Introduction to host-modulation therapeutics
As already discussed in the previous chapters, the primary etiology of periodontal diseases is bacterial infection 1. In addition to bacterial etiology, the progression of periodontal diseases is adversely influenced by a number of risk factors and risk indicators like diabetes, gender, age, hereditary factors and smoking 2. Traditional treatments focused on reducing the bacterial load through scaling and root planning, but they were not effective in every patient. Löe et al. (1986) 3 in their study on Sri Lankan tea workers demonstrated that not all individuals have the same response to similar amounts of plaque accumulation.
Definition
Host modulation therapy (HMT) is a treatment concept that aims to reduce tissue destruction and stabilize or even regenerate the periodontium by modifying or down-regulating destructive aspects of the host response and up-regulating protective or regenerative responses.
The purpose of HMT is to restore the balance, on one hand, between pro-inflammatory and anti-inflammatory mediators and on the other hand between destructive enzymes and their inhibitors. They can be systemically administered or locally delivered and used as adjuncts to scaling and root planning 4.
Pathogenesis of periodontal diseases
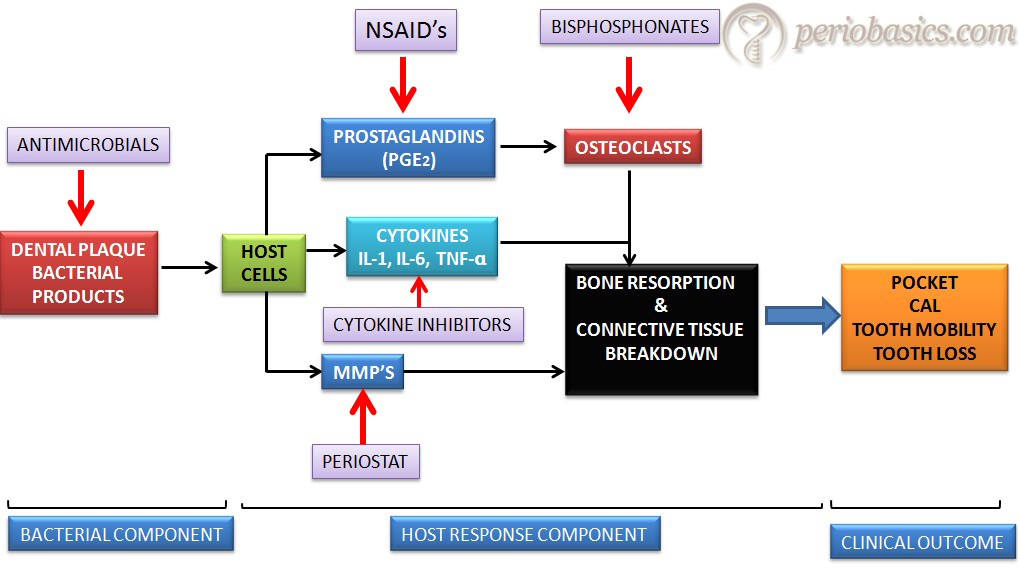
Presently, the models of periodontal disease progression 5, 6 suggest that a major component of connective tissue destruction associated with periodontal disease is the result of activation of the host’s immuno-inflammatory response to the bacterial challenge. The underlying biological mechanisms of this response are characterized by the expression of endothelial cell and intercellular adhesion molecules and by the production of host-derived inflammatory mediators, including, cytokines and lipids by neutrophils, monocytes, lymphocytes and fibroblasts.
Know More…
Perioceutics:
“Perioceutics” is a pharmaceutical field which deals with the development of drugs and medicine for the management and treatment of periodontal diseases. The term perioceutic (periodontal + therapeutic) was first introduced by Heska Corporation (Fort Collins, CO). In 1998, this corporation filed to protect the “perioceutic” trademark for labeling periodontal therapeutic gels, especially for use in the veterinary field, but in 2000 this trademark was abandoned. However, this term is currently being used to address the pharmacotherapeutic agents specifically developed to better manage periodontitis. These pharmacotherapeutic agents include antimicrobial and host response modulation agents.
Balance between pro- and anti-inflammatory mediators in periodontal health and disease
The balance between inflammatory mediators and their counter-regulatory molecules is crucial for determining the outcome of the immuno-inflammatory pathology of periodontal diseases. In the case of stable gingivitis lesion, the pro- and anti-inflammatory response is supposed to be in balance, whereas the response is skewed towards the predominance of pro-inflammatory reactivity in progressive periodontitis lesion. In the context of tissue destruction, cytokines such as interleukin (IL)-1, IL-6 and IL-18 are likely to be important, as are their regulating cytokines IL-10 and IL-11.
As present data suggest that periodontal diseases have got a multi-factorial etiology, the risk factors are equally important in the final outcome of the disease progression. The following figure describes the balance between the various factors favoring periodontal health and disease.

Host modulation therapeutic agents
Before we go through the therapeutic agents used in host modulation, let us first try to understand the steps where these agents modulate the host response. The following figure demonstrates various steps where therapeutic agents modulate the host response and thus the final outcome of the periodontal disease progression.
Classification of host modulation therapeutics
1. Modulation of the immune response,
i. Pro-inflammatory cytokine inhibition.
ii. Modulation of matrix metalloproteinase (MMP) activities.
2. Modulation of arachidonic acid metabolites,
i. Nonsteroidal anti-inflammatory drugs.
ii. Lipoxins, resolvins and protectins.
3. Modulation of bone remodeling,
i. Anti-Inflammatory agents.
ii. Bisphosphonates.
iii. Chemically modified tetracyclines.
iv. Hormone replacement therapy for post-menopause women.
4. Host modulation by promoting periodontal regeneration.
5. Modulation of nitric oxide synthase (NOS) activity.
6. Modulation of cell signaling pathways in periodontal diseases.
7. Recombinant anti-inflammatory cytokine administration.
Modulation of the immune response
Pro-inflammatory cytokine inhibition:
Many studies have indicated that the biological activity of a variety of cytokines may be directly relevant to periodontal destruction 7, 8. IL-1, IL-6, and tumor necrosis factor (TNF) have all been found to be significantly elevated in diseased periodontal sites as compared to healthy or inactive sites 9-12. Cytokines have a synergistic effect. Acting together, pro-inflammatory cytokines amplify the inflammatory condition. For example, IL-1β has synergistic activity with TNF-α or lymphotoxin in stimulating bone resorption 13. Blocking TNF-α has been proven to inhibit osteoclast formation effectively 14. As already explained ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
Pentoxifylline (PTX) is a methylxanthine derivative which blocks the synthesis of TNF-α by inhibiting gene transcription, thereby reducing the accumulation of TNF-α mRNA. The protective effect of PTX could be explained by its capacity to inhibit the production of inflammatory cytokines or to stimulate anti-inflammatory cytokine production 18. Recombinant human IL-11, which inhibits production of TNF-α, IL-1, and NO 19-20 was used in a study which showed reduced disease progression in a ligature-induced periodontitis canine model 21.
Along with this, anti-cytokine antibodies can also be used to block the activity of pro-inflammatory cytokines. Few anti-cytokine antibodies that are commercially available include,
TNF-α : Certolizumab pegol, Adalimumab, Golimumab, etc.
IL-6: Tocilizumab.
IL-15: AMG471.
IL-12 and IL-23: Ustekinumab.
IL-17: AIN457.
Modulation of matrix metalloproteinase (MMP) activities:
The activity of MMPs can be modulated by various ways which include, modulation of the production of MMPs, blocking activation of the proenzyme, blocking the activity of the enzyme, and activating MMP inhibitors 22. The MMPs are a family of zinc- and calcium-dependent endopeptidases secreted or released by a variety of infiltrating cells (i.e., neutrophils and macrophages) and resident cells (i.e., fibroblasts, epithelial cells, osteoblasts, and osteoclasts) found in the periodontium 23. MMPs include collagenases, gelatinases, and metalloelastases. MMPs have been strongly associated with periodontitis 24-28, and excellent reviews have been published discussing the role of MMPs in periodontal diseases 22, 29-31. For more details please read “Matrix metalloproteinases and their role in periodontal diseases”.
While experimenting on germ-free diabetic rats Golub et al. (1983, 1994) 32, 33 discovered the anti-collagenase activity of tetracyclines. Ten different chemically modified tetracyclines (CMTs) have been developed, 9 of which inhibit MMPs and do not possess antimicrobial properties 23. In further studies using these different tetracyclines, Golub et al 34 (1985) reported that the semisynthetic compounds (i.e., doxycycline) were more effective than tetracycline in reducing excessive collagenase activity in the GCF of adult periodontitis patients. Recent clinical trials have focused on doxycycline because it was found to be a more effective inhibitor of collagenase than minocycline or tetracycline 33, 35 and also because of its safety profile, pharmacokinetic properties, and systemic absorption. Presently, host modulation therapy utilizing tetracyclines has primarily involved the use of a reduced dose of doxycycline (20 mg bid).
Know More…
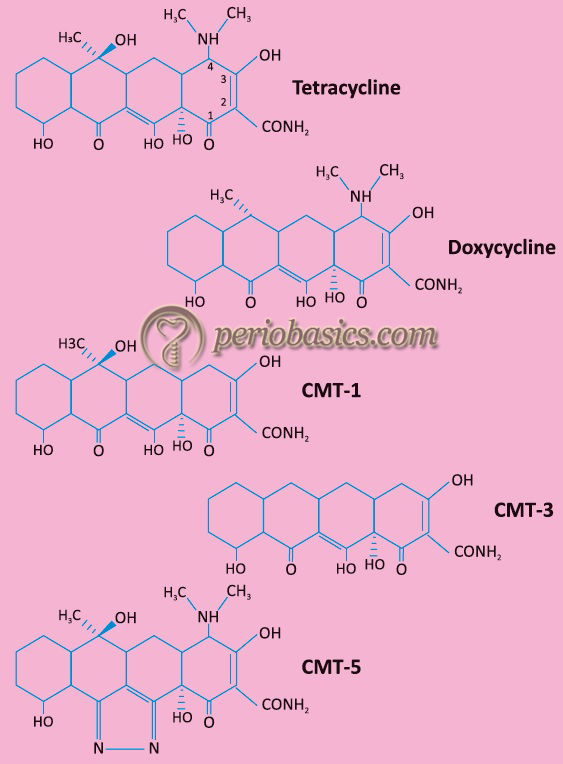
Chemically modified tetracyclines:
The chemically modified tetracyclines (CMTs) have been rationally designed to inhibit the activity of MMPs. Carbon 4 position side chain is responsible for the antimicrobial activity of tetracyclines. CMTs were produced by removing the dimethylamino group from the carbon-4 position of the A ring of the four-ringed (A, B, C, D) structure. The resulting compound, 4-dedimethylamino tetracycline (CMT-1) did not have antimicrobial property, but the anti-collagenase activity was retained both in vitro and in vivo. With the further substitution of functional groups, other CMTs have been developed. As already stated, at present we have 10 CMTs, 9 out of which inhibit MMPs and do not possess antimicrobial properties. The chemical formulas of some of these are,
CMT-1 (4-dedimethylaminotetracycline)
CMT-2 (tetracyclinonitrite)
CMT-3 (6-deoxy-6-demethyl-4-dedimethylamino tetracycline)
CMT-4 (7-chloro-4-de-dimethylamino tetracycline)
CMT-5 (tetracycline pyrrazole)
CMT-6 (4-dedimethylamino. 4-hydroxytetracycline)
CMT-7 (12-deoxy-4-de-dimethyamino tetracycline)
CMT-8 (4-dedimethylaminodoxycycline) have been developed.
The anti-collagenase property of the CMTs is attributed to Ca +2 and Zn +2 -binding sites at the carbonyl oxygen and hydroxyl group of c-11 and c-12 positions. Along with inhibiting MMPs, CMTs inhibit bone resorption and osteoclastic activity, inhibit cartilage degradation, inhibit cell invasion, migration and proliferation and also induce apoptosis. The chemical structure of tetracycline, doxycycline, CMT-1, CMT-3 and CMT-5 is as follows,……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
Periostat:
Periostat is a formulation containing a sub-antimicrobial dose of Doxycycline (SDD) (Doxycycline Hyclate 20 mg; Periostat, CollaGenex, Pharmaceuticals Newton PA) which is FDA approved and ADA accepted in 1998. It is indicated as an adjunct to scaling and root planning (SRP) taken twice daily for a period of 3-9 months in the treatment of chronic periodontitis. 20 mg dose of Doxycycline has been reported not to exhibit antimicrobial effects, but can effectively lower MMP levels 36. Various effects of sub-antimicrobial dose of Doxycycline on host response have been enumerated in the following table,
| Effect of doxycycline on host response |
|---|
| Direct inhibition of active MMPs by cation chelation (dependent upon Ca2+- and Zn2+-binding properties). |
| Inhibits oxidative activation of latent MMPs (independent of cation-binding properties). |
| Down-regulates the expression of key inflammatory cytokines (interleukin-1, interleukin-6, and tumor necrosis factor-α) and prostaglandin E2. |
| Scavenges and inhibits the production of reactive oxygen species produced by neutrophils. |
| Inhibits MMPs and reactive oxygen species, thereby protecting α 1-proteinase inhibitor, and thus indirectly reducing tissue proteinase activity. |
| Stimulates fibroblast collagen production. |
| Reduces osteoclast activity and bone resorption. |
| Inhibits osteoclast MMPs. |
A lot of research work has been done on SDD. Studies done on the gingival crevicular fluid found an increase in the level of transforming growth factor-β1 in the adjunctive low-dose doxycycline test group as compared to the control group, which received only scaling and root planing (SRP) and a placebo 38-40. A combination of low-dose doxycycline and NSAIDs has been found to suppress MMP activity more than low-dose doxycycline alone 41. A meta-analysis 42 of 6 selected clinical studies comparing long-term systemic SDD (20 mg bid doxycycline) to a placebo control in periodontal patients showed a statistically significant adjunctive benefit of SDD + SRP on clinical attachment levels and probing depth, in both 4 to 6 mm and ≥ 7 mm pocket depth categories. Bleeding on probing was ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..

Modulation of arachidonic acid metabolites
Nonsteroidal anti-inflammatory Drugs:
The fact that NSAIDs can suppress alveolar bone resorption suggests that the synthesis of arachidonic acid metabolites may represent a critical regulatory pathway for potentially blocking periodontal disease progression activity 44. In arachidonic acid metabolism, the cyclooxygenase pathway produces prostaglandins, prostacyclin, and thromboxane, called prostanoids. Some prostanoids have pro-inflammatory properties and have been associated with the destructive process in the inflammatory diseases. In periodontal diseases, Prostaglandin E2 (PGE2) has been extensively correlated to inflammation and bone resorption 5. Multiple NSAIDs, inclu-ding indomethacin 45, flurbiprofen 46, ibuprofen 47, naproxen 48, meclofenamic acid 49, and piroxicam 50 have demonstrated the ability to inhibit gingivitis 50 and progression of periodontitis in both ligature-induced 45, 51 and naturally occurring periodontal disease in animal models 46- 48 ………. Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Lipoxins and resolvins:
Bacteria and their products like lipopolysaccharides (LPS) initiate an inflammatory response when they are countered by the protective host response. Many mediators produced by arachidonic acid pathway, including prostanoids, leukotrienes, and related compounds, play important roles in the initiation and progression of inflammation and are thus termed as “pro-inflammatory mediators” 52, 53. In addition to the pro-inflammatory mediators, “anti-inflammatory mediators” are also produced during these interactions. These include lipoxins, aspirin-triggered 15-epi-lipoxins (ATLs), resolvins, docosatrienes, and neuroprotectins. Lipoxins are trihydroxy tetraene-containing eicosanoids that are generated within the vascular lumen during platelet-leukocyte interactions and at mucosal surfaces via leukocyte-epithelial cell interactions 54. The role of the neutrophils in lipoxin generation is crucial. It has been shown that primed neutrophils are another source of lipoxin biosynthesis 55. Lipoxin A (LXA4) gives potent ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..

Protectins:
The protectins are the product of the lipoxygenase-mediated pathway. The endogenous docosahexaenoic acid (DHA) is converted into protectins. The pathway converts DHA into a 17S-hydroxyperoxide containing intermediate that is taken up by leukocytes and converted into 10,17-diHDHA, known as protectin D1 or neuroprotectin (when produced by neural tissues). The name, “neuroprotectin” has been given to them because of their protective actions observed in neural tissues and within the immune system. The capability of protectins in the modulation of host response in periodontal diseases is still under investigation.
As lipoxins, resolvins and protectins are a new class of endogenous mediators that are anti-inflammatory or serve for the “pro-resolution” of inflammation, research work is going on in this field to explore the future possibilities of their clinical use.
Modulation of bone remodeling
Anti-inflammatory agents:
Arachidonic acid metabolites are pro-inflammatory mediators that have been implicated in a variety of bone resorptive processes including chronic periodontitis 56. These mediators can be inhibited by NSAIDs, which include various drugs such as aspirin, ibuprofen, ketorolac, flurbiprofen, naproxen, etc. They inhibit the enzyme cyclooxygenase, thereby preventing the production of arachidonic acid metabolites which are involved in bone resorption.
Bisphosphonates:
Periodontitis is characterized by the alveolar bone loss. One of the therapeutic modality of host modulation is to stop the alveolar bone resorption. Bisphosphonates are widely used in the management of systemic metabolic bone disorders such as osteoporosis and Paget’s disease. They have a ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
Chemical structure:
Chemically bisphosphonates are pyrophosphate analogs characterized by two C-P bonds. They are identified by a common ending in their generic names (“……….. dronate”). These drugs can be subdivided into the nitrogen-containing bisphosphonates and non-nitrogen-containing bisphosphonates 58. Small changes in the structure of the bisphosphonates can lead to extensive alterations in their physicochemical, biological, therapeutic, and toxicological characteristics.

Generations of bisphosphonates:
Bisphosphonates are classified into three generations according to the R1 and R2 groups present in their chemical structure.
| 1st Generation (Non-Nitrogen containing) | 2nd Generation (R2 group contains nitrogen in form of a primary amino group) | 3rd Generation (R2 group contains nitrogen but within a heterocyclic group) |
|---|---|---|
| Etidronate Clodronate | Alendronate Pamidronate (100-1000 times more potent than the 1st generation) | Risedronate Ibandronate Zoledronic Acid (10,000- 100,000 times more potent than the 1st generation) |
Physicochemical effects:
Bisphosphonates work by inhibiting the precipitation of calcium phosphate even at very low concentration 59. They also slow down the dissolution of these crystals 60. All these effects appear to be related to the marked affinity of these compounds for the solid-phase calcium phosphate to which they bind 61. These compounds inhibit osteoclastic activity by blocking acidification by local release and represent a class of chemical structures related to pyrophosphates 62. They also down-regulate levels of several MMPs including MMP-3, MMP-8, and MMP-13 from human periodontal ligament cells 63. The effects of bisphosphonates at tissue level, cellular level, and molecular level are summarized in the following table,
| Tissue Level | Cellular Level | Molecular Level |
|---|---|---|
| ↓sed Bone turnover due to ↓sed Bone resorption. ↓sed Number of new bone multicellular units. Net positive whole body bone balance | ↓sed Osteoclast recruitment. ↑sed Osteoclast apoptosis. ↓sed Osteoclast adhesion. ↓sed Depth of resorption site. ↓sed Release of cytokines by macrophages. ↑sed Osteoblast differentiation and number. | Inhibit mevalonate pathway (that result in perturbed cell activity and induction of apoptosis). ↓sed Post-translational prenylation of GTP- binding proteins. |
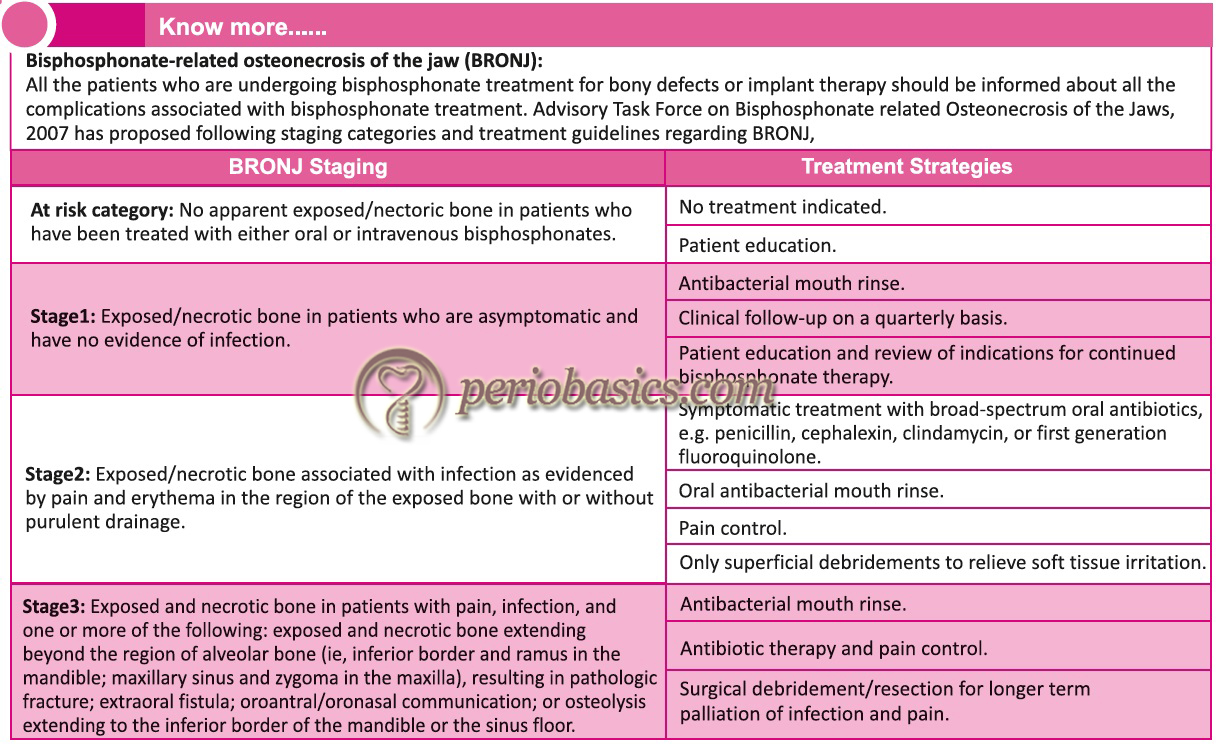
Adverse effects:
A serious adverse effect of bisphosphonates that has substantial dental implications is osteonecrosis of the jaws (see know more box); other bones in the skeleton do not appear to be involved 64. Good dental hygiene reduces the risk of osteonecrosis.
Recent research:
A lot of research work has been done on bisphosphonates and periodontitis. Sodium alendronate treatment in experimental periodontitis in Wistar rats was studied and the results showed that sodium alendronate preserves alveolar bone resorption and has anti-inflammatory and antibacterial activities in experimental periodontitis 65. MMP Inhibition and down-regulation by bisphosphonates has also been demonstrated in one study, which observed the inhibition of MMP-1, -2, -3, -7, -8, -9, -12, -13, and -14 by clodronate, alendronate, pamidro-nate, zoledronate, and inordinate 66.
A study was done to investigate the effects of oral alendronate treatment on radiological and clinical measurements of periodontal disease in postmenopausal women without hormone replacement therapy. Results demonstrated that alendronate treatment improved the perio-dontal status and bone turnover in postmenopausal women 67.
Recent studies have demonstrated that osseointegration of titanium implants can be significantly reinforced with a nanostructure treated with anodic oxidation and ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
Chemically modified tetracyclines (CMTs):
As it is well established that CMTs inhibit the MMPs, so are indirectly involved in inhibition of bone resorption in periodontal diseases.
Hormone replacement therapy for post-menopause women:
The endocrine system plays an important role in the homeostasis of the periodontium 69. Osteoporosis, which is defined as a systemic condition characterized by a decrease in the bone mineral density by at least 2.5 times the normal value in a healthy young female, is a major health problem in postmenopausal women 70. It is a major cause of morbidity and mortality in post-menopause women. The research work clearly indicates that low estrogen production after menopause is associated with increased production of IL-1, IL-6, IL-8, IL-10, TNF-α, granulocyte colony-stimulating factor, and granulocyte-macrophage-colony-stimulating factor, which stimulates mature osteoclasts, modulates bone cell proliferation and induces resorption of both skeletal and alveolar bone 71, 72. The American Academy of Periodontology considers osteoporosis to be a risk factor for periodontal disease 73.
Clinical changes in the periodontal tissues during menopause and post-menopause:
- Reduction in epithelial keratinization 74.
- A reduction in salivary gland flow 75.
- Drying of the oral tissues 76.
- Redness and abnormal paleness of the gingival tissues 76.
- Bleeding on probing and brushing 76.
- Taste sensation may change, causing frequent complaints of a metallic taste 77.
Radiographic changes in the periodontal tissues during menopause and post-menopause:
- Reduced bone mineral content in the jaws 78, 79.
Hormone replacement therapy (HRT) is used to relieve these symptoms and improve the quality of life of peri- or post-menopausal women 80, 81. Many studies have suggested that using HRT in post-menopausal women can decrease the periodontal destruction 79, 82 and increase tooth retention 83.
Effects of HRT on the periodontal tissues:
- Protection against tooth loss 83.
- Reduction in gingival bleeding 84.
- Reduction in the risk of edentulism 85.
Host modulation by promoting periodontal regeneration
Root surface conditioning, growth factors, and cytokines can be used to promote periodontal regeneration. Growth factors and hormones, including platelet-rich plasma (PRP), bone morphogenic proteins (BMPs), platelet-derived growth factor (PDGF), parathyroid hormone (PTH), and enamel matrix derivatives (EMD) have shown promise in enhancing regeneration, although their long-term predictability remains questionable, and their anticipated benefits are moderate 86, 87. In 1976, Melcher 88 presented the concept of “compartmentalization,” in which the connective tissues of the periodontium were divided into four compartments: the lamina propria of the gingiva (gingival corium), the periodontal ligament (PDL), the cementum, and the alveolar bone. Since then a lot of research has been done on periodontal regeneration. Regeneration has been broadly divided into two categories; graft associated and non-graft associated. For details, read “History of periodontal regenerative therapy”.
Modulation of nitric oxide synthase (NOS) activity
Nitric oxide (NO) is a free radical involved in host defense that can be toxic when present in high concentrations and it has been implicated in a variety of inflammatory conditions. NO is produced by a wide variety of cells and appears to be an important regulator of various physiologic processes in both animals and humans 89. NO imbalances have been noted in a variety of chronic infectious and inflammatory conditions, including, periodontal disease 90-92.
NO is generated within biologic tissues via the enzymatic conversion of L-arginine to L-citrulline by NOS. Nitric oxide synthase (NOS) exists in the body in three distinct isoforms: neuronal (nNOS or NOS-I), inducible (iNOS or NOS-II) and endothelial NOS (eNOS or NOS-III) 93. NO has a critical role in the regulation of vascular tone, smooth muscle proliferation, angiogenesis, coagulation, mitochondrial energy generation, neurotransmission, immunity, cell survival, and ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
The role of NO in periodontal diseases has been well investigated. LPS and other antigenic substances from putative periodontal pathogens such as Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Prevotella intermedia, Prevotella nigrescens, and Fusobacterium nucleatum have been shown to induce the iNOS expression and NO production in murine macrophages 101-104. It has been demonstrated that iNOS expression and activity is induced in gingival fibroblasts and neutrophils, following the stimulation by periodontal pathogens, cytokines, and other inflammatory mediators 105. Along with this, neutrophils isolated from localized Grade C (aggressive) periodontitis patients were shown to display increased iNOS activity and subsequent chemotactic defects 106. Inhibition of NOS can be beneficial in the modulation of periodontal disease by preventing the participation of NO and other reactive nitrogen species in a variety of pathways which are thought to be deleterious to the host 107.
There are two kinds of NOS inhibitors; non-selective and selective. Non-selective inhibitors of NOS are not specific to any kind of NOS whereas, selective are specific. The alkyl guanidines are a ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Modulation of cell signaling pathways in periodontal diseases
As we know that bacterial biofilm present in the gingival sulcus around the tooth is a source of various bacterial components and products, which initiate the host response. First of all the innate immune system counters the infection, but when not controlled, the acquired immune system is activated. The invader is recognized by the antigen-presenting cells and presented to T-cells by MHC-I or MHC-II, depending on which helper or cytotoxic-T-cell mediated immune response is generated. Within 3-4 days a robust inflammatory response is generated, which initiates the connective tissue destruction. This activation is done by various cellular signaling mechanisms, which lead to the synthesis of various cytokines and other inflammatory chemical mediators.
When a signal is generated, it travels through the cytoplasm and reaches the nucleus, and ultimately the pattern of gene expression is altered by transcriptional and post-transcriptional mechanisms. Signal transduction depends on receptor-ligand interactions, which usually involves some modification on the cytoplasmic proteins associated with these receptors. The most common modification associated with signal transduction is phosphorylation of specific amino acid residues by kinases, which induces a conformational change in the tri-dimensional structure of the protein. In the process of intracellular signaling, energy is transferred at every step which modulates the biological activity of the proteins involved. In periodontal disease, the most important pathways include the mitogen-activated protein kinase (MAPK), nuclear factor kappa B (NF-κB) and Janus tyrosine kinase-signal transducer and activator of transcription (JAK/STAT) 110, 111.
MAPK pathway
The MAP kinases are a large family of protein kinases which are involved in cellular signaling pathways in various biological processes. These are involved in signal transduction of extracellular hormones, growth factors, and cytokines 112, 113. MAPKs are further divided into three classes: extracellular-regulated kinases (ERK-1/-2), c-Jun N-terminal activated kinases (JNK), and p38. During inflammation, MAPK pathways (particularly, p38) are involved in the increased expression of various cytokine genes by modulation of both transcriptional and post-transcriptional mechanisms. Studies have demonstrated that inhibition of JNK and ERK pathways may effectively inhibit the production of pro-inflammatory mediators 114, 115. Furthermore, the MAPK inhibitors have been shown to be capable of reducing inflammation in inflammatory conditions like rheumatoid arthritis and periodontal disease 116-119.
Studies have shown that ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
NF-κB pathway
The NF-κB is a family of transcription factors involved in various signal transduction pathways that participate both in adaptive and innate immune responses. The NF-κB family consists of five members: REL-a (p65), NF-κB1 (p50; p105), NF-κB2 (p52; p100), c-REL and REL-b 122. The NF-κB pathway is activated when a large number of pro-inflammatory mediators, such as bacterial LPS, TNF-α, IL-1, MMPs, COX2 and inducible nitric oxide synthase (iNOS) are present in tissue 123, 124. It has been demonstrated that periodontal pathogens like P. gingivalis and others also activate NF-κB in periodontal tissues 125.
As already stated, the NF-κB family consists of five members. Except for REL-b, all other members join to form homodimers or heterodimers to produce NF-κB transcription factors. During inflammatory reactions, the most common heterodimer formed is of p50 and p65. This heterodimer binds to NF-κB at 5′-3′ site to activate or repress target gene transcription 126, 127. The NF-κB is also involved in the TRL activation pathway. Agents that prevent degradation of NF-κB inhibitors have been investigated to inhibit the NF-κB pathway 128. However, these strategies are still under investigation to be used clinically.
JAK/STAT pathway
The JAK/STAT pathway is involved in signal transduction of interleukins, interferons, epidermal growth factor, growth hormone, erythropoietin and other mediators 129. In periodontitis, this pathway is the major mechanism of signal transduction for cytokines, including IFN-γ, TNF-α, IL-1 IL-4, IL-6, and IL-10 120, 130, 131. Cytokines and interferons exert their role in the regulation of immune response by activating the enzymes, JAK or Janus kinases. These enzymes are associated with the cytoplasmic portion of the transmembrane receptors 132. They further activate proteins known as STATs (STAT1-4, 5a, 5b, and 6) in the ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
Recombinant anti-inflammatory cytokine administration
IL-11 has anti-inflammatory action which can be utilized in host modulation therapy. IL-11 has been shown to attenuate IL-1 and TNF synthesis from macrophages by up-regulating inhibitory NF-kB synthesis in monocyte/macrophage cell lines. Inhibitory NF- kB prevents NF- kB from translocating to the nucleus where NF- kB functions as a transcriptional activator for the proinflammatory cytokines. IL-11 has also been shown to inhibit the synthesis of IFN-γ and IL-2 by CD41 T-cells. Martuscelli et al. (2000) 136 demonstrated that subcutaneous injections of recombinant human IL-11 (rh IL-11) were able to slow the progression of attachment and radiographic alveolar bone loss in a ligature-induced beagle dog model. These observations support the use of rhIL-11 as host modulation agent for the treatment of periodontal diseases. However, more clinical research, especially on humans is required to authenticate their clinical efficacy.
Newer strategies in host modulation therapy
Aspirin-triggered epimeric forms from DHA:
It is a recently discovered aspirin-triggered docosahexaenoic acid (DHA) metabolome that biosynthesizes a potent product in inflammatory exudates and human leukocytes, namely aspirin-triggered Neuroprotectin D1/Protectin D1 [AT-(NPD1/PD1)]. This metabolome has been shown to have a positive interaction with CB2 and peroxisome proliferator-activated receptor (PPAR) family receptors. The primary function of protectins is to reduce PMN transmigration through the endothelial cells and enhance clearance (efferocytosis) of apoptotic PMN by human macrophages 137.
Glucocorticoid-induced Annexin-A1:
Annexin A1 is a protein with multifunctional roles in innate and adaptive immunity mainly devoted to the regulation of inflammatory cells and the resolution of inflammation. It is expressed in the cytoplasm of several peripheral blood cells, mainly in neutrophils, monocytes, macrophages, eosinophils, mast cells, and in minimal amounts in T-cells. Annexin A1 levels in circulating neutrophils are under the control of glucocorticoids (endogenous and exogenous) that involves the Annexin A1 Lipoxin A receptor (ALXR), the glucocorticoid-induced leucine zipper gene (GILZ) 138. It resolves inflammation by inhibiting transmigration and recruitment of PMNs cells at the inflammatory site 139. Another important function of Annexin A1 is to act as a ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
Polyenolic zinc-binding compounds (PEZBINs):
These compounds have been developed to inhibit MMPs and cytokines in periodontal and other collagen-destructive and inflammatory diseases. These agents have been approved for systemic administration to patients with chronic inflammatory periodontal and skin diseases, but in higher doses can produce side-effects. Some examples of these agents include bi-phenolic 1,3-diketo analogs (e.g. bis-aroyl methanes) and chemically-modified curcumins (e.g. methoxycarbonyl curcumin). Curcumin has received attention because of its anti-inflammatory properties. Its anti-inflammatory effects have been demonstrated in periodontal disease, cardiovascular diseases, cancer, arthritis, and diabetes 141. To clinically use the beneficial effects of curcumin, a newer class of drugs has been developed referred to as, “chemically modified curcumins (CMCs)”. These agents have improved ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Semisynthetic glycosaminoglycan ether (SAGE):
The semisynthetic glycosaminoglycan ethers are a novel family of sulfated and metabolically stabilized anionic polysaccharide derivatives. These agents have been shown to have the ability to reduce local and systemic inflammation. These agents have been shown to have the ability to suppress inflammation in high-risk individuals such as smokers and those with diabetes. Their mechanism of action is based on their ability to reduce the impact of advanced glycation end products (AGEs), thus, reducing the proinflammatory mediators of disease 143. In a study on diabetic rats, SAGE significantly attenuated the alveolar bone loss 144.
Stem cells in host modulation therapy:
The application of stem cells in periodontal regeneration is being extensively studied presently. These cells are self-renewable and can differentiate into a variety of cell types that form mesenchymal and connective tissues. These cells have the capability to differentiate into different types of cells present in the periodontium and thus can regenerate the lost tissue. A detailed description of the stem cells has been given in, “Tissue engineering in periodontics”.
Limitations of host modulation therapy
In the above discussion, we studied various therapeutic modalities which have been investigated and used for host response modulation. However, presently there are many limitations of HMT. The first limitation is regarding the duration of therapy. For most of the host modulation agents, the duration for which these can be safely given is not well established. For SDD, twice daily administration as an adjunct for the treatment of chronic periodontitis both in short term duration (1 – 3 months) and longer duration (up to 9 months) has showed more improved and predictable treatment outcomes without the emergence of adverse effects of doxycycline and any alterations in the subgingival microflora 145. However, for many other ……… Contents available in the book………….. Contents available in the book……… Contents available in the book……… Contents available in the book……… Contents available in the book…..
The newer host modulation agents such as cytokine inhibitors, human recombinant anti-inflammatory cytokines, docosahexaenoic acid metabolites, PEZBINs, SAGE and stem cell therapy are still in their infancy and require more research on human model to find out their efficacy. Along with this, we also need to make these terapeutic agents economically viable for clinical use.
Conclusion
The initiation and progression of periodontal diseases are the result of interactions between periodontopathogenic microorganisms and host response. In some clinical situations (systemically compromised patient, smokers, genetically predisposed patients), the conventional periodontal therapy does not always achieve the desired clinical outcome. Furthermore, cases which are refractory to conventional treatment and patients in whom surgical approach is not possible because of medical risk factors or age, the host modulation therapy is desirable along with the conventional anti-biofilm therapy. However, on many of the host modulation agents, long-term clinical trials still need to be done to authenticate their efficacious, safe and long term use on patients.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

