Introduction
Periodontal diseases are a group of conditions affecting the supporting structures of the dentition. These are multifactorial diseases where many risk factors affect the progression of the disease. Among those risk factors identified for periodontitis are bacterial colonization, age, gender, socioeconomic status, genetic predisposition, certain systemic conditions, and smoking. Tobacco smoking has been found to be a major environmental risk factor associated with generalized forms of severe periodontitis in several studies 1-4. Cigarette smoke contains at least 400 potentially toxic substances, including hydrogen cyanide, carbon monoxide (resulting in the formation of carboxyhemoglobin), free radicals, nicotine, nitrosamines (potent carcinogens) and a variety of oxidant gases (causing platelet activation and endothelial dysfunction).
History of tobacco use
Tobacco is a green, leafy plant that is grown in warm climates. After leafs of the plant are picked up, these are dried up and used in different forms such as smoked form (cigarette, pipe, or cigar) or smokeless (chewed tobacco) or sniffed through the nose (called snuff). Tobacco has been used in different forms by mankind for centuries. The Mayan Indians of Mexico carved drawings in stone that date back to somewhere between 600 to 900 A.D. show tobacco use. The Mayans ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
Probably, the first European to see the tobacco plant was Christopher Columbus in 1492 when he arrived in ‘San Salvador’, where he was greeted with wooden spears, wild fruits and dried leaves. However, Columbus threw the leaves away. The tobacco leaves were brought to Portugal by Friar Roman Pane, a monk who accompanied Columbus on his second voyage in 1493. After this, the use of tobacco started to spread.
Initially, tobacco was grown in different parts of Europe, which then was grown in other parts of the world with the migration of Europeans. Tobacco was the first crop grown for money in North America. The first official condemnation of tobacco use was issued by King James I in England in 1604. The first cigarette making machine was invented by James Bonsack in 1881. After this, cigarette smoking became widespread.
Constituents of tobacco smoke
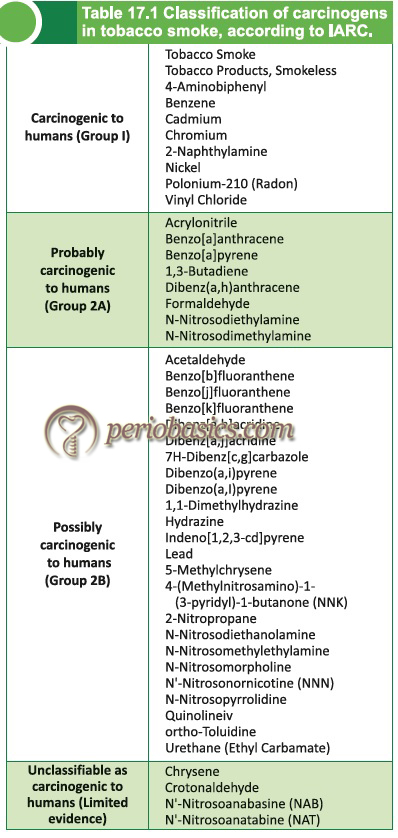
The tobacco smoke is composed of more than 400 chemical constituents, many of which are toxic, mutagenic and carcinogenic. The tobacco smoke constituents are derived from non-specific products of organic material combustion (such as acetaldehyde and formaldehyde) and chemicals that are specific to the combustion of tobacco and other components of the cigarette (e.g. tobacco-specific nitrosamines). In 1989, the United States Surgeon General released a report 5 listing 43 carcinogenic agents found in tobacco smoke. Those carcinogens and their classification according to the International Agency for Research on Cancer (IARC) are listed in the following table,
Pharmacokinetics of nicotine
Nicotine is the main alkaloid found in tobacco and is responsible for its addictive potential. Its half-life is approximately 2-3 hours and it is the most active compound in smoke. During smoking the inhaled nicotine is absorbed through the pulmonary venous rather than the systemic venous system, and thus reaches the brain in 10-20 seconds. It is highly lipid-soluble and rapidly enters the cell membrane. It is not well absorbed through the oral mucosa because of its ionized form. It has action on all parts of the body but has a predilection for the brain and other nervous tissue. Nicotine acts on the nicotinic acetylcholine receptors, specifically the ganglion type nicotinic receptor and the CNS nicotinic receptor. By binding to nicotinic acetylcholine receptors, nicotine increases the levels of several neurotransmitters, including dopamine. It is thought that increased levels of dopamine in the reward circuits of the brain are responsible for the euphoria and relaxation and eventual addiction caused by nicotine consumption.
Nicotine is basic in nature, so its absorption from the stomach is limited, but intestinal absorption is far more efficient. The duration of action of nicotine in chewable tobacco is longer than inhaled nicotine because of its slow rate of absorption. The average cigarette contains 6 to 11 mg of nicotine and delivers about ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Effect of smoking on various organ systems
Peripheral nervous system: Nicotine causes transient stimulation and subsequently a more persistent depression of all autonomic ganglia. It has a biphasic action on the adrenal medulla. In small doses, it evokes the discharge of catecholamines whereas, in large dose, it prevents their release in response to splanchnic nerve stimulation.
Central nervous system:
The primary sites of action of nicotine in the CNS are prejunctional nerve ending, causing the release of other neurotransmitters (mainly dopamine which stimulates reward circuit). Nicotine is a CNS stimulant. In small doses, it produces weak analgesia, whereas high dose may produce convulsions. It is also a respiratory stimulant. Nicotine induces vomiting by both central and peripheral actions.
Cardiovascular system:
Nicotine causes stimulation of sympathetic ganglia and the adrenal medulla, together with the discharge of catecholamines from sympathetic nerve endings, resulting in vasoconstriction, tachycardia, and elevated blood pressure.
Gastrointestinal tract:
Nicotine stimulates parasympathetic ganglia and cholinergic nerve endings, resulting in increased tone and motor activity of the bowel.
Exocrine glands:
Nicotine causes an initial stimulation of salivary and bronchial secretions that is followed by inhibition.
Who is a current smoker, a nonsmoker, and a former smoker?
According to Centre for Disease Control (CDC) and Prevention, the smokers are classified as:
Current smokers: Those that had smoked ≥ 100 cigarettes in their lifetime and smoked at the time of interview.
Non-smokers: Those that had not smoked ≥ 100 cigarettes in their lifetime.
Former smokers: Those that had smoked ≥100 cigarettes in their lifetime, but were not currently smoking.
According to the number of cigarettes smoked/day, smokers can be classified as:
Heavy smokers: smoke ≥ 20 cigarettes/day.
Light smokers: smoke ≤ 19 cigarettes/day.
Pharmacology of tobacco smoke products
Tobacco smoke has two distinct phases: Vapor and particulate phase.
Vapor phase: Contains CO2 and up to 5% of CO.
Particulate phase: It is in the form of aerosols and has liquid droplets and solid sub-microscopic particles (diameter 0.8 – 1.6μm). It contains tar droplets of the free substance suspended on these tar particles.
Measurement of exposure:
Patient’s exposure to tobacco can be measured by simple questions, sophisticated questionnaire, and biochemical analysis. The biochemical analysis includes estimation of exhaled CO in breath and cotinine (a metabolite of nicotine) in saliva, plasma / serum or urine. Cotinine measurements are more reliable in determining a subject’s exposure to tobacco smoke because its half-life is 14 – 20 hours as compared to nicotine (2-3 hours). The mean plasma and salivary cotinine concentration of regular smokers is approximately 300 ng/ml and for non-smokers it is 2 ng/ml.
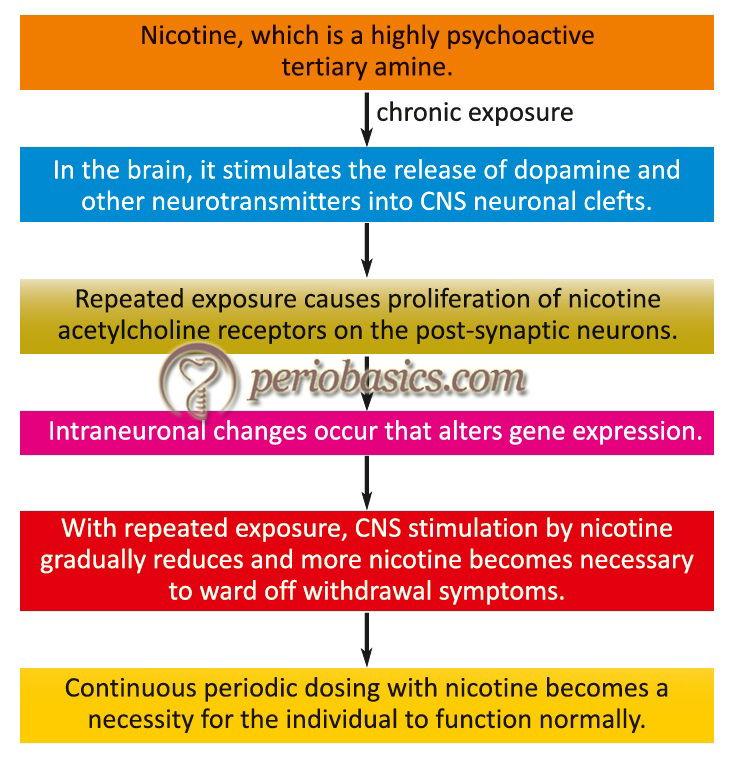
Mechanism of nicotine addiction
Nicotine acts on the brain and other parts of the nervous system. It’s use is associated with many well-known pleasurable psychoactive effects, such as arousal, relaxation, and improved mood. Nicotine has been shown to act as a positive reinforcer of smoking because a regular smoker tries to maintain a particular level of nicotine in the body. The mechanism of nicotine addiction has been demonstrated in the following figure,
Evidence for relationship of smoking with periodontitis
Arno et al. 6 in 1958 studied a sample of 1346 employees, 25 to 55 years old, to find out if there was any association between tobacco consumption and the presence of gingivitis after adjustment for hygiene and age. The authors found that there was a significant relation between tobacco consumption and the presence of gingivitis. In a subsequent study on 728 male patients (21-45 years of age), the radiographic examination showed that alveolar bone loss increased with increasing use of tobacco, thus suggesting that tobacco consumption is a complicating factor in periodontal disease 7. In a study done by Solomon et al. (1968) 8, 9561 patients ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
A study done on healthy male Spanish military recruits to find out the degree of periodontal disease and its relationship to smoking revealed higher plaque and bleeding indices in non-smokers although probing depths and attachment loss were greater in smokers 4. Another clinical study done in Northern Ireland demonstrated periodontal probing depth in excess of 4 mm was more than double in young smokers (15%) as compared to non-smokers (6%) 10. Several studies have shown smoking as a major environmental factor associated with generalized forms of aggressive periodontitis 11, 12. Overall, many studies in which smokers and non-smokers had similar plaque accumulation or where it was adjusted, have demonstrated that smokers had deeper probing depths 13-16, greater attachment loss 10, 14, 15, 17, 18, greater alveolar bone loss 14, 19-21 and greater tooth loss 14, 18.
The strongest evidence in support of this relationship comes from the National Health and Nutrition examination survey (NHANES)- III, where 12,329 U.S. adults (18 yrs or older) were evaluated for periodontal status in smokers and non-smokers. The results of the study demonstrated that approximately 75% of periodontitis cases were ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
Effects of smoking on periodontal diseases
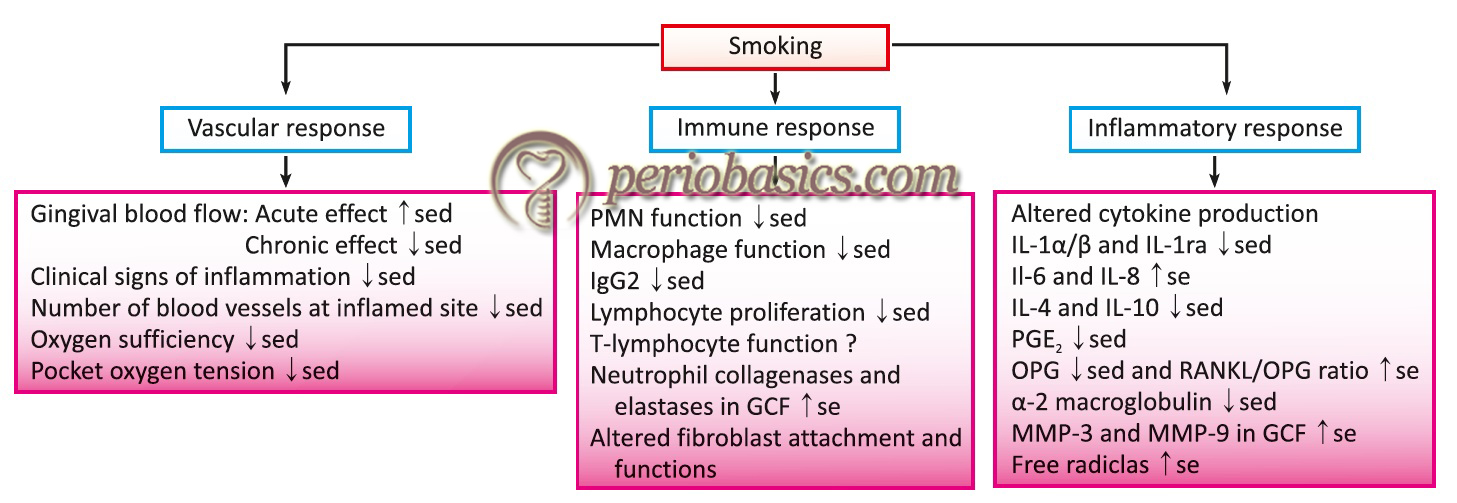
Effect on clinical signs of inflammation:
One of the most important biological effects of smoking on periodontal tissues is reduced clinical signs of inflammation. Nicotine in the smoke may cause vasoconstriction in the peripheral blood vessels, thus may reduce the clinical signs of gingivitis 23. Many studies have shown decreased clinical signs of inflammation in the presence of the same amount of local factors in smoking patients as compared to non-smoking patients 24-26. This has been reported that the reduction in clinical signs of gingivitis in smokers is independent of plaque levels 23.
Effect on gingival epithelium:
Heavy smokers often present with a thickened, fibrotic appearance of their gingival tissues. It has been shown that heavy smokers have grayish discoloration and hyperkeratosis of the gingiva. Changes in the epithelium were described as keratotic, hyperkeratotic and hyperplastic 27. Prolonged irritation from tobacco smoke causes changes in the oral mucosa, causing benign smoker’s keratosis, leukoplakia etc.
Effect on gingival bleeding:
As already explained the initial signs of inflammation of gingiva are suppressed in smokers. Bleeding on probing is the initial sign of inflammation of gingiva. The nicotine present in cigarette smoke stimulates sympathetic ganglia, which release neurotransmitters, including catecholamines 28. Catecholamines are potent vasoconstrictors causing a reduction in the blood flow in gingiva. This results in decreased gingival bleeding on probing. The decreased gingival bleeding in smokers can also be attributed to ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
Effects on gingival crevicular fluid (GCF):
Various studies have been done to compare the volume of GCF produced in smokers and in non-smokers. Contradictory results have been reported. Some studies have shown a decreased secretion of GCF in smokers as compared to nonsmokers 32-34. The reason for this decrease in GCF flow has been suggested to be the peripheral vasoconstriction which causes decreased blood flow and hence decreased GCF production. On the other hand, some studies have reported increased GCF flow in smokers. McLaughlin et al. (1993) 35 demonstrated an increased GCF flow in smokers and compared to non-smokers. In another study Mavropulos et al. (2003) 36 also observed increased GCF flow in smokers. They measured the gingival blood flow with a laser doppler. The authors explained this increased GCF flow on the basis of increased gingival blood flow during smoking. They mentioned that normally smoking causes a vasoconstriction. However, the degree of vasoconstriction is overcome by the evoked rise in arterial perfusion pressure. As a consequence, the gingival blood flow increased during smoking. The authors speculated that small repeated vasoconstrictive attacks due to cigarette smoking may, in the long run, contribute to gingival vascular dysfunction and periodontal disease. Hence, the effect of smoking on GCF flow needs further research to reach an appropriate conclusion.
Effects on host immune response:
Various aspects of host immune response are affected by smoking. These include the adverse effects on fibroblast function 37, defective chemotaxis and phagocytosis by neutrophils 38, 39 and disturbance in immunoglobulin production 40, 41. Studies have shown elevated levels of TNF-α in the GCF of smokers 42 as well as elevated levels of PGE 2, neutrophil elastase, and ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
It has been observed in many studies that in smokers the migration of neutrophils in the periodontal tissue from blood vessels is similar to non-smokers, however, once in the tissues, the continual exposure to smoke may impair their further progress into the periodontal pocket. The oxidative respiratory burst is an important mechanism by which neutrophils kill microorganisms. It has been suggested that in smokers the respiratory burst is compromised, causing a diminished neutrophil response to microorganisms 45. Dendritic cells play an important role in the initiation of the inflammatory response. It has been shown that acute exposure of dendritic cells to cigarette smoke extract suppresses their activation by bacterial lipopolysaccharide (LPS). It results in the reduced production of interleukin-12 and interleukin-23 cytokines, resulting in the modulation of inflammatory response 46, 47.
Effects on humoral immune system:
The humoral immune system is also affected by smoking. Macrophages are the components of both cellular and humoral immunity. It has been demonstrated that alveolar macrophages derived from smokers exhibit reduced expression of Class II MHC 48, 49. Further investigations have shown a decreased concentration of serum IgG in smokers 50-54. Along with this, serum IgG titers against Prevotella intermedia and Fusobacterium nucleatum have been shown to be reduced in smokers 55.
In a study, effect of smoking on IgG subclasses in young adults with aggressive forms of periodontitis was investigated. Results showed that smoker group with an aggressive form of periodontal diseases had depressed IgG immunoglobulin subclasses as compared to nonsmoker group. Also, smoking was not found to depress serum levels of IgG2 in black subjects, except for those with generalized periodontal destruction 56.
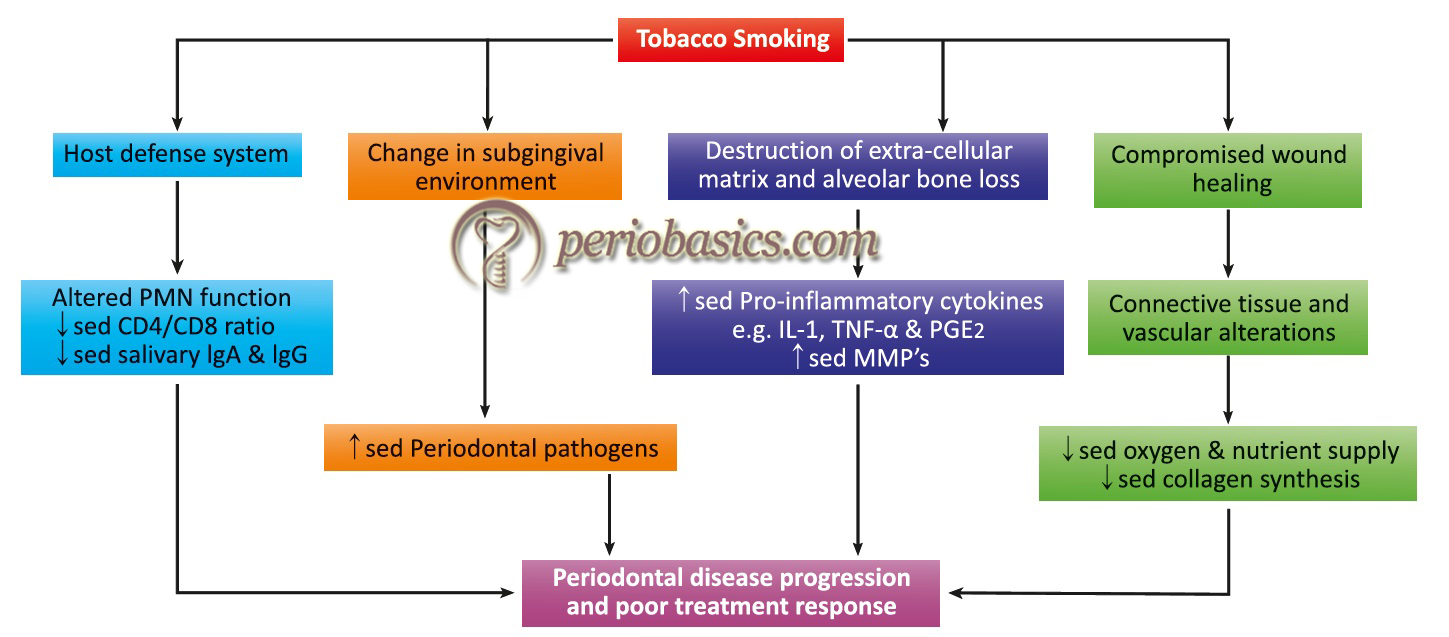
Effects on cytokine production:
Many studies have suggested that smoking influences host cytokine levels. It has been shown that exposure to bacterial lipopolysaccharides in smokers results in significantly more production of TNF-α and Interleukin-6 (IL-6) and also the acute phase protein α2-macroglobulin 57 (Figure 17.2). However, in another study, smokers showed a significantly lower concentration of α2-macroglobulin in GCF as well as total amounts of α2- macroglobulin and α1-antitrypsin than in non-smokers 58. Bostrorm and Bergstrom (1998) 59 ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
These variations in the cytokines also affect the chemical mediators involved in bone remodeling. The sRANKL/OPG ratio has been found higher in smokers compared with non-smokers and OPG concentration has been found significantly lower in smokers 63.
Effects of smoking on subgingival microflora:
Smoking does not appear to increase the amount of plaque formation when other factors are controlled 45. Smoking causes a change in the subgingival environmental conditions by lowering of the oxidation-reduction potential (Eh), and this could cause an increase in anaerobic plaque bacteria 33. One investigation showed a statistically significant increase in the proportion of Gram-negative to Gram-positive bacteria in 3-days old plaque from smokers when compared with the non-smokers 64. Studies have demonstrated an increase in subgingival pathogenic bacteria in smokers. These include Tenerella forsythensis, Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and Treponema denticola 64-66. The changes in the oral ecosystem which, among other effects also predispose smokers to the increased risk of oral candidiasis.
Effect on calculus formation:
In general, more calculus has been observed in smokers as compared to non-smokers. This might be due to the increased salivary flow rates in smokers. There is an increased calcium concentration in fresh saliva in smokers following smoking, which may facilitate more calculus formation 67. Calculus formation in pipe smokers has been found to be more than cigarette smokers 68. This might be because, the pH of pipe smoke is higher than that of cigarette smoke. Furthermore, pipe smokers ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
Effects on periodontal treatment and post-operative healing:
Smoking has adverse effects on periodontal treatment outcome and post-operative healing. One investigation showed that past smokers and non-smokers responded similarly to the treatment and heavy smokers (over 20/day) had higher plaque levels during maintenance and poorest response to the treatment, but did not significantly differ from light smokers 70. Another microbiological study showed that current smokers had less healing and reduction in subgingival B. forsythus and P. gingivalis after treatment as compared to former and non-smokers 71.
Smokers have been shown to have deeper pockets after periodontal therapy than non-smokers, and these pockets continue to harbor quantitatively and qualitatively more pathogenic bacteria than shallower pockets 33. Another factor responsible for reduced healing is reduced fibroblast, PMN, and epithelial cell function as well as reduced host defense response. Fibroblasts have been shown to bind and internalize nicotine, which is detrimental to their function because of which there is a slow production of collagen fibers by these cells and thus periodontal healing is delayed 72.
Effects on regenerative therapy:
Research has shown that recession sites treated using connective tissue with a partial thickness pedicle graft 73 and a coronally positioned flap alone, or with a bioabsorbable membrane 74 found no difference in root coverage between smokers and non-smokers. On the other hand, when guided tissue regeneration procedures were used ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Effects on implant therapy:
Studies have shown the detrimental effects of smoking on the success of implant therapy. One of the initial studies done on smoking and its effects on implant therapy found the overall implant failure rate of 5.92% and specifically implant failure in smokers was 11.28% as compared to 4.76% in non-smokers 80. In fact, the success rate of dental implant has been found to be twice in non-smokers as compared to smokers and that too maxillary implants are more affected 81. The smokers showed a higher score in bleeding index with greater peri-implant pocket depth and radiographically discernible bone resorption around the implant, particularly in the maxilla 82. Also, studies have shown the benefit of smoking cessation on ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book………
Acute necrotizing ulcerative gingivitis and smoking:
Acute necrotizing ulcerative gingivitis occurs more frequently in smokers. Possible mechanisms for this increased susceptibility include vasoconstriction of gingival blood vessels, reduced activity of leukocytes and proliferation of anaerobic, fusospirochetal micro-organisms. Along with this, other factors like poor oral hygiene and mental stress are jointly implicated in the etiology of acute necrotizing periodontal diseases in smokers.
Smoking cessation
Studies have shown beneficial effects of smoking cessation on periodontal health. Dentists play an important role in smoking cessation, reason being patients visit their dentist more often than their physician, so dentists have more opportunity for patient counseling. Also, oral effects of smoking e.g. staining of teeth are visible to the patient, which can help the dentist to explain the effects of smoking on oral and systemic health.
Transtheoretical model of smoking cessation:
This is the most widely used model for smoking cessation (Prochaska and DiClemente 1983) 84. There are five stages in this model which help the health care providers to understand at what stage the patient is in and what type of support is indicated for smoking cessation by the patient.
Precontemplation stage:
In this stage, the patient is not aware that the habit is the cause of his/her problem and has no intention of quitting. Here the aim of health provider is to increase the awareness of the problem and to guide them into the contemplation stage.
Contemplation stage:
Now, the patient is aware of the fact that smoking is the reason for his/her problems and expresses an intention to stop it within 6 months. The aim of health workers is to reinforce and encourage the patient to follow through with their intentions.
Preparation stage:
The patient intends to stop the habit within less than 1 month. Most of the patients at this stage have previously attempted to quit, but without success. Patients are most responsive. Adjunctive therapies should be offered to help the patient in smoking cessation.
Action stage:
In this stage, the patient stops the habit and maintains early abstinence. Significant effort should be made to control withdrawal symptoms at this stage, otherwise, there are chances of relapse.
Maintenance stage:
The patient has stopped the habit for six continuous months. Continued efforts should be made to prevent relapse.
Cessation advice for health care providers:
The guidelines for health care providers when giving smoking cessation advice include the ‘Five A’s’ which are,
- Ask at each appointment about current and past smoking status.
- Advise all smokers to quit.
- Assess the smoker’s current stage in the transtheoretical model.
- Assist the patient in the preparation stage, including nicotine replacement therapy (NRT).
- Arrange for proper follow-up, and refer the patient to a smoking cessation clinic, if necessary.
Nicotine withdrawal
There are two types of nicotine withdrawal agents: nicotine containing and non-nicotine containing. These agents are used to replace nicotine and gradually lower patients dependency on smoking.
Nicotine containing nicotine replacement agents:
These contain nicotine and deliver measured amounts of nicotine so that gradually the nicotine intake can be reduced. These are available in the following forms,
- Patch: Habitrol, Nicoderm.
- Gum: Nicorette
- Nasal spray: Nicotrol NS
- Inhaler: Inhaler Nicotrol
Nicotine patch:
Patch is often a preferred route for clinical use because of little compliance problem. Patch is applied on different skin areas to minimize irritation. Three bands of the patch are available in different strengths, according to the patch size and are used for 16-24 hours each. Largest patch is used for initial 4 weeks and next smaller size for ………….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……….. Contents available in the book……..
Nicotine Gum:
4 mg nicotine gum is usually preferred when:
- Skin disease or adhesive allergy result in contraindication to patch.
- When the patient has not been successful with using the patch.
- As a supplement to patch.
- When gum is preferred by the patient for any reason.
One piece should be used every 1-2 hours for 6 weeks, then 2-4 hours for the next 3 weeks, 4-8 hours for next 3 weeks. The “chew and park” routine is followed for about 30 minutes per piece. The patient must be instructed to chew the gum until the peppery taste is noticeable and then to park the gum as nicotine absorption occurs.
Nicotine nasal spray:
It is an option that simulates the rapid delivery effect of cigarette smoking. The recommended dose is 1 spray into each nostril 8-16 times daily.
Nicotine oral inhaler:
It resembles smoking. The dosage is 16 cartridges per day.
Use of any of the products is recommended for 8-10 week period, continued use of nicotine replacement agents beyond 10-12 weeks is not recommended.
General contraindications:
These are similar for all nicotine supplements.
- Patient in an immediate post-myocardial infarction period.
- Patient having severe arrhythmias.
- Patient having severe or worsening angina pectoris.
Specific contraindications:
Skin patches: skin disorder
Nasal spray and inhalation system: asthma/ chronic nasal disorder.
Nicotine gum: TMJ disorder/ denture
Non-nicotine agents:
Bupropion hydrochloride:
It is a nicotine replacement alternative. It is used as a centrally acting non-nicotine agent. Patient strongly dependent on nicotine may use bupropion in combination with nicotine, as a nicotine replacement agent. Patient’s medical history, current medical status, and behavior must be carefully evaluated before recommending bupropion. It interacts with many drugs, including alcohol antipsychotic agents, hepatic enzyme inducers and inhibitors, levodopa and MAO inhibitors. These are of concern because many of these agents potentiate the risk of seizures. Use of bupropion differs from nicotine replace-ment in that bupropion treatment should begin 7-10 days before the patient selected quit date, whereas pharmaceutical nicotine substitution should begin on the quit date.
Conclusion
From the above discussion, it is clear that tobacco smoking has got adverse effects on various aspects of periodontal health. The toxic substances present in tobacco smoke are one of the risk factors for periodontal disease progression. Studies have also shown the adverse effects of smoking on healing after periodontal therapy. Also, cessation of smoking has favorable effects on healing and maintenance of periodontal health. Dentists can play an important role in smoking cessation and also help the patients to maintain good periodontal health during the maintenance phase of periodontal therapy.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

