.
Before we go into the details of periodontal findings, lets first try to understand how periodontal pockets and clinical attachment loss is recorded.
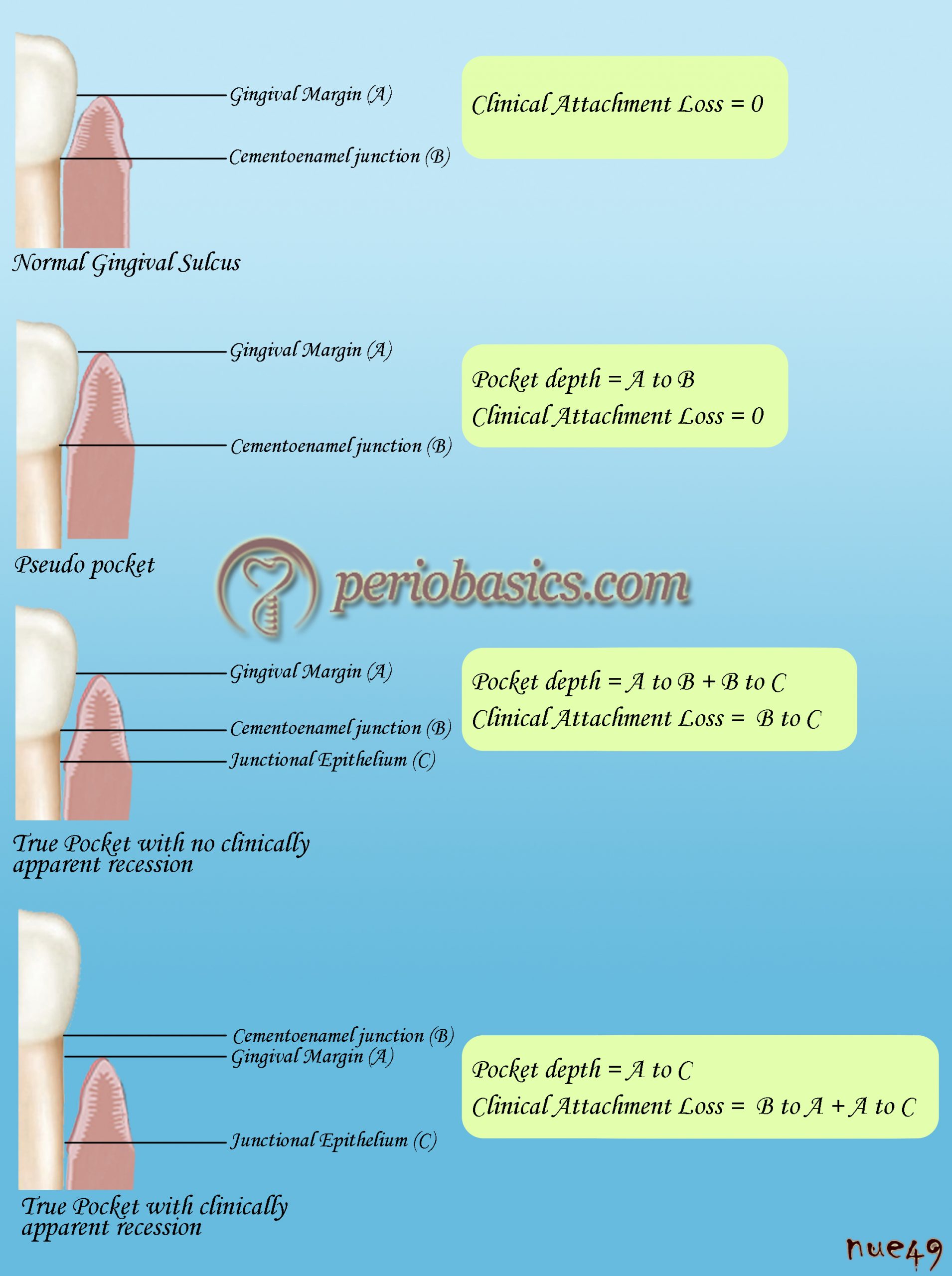
Pocket depth:
The distance between gingival margin and the base of the pocket is known as pocket depth. The pocket depth determination is the cornerstone of periodontal examination. A correct probing technique is essential to accurately determine the pocket depth. One should know the exact probing technique to avoid any false readings during the periodontal examination.
Probing technique:
Probing is the act of walking the tip of a probe along the junctional epithelium within the sulcus or pocket for the purpose of assessing the health ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Walking of periodontal probe:
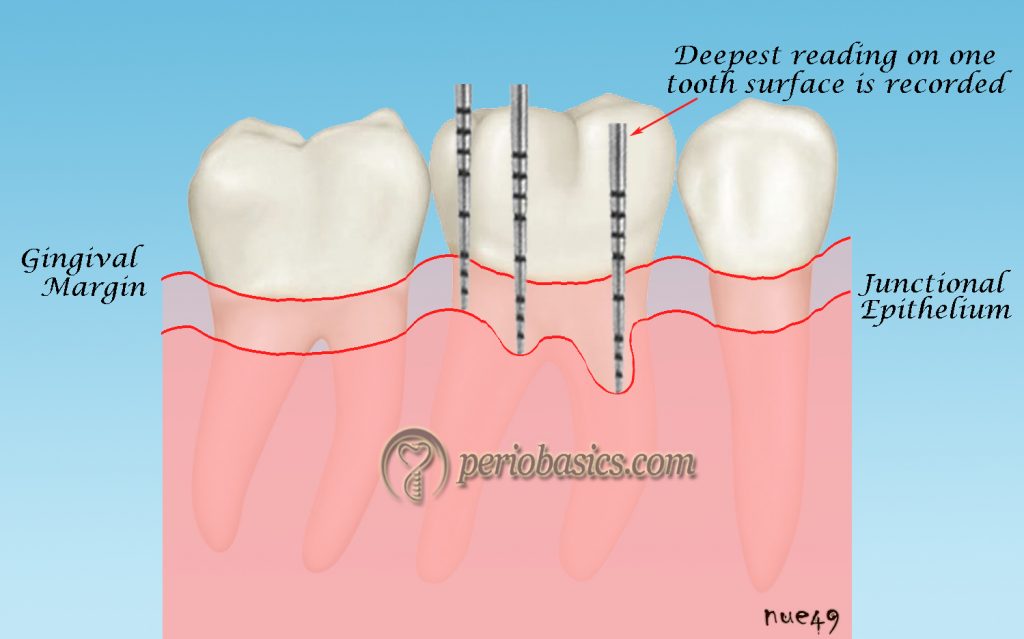
The walking stroke is the movement of a calibrated probe around the perimeter of the base of a sulcus or pocket. A calibrated probe is walked around the circumference of the tooth. The purpose is to record the periodontal pocket depth around all the tooth surfaces. It is important to note that the junctional epithelial attachment is not uniform around the tooth surface. The periodontal pocket may be present only on one surface of the tooth.

Procedure of walking the probe:
The probe is kept against the tooth surface and is inserted into the sulcus/pocket. The probe tip (1-2 mm of probe tip) is kept in contact with the tooth surface. The probe should be kept as parallel as possible to the mesiodistal and faciolingual dimension of the tooth. A series of bobbing strokes are made within the sulcus or pocket. Clinically, the force applied to the periodontal probe can be measured as the force equivalent to cause blanching of the nail bed. The probe is inserted until the tip encounters the resistance of the junctional epithelium that forms the base of the sulcus. Short, up and down, and incremental strokes of 1mm are made by moving the probe along the tooth surface. The probe should not be removed from the sulcus while probing as repeated insertion of the probe into the periodontal pocket may traumatize the gingival margin. While walking the probe only the deepest reading on one tooth surface is recorded.
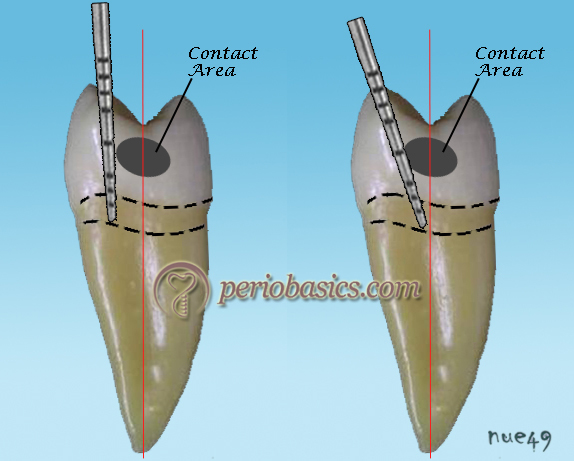
Probing the contact area:
It is done in two steps. Firstly, the probe is kept parallel to the long axis of the tooth with the tip of the probe touching the tooth surface. By walking the probe it is brought to the contact area of the teeth. The probe cannot go beyond this point into the contact area. In the second step, the probe is slightly tilted so that the tip reaches under the contact area. Now, with the probe in its right position, recommended force is applied and recording is taken when the probe touches the junctional epithelium below the contact area.
How to probe maxillary molars:
Because of the angulation of the probe, it is difficult to probe the maxillary molars especially the distal surface. Mandibular teeth also come in the way of placing a periodontal probe. So, in this case, the cheek ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
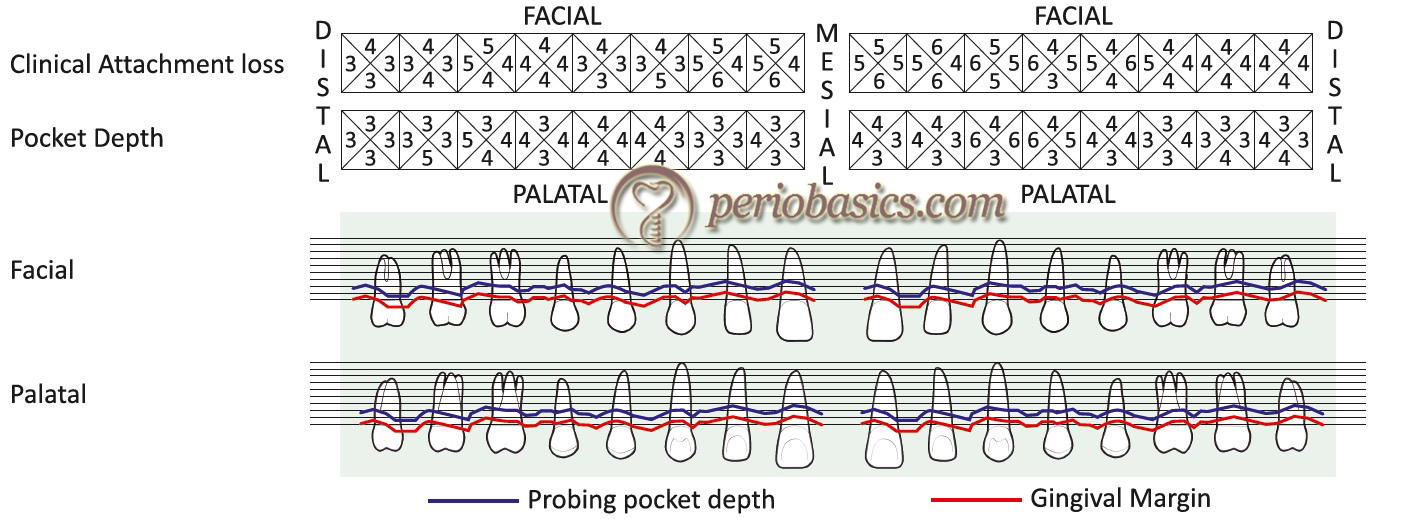
Clinical attachment loss:
For calculating the clinical loss of attachment, we first need to find out the location of the CEJ because clinical attachment loss is the apical migration of junctional epithelium from its normal position at CEJ. If the cervical area of the tooth is covered by calculus, it is difficult to find out the exact location of the CEJ. So, in such case, first the calculus should be removed by scaling. Then a periodontal probe is moved on the enamel of the tooth over the crown surface guiding it onto the root surface. We can feel the change in tactile sensation when the tip of the probe reaches the CEJ. The probe is further moved towards the apical portion of the tooth till it faces resistance from the junctional epithelial attachment. The distance between the CEJ and the base of the pocket is the clinical loss of attachment. Following figure demonstrates a sample chart for recording periodontal pocket depth and attachment loss.
Tooth mobility:
The AAP definition of tooth mobility is “The movement of a tooth in its socket resulting from an applied force”. Normally, all healthy teeth have some physiological tooth mobility which varies for different teeth and at different times of the day. It is greatest on arising in the morning and progressively decreases during the day. The increased mobility in the morning is attributed to slight extrusion of the tooth because of limited occlusal contact during sleep. During the waking hours, mobility is reduced by chewing and swallowing forces, which intrude the teeth in the sockets 18. Tooth mobility is graded clinically by applying firm pressure with either two metal instruments or one metal instrument and a gloved finger. Various mechanical or electronic devices for the precise measurement of tooth mobility have also been designed. The Muhlemann’s Periodontometer and Periotest are examples of such devices.
| Classification of tooth mobility |
|---|
| Miller Classification |
| Class 0 Normal (physiologic) movement when force is applied. Class I Mobility greater than physiologic. Class II The tooth can be moved up to 1mm or more in a lateral direction (buccolingual or mesiodistal). Inability to depress the tooth in a vertical direction (apicocoronal). Class III The tooth can be moved 1mm or more in a lateral direction (buccolingual or mesiodistal). Ability to depress the tooth in a vertical direction (apicocoronal). |
| Glickman grading of tooth mobility |
| Normal Grade 1 Slightly more than normal Grade 2 Moderately more than normal Grade 3 Severe mobility faciolingually and /mesiodistally combined with vertical displacement. |
Furcation involvement:
The extension of inflammatory periodontal disease into the inter-radicular area of multirooted teeth is known as furcation involvement 19. Diagnosis of furcation involvement is based on probing and radiographic findings. Nabers No. I and No. 2 probes have been designed especially for clinical detection of furcation involvement. To detect furcation involvement, the tip of the probe is moved towards the presumed location of the furcation and then curved into the furcation area. Mandibular molar furcation is easy to detect because they usually has two roots. Detection of furcation involvement in maxillary molars (especially the mesial and distal furcation) is difficult as compared to mandibular molars. For the mesial surfaces of maxillary molars, it is better to go for a palatal direction, as the mesial furcation is located palatal to the midpoint on the mesial surface. The distal furcation of maxillary molars is located more towards the midline, and may be detected by a buccal or palatal approach. The detection of furcation involvement is essential as it directly affects the prognosis.
| Classifications of furcation involvement |
|---|
| According to Glickman (1953) |
| Grade I: It is the incipient stage of furcation involvement, but radiographically changes are not usually found. Grade II: The furcation lesion is a cul-de-sac with a definite horizontal component. Radiographs may or may not depict the furcation involvement. Grade III: The bone is not attached to the dome of the furcation. Grade III furcations display the defect as a radiolucent area in the crotch of the tooth. Grade IV: The interdental bone is destroyed and soft tissue has receded apically so that the furcation opening is clinically visible. |
| According to Hamp et al. (1975) |
| Degree I: Horizontal loss of periodontal support not exceeding 1/3rd of the width of the tooth. Degree II: Horizontal loss of periodontal support exceeding 1 / 3rd of the width of the tooth. Degree III: Horizontal through and through destruction of periodontal tissue in the furcation area. |
| According to Tarnow and Fletcher (1984) |
| Based on vertical component. Depending on the distance from the base of the defect to the roof of the furcation: Subgroup A: Vertical destruction of bone up to 1 / 3rd of the inter-radicular height (1-3 mm). Subgroup B: Vertical destruction of bone up to 2/3rd of the inter-radicular height (4-6 mm). Subgroup C: Vertical destruction beyond the apical-third (7 mm or more). More classifications have been given in “Furcation involvement and its management”. |
Tenderness on percussion:
Any tooth which is tender on vertical or lateral percussion should be noted. Tenderness on vertical percussion indicates periapical involvement whereas tenderness on lateral percussion indicates periodontal involvement.
Periodontal abscess:
If periodontal abscess is present, it should be evaluated for the involved tooth. Periodontal abscess may be purely of periodontal origin or may be a combined abscess due to periodontal-endodontic involvement. The treatment plan is formulated accordingly.
Mucogingival findings:
The mucogingival findings include recession, depth of the vestibule and width of attached gingiva.
Recession:
The recession has already been discussed under the heading of gingival findings and subheading position of the gingiva. The apical migration of the gingival margin from its normal position at the CEJ is known as recession. In the periodontal examination chart, the Class of recession is mentioned with the respective tooth. Following are the two main classifications of recession out of which Cairo’s classification of recession is most commonly used.
| Classification of recession |
|---|
| According to Miller |
| Class I: Marginal tissue recession not extending to the mucogingival junction. No loss of interdental bone/soft tissue. Class II: Marginal tissue recession extends to or beyond the mucogingival junction. No loss of interdental bone/soft tissue. Class III: Marginal tissue recession extends to or beyond the mucogingival junction. Loss of interdental bone / soft tissue or there is malpositioning of the tooth. Class IV: Marginal tissue recession extends beyond the mucogingival junction. Loss of interdental bone and soft tissue loss interdentally and/or severe tooth malposition. |
| According to Cairo et al. |
| Recession Type 1 (RT1): Gingival recession with no loss of interproximal attachment. Interproximal cementoenamel junction is clinically not detectable at both mesial and distal aspects of the tooth. Recession Type 2 (RT2): Gingival recession associated with loss of inter-proximal attachment. The amount of interproximal attachment loss (measured from the interproximal cementoenamel junction to the depth of the interproximal pocket) is less than or equal to the buccal attachment loss (measured from the buccal cementoenamel junction to the depth of the buccal pocket). Recession Type 3 (RT3): Gingival recession associated with loss of inter-proximal attachment. The amount of interproximal attachment loss (measured from the interproximal cementoenamel junction to the depth of the pocket) is higher than the buccal attachment loss (measured from the buccal cementoenamel junction to the depth of the buccal pocket). |
Depth of the vestibule:
The depth of the vestibule may be adequate or inadequate. It is related to the width of attached gingiva. If the width of the attached gingiva is normal the vestibular depth is usually adequate. When the attached gingiva is minimal the vestibule is also shallow. Tension test is used to check the adequacy of attached gingiva.
Tension test:
This test is performed to check the adequacy of attached gingiva as well as an abnormal frenal attachment. Here the lip is moved outwards, upwards for the upper and downwards for the lower lip and also moved sideward. If the marginal and/or the interdental papilla moves away from the tooth surface, then the ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Width of attached gingiva:
Attached gingiva is non-movable gingiva, as the name indicates. It is lined by keratinized stratified squamous epithelium. The width of attached gingiva is generally greatest in the incisor region (3.5 to 4.5 mm in the maxilla and 3.3 to 3.9 mm in the mandible) and less in the posterior segments, with the least width in the first premolar area (1.9 mm in the maxilla and 1.8 mm in the mandible).
Examination of occlusion
Occlusal findings:
The occlusion of the patient should be thoroughly examined. Abnormal forces from the opposing teeth may cause various signs and symptoms ranging from slight discomfort to severe pain. Occlusal disharmony is usually a result of traumatic occlusion/ trauma from occlusion.
Fremitus test:
This test is used to detect trauma from occlusion. In this test vibratory pattern of the teeth is observed when they are brought in contact. Trauma from occlusion is an importnat clinical finding and should be carefully checked. This test has been described in “Trauma from occlusion”.
Wax records:
The wax records should be obtained if occlusal interferences are identified. Wax records are used to replicate patient’s occlusion on articulator. The interferences are first corrected on the articulator and are then replicated on the patient. For details, read “Temporomandibular joint and occlusal considerations in periodontics”.
Radiographic findings
The radiographic analysis is required to know the extent of periodontal destruction in the form of bone loss. Intraoral periapical radiographs or orthopantomogram are normally used to do the radiographical analysis. In the radiographical analysis, we record the amount of bone remaining with respect to tooth under examination, bone density, continuity of lamina dura, any radiolucent areas, pattern of bone loss and any other finding of significance. The following table describes the sample chart commonly used to record radiographic findings by dividing entire dentition into six saxtants.
| Sample chart for recording the radiographic findings | |
|---|---|
| Tooth region | Radiographic findings |
| Maxillary right first premolar to last molar (14-18) | |
| Maxillary canine to canine (13-23) | |
| Maxillary left first premolar to last molar (24-28) | |
| Mandibular left first premolar to last molar (34-38) | |
| Mandibular canine to canine (33-43) | |
| Mandibular right first premolar to last molar (44-48) | |
Provisional diagnosis
A provisional diagnosis is the one that is initially determined to be the diagnosis. It is followed by investigations which help us in making the final diagnosis. The special investigations may include microbiological, immunological or molecular investigations.
Special investigations
Microbiological analysis:
It involves the isolation and identification of bacteria from plaque samples. Some bacteria can be grown in culture, whereas others may not be grown in cultures. The colony count of bacteria grown in culture gives us an indication regarding the number of bacteria in plaque sample. This investigation is important for the diagnosis of Grade C periodontitis cases and some special cases where repeated treatment is not able to control the disease progression.
DNA analysis to identify plaque microorganisms:
The DNA analysis is done for those bacteria which cannot be grown in culture. Here the plaque sample is subjected to various DNA amplification methods. The specific DNA of a bacterial species is allowed to pair with the DNA available in the sample. If that particular organism is present in the sample its DNA makes a double strand with the test DNA single strand which is then amplified for identification.
Immunological investigations:
These investigations are based on immunological tests. For example, patients with Grade C periodontitis have poly-morphonuclear cell function abnormalities which predispose the patient for the rapid periodontal breakdown. These tests are used to confirm these abnormalities.
Blood examination:
It is done for patients scheduled for periodontal surgery as well as patients who are suspected to have any kind of bleeding disorder. The routine blood examination is mandatory before any surgical procedure. If the patient has any systemic disease the corresponding blood tests should be advised.
Urine examination:
Urine examination is indicated in patients with systemic diseases where the disease status can be identified by doing specific tests.
Biopsy:
In the case of any overgrowth, an excisional or incisional biopsy should be taken and sent for histopathological investigation.
Study casts:
Study casts are especially useful for occlusal evaluation of the patient. If the patient is having any kind of occlusal disharmony, these casts are articulated on a fully adjustable articulator and selective occlusal reduction is carried out to achieve occlusal harmony which is then replicated on the patient.
Any other specific test:
Any other specific test should be advised if required under special circumstances.
Final diagnosis
A complete and accurate diagnosis is required to make an appropriate treatment plan. If the patient has healthy periodontium, it should be identified whether the periodontium is intact or reduced. If the patient has gingivitis, it should be identified whether it is localized or generalized. If the patient has periodontitis, Stage and Grade of the periodontitis should be carefully decided. Along with this, if the patient has any associated systemic disease, it should also be considered in making the final diagnosis. The steps in making the final diagnosis have been discussed in “Classification of periodontal and peri-implant diseases and conditions”.
Prognosis
The prognosis is a prediction of the probable course, duration, and outcome of a disease, based on the general knowledge of the pathogenesis of the disease and presence of risk factors for the disease. The determination of the prognosis facilitates the formulation of treatment plan as well as the periodontal maintenance protocol. Prognosis can be divided into two types: overall prognosis and individual prognosis.
Overall prognosis:
It is the prognosis based on the sum of various local, systemic, environmental and other factors which may affect the overall periodontal health of teeth. Factors which affect the overall periodontal prognosis include age, genetics, oral hygiene, systemic conditions such as diabetes mellitus, environmental factors such as stress and smoking, patient compliance and economic consideration.
Individual prognosis:
It is the prognosis of individual teeth, based on local and prosthetic/restorative factors that have a direct effect on their prognosis. These factors like attachment loss, probing depth, furcation involvement; crown-to-root ratio, fixed abutment status, and percentage of bone loss are the most important factors in determining tooth loss. A detailed description of prognosis is available in the chapter 45 “Determination of prognosis”.
Treatment plan
The treatment plan is the reflection of diagnosis. An accurate and complete diagnosis guides us to formulate an appropriate treatment plan. For a systematic approach, treatment plan has been divided into four phases.
Phase I Therapy or Etiotropic Phase
Phase II Therapy or Surgical Phase
Phase III Therapy or Restorative Phase
Phase IV Therapy or Maintenance Phase or suppo-rtive periodontal therapy
| Phases of treatment plan |
|---|
| Emergency phase/Preliminary Phase |
| · Due to endodontic or periapical pathology. · Due to periodontal pathology. · Any other reason. · Extraction of hopeless teeth and provisional replacement, if required. |
| Phase I Therapy or Etiotropic Phase |
| · Patient education about plaque control and maintaining oral hygiene. · Demonstration of accurate brushing technique indicated for the patient. · Scaling and root planing to remove soft deposits and calculus. · Restorative and/or prosthetic corrections. · Excavation of caries and restoration (temporary or final, depending on whether a definitive prognosis for the tooth has been arrived at and on the location of caries). · Antimicrobial therapy (local drug delivery or systemic). · Diet control (in patients with rampant caries). · Treatment of occlusal abnormalities. · Minor orthodontic movement. · Provisional splinting and prosthesis. |
| Evaluation of Response to Etiotropic Phase |
| · Pocket depth and gingival inflammation. |
| Phase II Therapy or Surgical Phase |
| · Periodontal surgical procedures, including placement of implants. · Endodontic therapy completion. |
| Phase III Therapy or Restorative Phase |
| · Final restorations. · Fixed and/or removable prosthodontics. |
| Phase IV Therapy or Maintenance Phase or supportive periodontal therapy for Periodic rechecking |
| · Plaque and calculus evaluation. · Gingival and periodontal status. · Occlusion, tooth mobility. · Any other pathologic changes. |
If the patient is in pain, these phases are preceded by the emergency phase, which involves the elimination of pain or any other emergency treatment. It is important to note that after completion of Phase I therapy, the patient is placed on the Maintenance Phase (Phase IV) to preserve the results ……… Contents available in the book ……… Contents available in the book……… Contents available in the book……… Contents available in the book …….
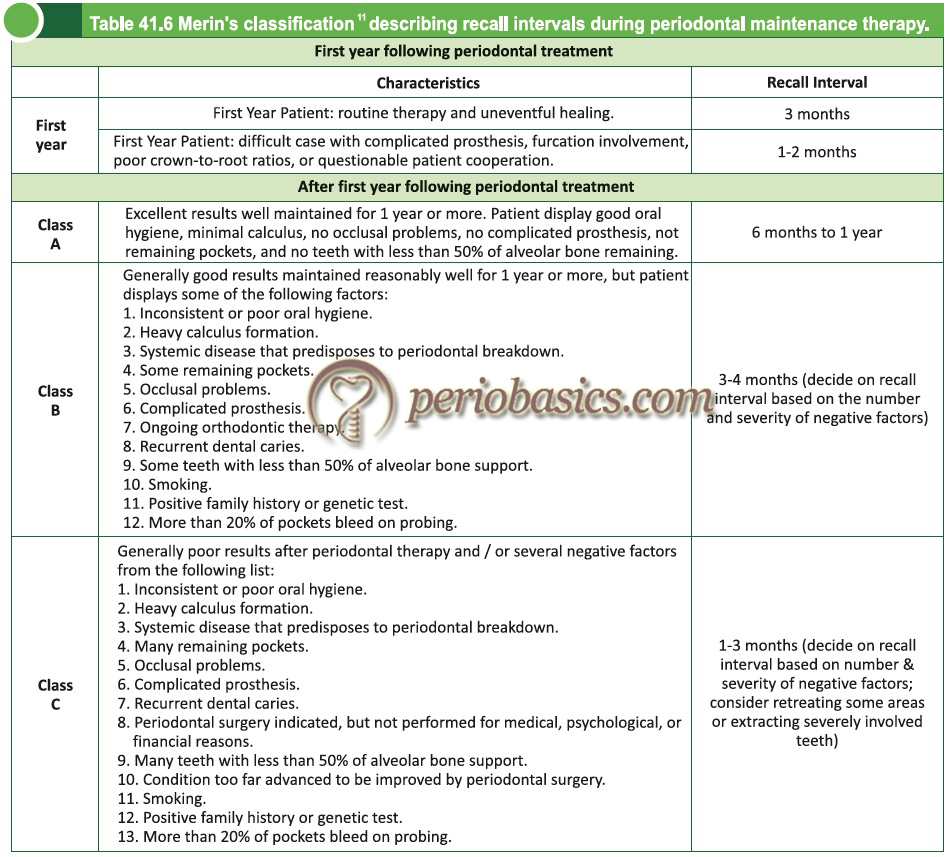
Supportive periodontal therapy
Maintenance phase or supportive periodontal therapy is defined as an extension of active periodontal therapy. It is distinct from but is an inseparable part of active periodontal treatment. During this phase of the treatment plan, the patient is periodically evaluated for the periodontal status and needful treatment is provided according to the disease condition. Details about supportive periodontal therapy are available in “Periodontal maintenance”. According to Merin’s classification, the patient recall during the first year is different from the following years.
Conclusion
Case history recording is the first and most important steps in the successful outcome of the treatment. It is the blueprint of overall treatment planning for a patient. Further, case history also provides us the information regarding the risk factors associated with the disease progression in a particular patient. An appropriate treatment planning may prevent many complication that can happen intra-operatively and post-operatively. However, it must be remembered that a good history recording requires an in depth knowledge of the subject. One should master the art of history taking for appropriate treatment of the patient.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:

